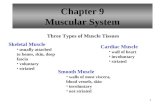
Cardiac Muscle Found only in heart Found only in heart Striated Striated Each cell usually has one...
-
date post
18-Dec-2015 -
Category
Documents
-
view
216 -
download
2
Transcript of Cardiac Muscle Found only in heart Found only in heart Striated Striated Each cell usually has one...
Cardiac MuscleCardiac Muscle
Found only in Found only in heartheart StriatedStriated Each cell usually has Each cell usually has one nucleusone nucleus Has intercalated disks and gap junctionsHas intercalated disks and gap junctions AutorhythmicAutorhythmic cells cells Action potentials of longer duration and Action potentials of longer duration and
longer refractory periodlonger refractory period CaCa2+2+ regulates contraction regulates contraction
Cardiac MuscleCardiac Muscle
Elongated, branching cells containing 1-2 centrally located nucleiElongated, branching cells containing 1-2 centrally located nuclei Contains actin and myosin myofilaments Contains actin and myosin myofilaments Intercalated disksIntercalated disks: Specialized cell-cell contacts: Specialized cell-cell contacts Desmosomes hold cells together and gap junctions allow action Desmosomes hold cells together and gap junctions allow action
potentialspotentials Electrically, cardiac muscle behaves as single unitElectrically, cardiac muscle behaves as single unit
Refractory PeriodRefractory Period
AbsoluteAbsolute: Cardiac muscle cell : Cardiac muscle cell completely insensitive to further completely insensitive to further stimulationstimulation
RelativeRelative: Cell exhibits reduced : Cell exhibits reduced sensitivity to additional stimulationsensitivity to additional stimulation
Long refractory period prevents Long refractory period prevents tetanic contractionstetanic contractions
AP-contraction AP-contraction relationship:relationship:
AP in skeletal muscle is AP in skeletal muscle is very short-livedvery short-lived AP is basically over before AP is basically over before
an increase in muscle an increase in muscle tension can be measured.tension can be measured.
AP in cardiac muscle is AP in cardiac muscle is very long-livedvery long-lived AP has an extra AP has an extra
component, which extends component, which extends the duration.the duration.
The contraction is almost The contraction is almost over before the action over before the action potential has finished.potential has finished.
Functions of the HeartFunctions of the Heart Generating Generating bloodblood pressure pressure Routing Routing bloodblood
Heart separates pulmonary and Heart separates pulmonary and systemic circulationssystemic circulations
Ensuring one-way Ensuring one-way bloodblood flow flow Heart valves ensure one-way flowHeart valves ensure one-way flow
Regulating Regulating bloodblood supply supply Changes in contraction rate and Changes in contraction rate and
force match blood delivery to force match blood delivery to changing metabolic needschanging metabolic needs
Orientation of cardiac Orientation of cardiac muscle fibres:muscle fibres:
Unlike skeletal Unlike skeletal muscles, cardiac muscles, cardiac muscles have to muscles have to contract in more than contract in more than one direction.one direction.
Cardiac muscle cells Cardiac muscle cells are striated, meaning are striated, meaning they will only contract they will only contract along their long axis.along their long axis.
In order to get In order to get contraction in two contraction in two axis, the fibres wrap axis, the fibres wrap around.around.
Heart WallHeart Wall
Three layers of tissueThree layers of tissue EpicardiumEpicardium: This serous membrane : This serous membrane
of smooth outer surface of heartof smooth outer surface of heart MyocardiumMyocardium: Middle layer composed : Middle layer composed
of cardiac muscle cell and of cardiac muscle cell and responsibility for heart contractingresponsibility for heart contracting
EndocardiumEndocardium: Smooth inner surface : Smooth inner surface of heart chambersof heart chambers
Heart SoundsHeart Sounds
First heart sound or “lubb”First heart sound or “lubb” Atrioventricular valves and surrounding fluid Atrioventricular valves and surrounding fluid
vibrations as valves close at beginning of vibrations as valves close at beginning of ventricular systoleventricular systole
Second heart sound or “dupp”Second heart sound or “dupp” Results from closure of aortic and pulmonary Results from closure of aortic and pulmonary
semilunar valves at beginning of ventricular semilunar valves at beginning of ventricular diastole, lasts longerdiastole, lasts longer
Third heart sound Third heart sound (occasional)(occasional) Caused by turbulent blood flow into ventricles and Caused by turbulent blood flow into ventricles and
detected near end of first one-third of diastoledetected near end of first one-third of diastole
Cardiac ArrhythmiasCardiac Arrhythmias
TachycardiaTachycardia: Heart rate in excess of : Heart rate in excess of 100bpm100bpm
BradycardiaBradycardia: Heart rate less than 60 : Heart rate less than 60 bpmbpm
Sinus arrhythmiaSinus arrhythmia: Heart rate varies 5% : Heart rate varies 5% during respiratory cycle and up to 30% during respiratory cycle and up to 30% during deep respirationduring deep respiration
Premature atrial contractionsPremature atrial contractions: : Occasional shortened intervals between Occasional shortened intervals between one contraction and succeeding, one contraction and succeeding, frequently occurs in healthy peoplefrequently occurs in healthy people
Cardiac CycleCardiac Cycle
Heart is two pumps that work Heart is two pumps that work together, right and left halftogether, right and left half
Repetitive contraction (Repetitive contraction (systolesystole) and ) and relaxation (relaxation (diastolediastole) of heart chambers) of heart chambers
Blood moves through circulatory Blood moves through circulatory system from areas of higher to lower system from areas of higher to lower pressure.pressure. Contraction of heart produces the Contraction of heart produces the
pressurepressure
Mean Arterial Pressure Mean Arterial Pressure (MAP)(MAP)
Average blood pressure in aortaAverage blood pressure in aorta MAP=CO x PRMAP=CO x PR
CO is amount of blood pumped by heart CO is amount of blood pumped by heart per minuteper minute CO=SV x HRCO=SV x HR
SVSV: Stroke volume of blood pumped during each : Stroke volume of blood pumped during each heart beatheart beat
HRHR: Heart rate or number of times heart beats per : Heart rate or number of times heart beats per minuteminute
Cardiac reserve: Difference between CO at Cardiac reserve: Difference between CO at rest and maximum COrest and maximum CO
PR is total resistance against which PR is total resistance against which blood must be pumpedblood must be pumped
Regulation of the HeartRegulation of the Heart Intrinsic regulationIntrinsic regulation: Results from : Results from
normal functional characteristics, not normal functional characteristics, not on neural or hormonal regulationon neural or hormonal regulation Starling’s law of the heartStarling’s law of the heart
Extrinsic regulationExtrinsic regulation: Involves neural : Involves neural and hormonal controland hormonal control Parasympathetic stimulationParasympathetic stimulation
Supplied by vagus nerve, decreases heart rate, Supplied by vagus nerve, decreases heart rate, acetylcholine secretedacetylcholine secreted
Sympathetic stimulationSympathetic stimulation Supplied by cardiac nerves, increases heart rate Supplied by cardiac nerves, increases heart rate
and force of contraction, epinephrine and and force of contraction, epinephrine and norepinephrine releasednorepinephrine released
Heart HomeostasisHeart Homeostasis Effect of blood pressureEffect of blood pressure
Baroreceptors monitor blood pressureBaroreceptors monitor blood pressure Effect of pH, carbon dioxide, oxygenEffect of pH, carbon dioxide, oxygen
Chemoreceptors monitorChemoreceptors monitor Effect of extracellular ion concentrationEffect of extracellular ion concentration
Increase or decrease in extracellular KIncrease or decrease in extracellular K++ decreases heart ratedecreases heart rate
Effect of body temperatureEffect of body temperature Heart rate increases when body temperature Heart rate increases when body temperature
increases, heart rate decreases when body increases, heart rate decreases when body temperature decreasestemperature decreases
Pacemaker regulation:Pacemaker regulation:
Once the pacemaker cells reach threshold, Once the pacemaker cells reach threshold, the magnitude and duration of the AP is the magnitude and duration of the AP is always the same.always the same.
In order to change the frequency, the time In order to change the frequency, the time between APs must vary.between APs must vary. The interval can only be changed in two ways.The interval can only be changed in two ways.
The rate of depolarization can be changedThe rate of depolarization can be changed The amount of depolarization required to reach The amount of depolarization required to reach
threshold can be changed.threshold can be changed.
Peripheral Circulatory Peripheral Circulatory SystemSystem
Systemic vesselsSystemic vessels Transport blood through most all body Transport blood through most all body
parts from left ventricle and back to right parts from left ventricle and back to right atriumatrium
Pulmonary vesselsPulmonary vessels Transport blood from right ventricle Transport blood from right ventricle
through lungs and back to left atriumthrough lungs and back to left atrium Blood vessels and heart regulated to Blood vessels and heart regulated to
ensure blood pressure is high enough ensure blood pressure is high enough for blood flow to meet metabolic needs for blood flow to meet metabolic needs of tissuesof tissues
Blood Vessel StructureBlood Vessel Structure ArteriesArteries
Elastic, muscular, arteriolesElastic, muscular, arterioles CapillariesCapillaries
Blood flows from arterioles to capillariesBlood flows from arterioles to capillaries Most of exchange between blood and Most of exchange between blood and
interstitial spaces occurs across the wallsinterstitial spaces occurs across the walls Blood flows from capillaries to venous Blood flows from capillaries to venous
systemsystem VeinsVeins
Venules, small veins, medium or large Venules, small veins, medium or large veinsveins
Structure of Arteries Structure of Arteries and Veinsand Veins
Three layers except for Three layers except for capillaries and venulescapillaries and venules
Tunica intima (interna)Tunica intima (interna) EndotheliumEndothelium
Tunica mediaTunica media VasoconstrictionVasoconstriction VasodilationVasodilation
Tunica adventitia Tunica adventitia (externa)(externa) Merges with connective Merges with connective
tissue surrounding blood tissue surrounding blood vesselsvessels
Note mistake on figureNote mistake on figure
Structure of ArteriesStructure of Arteries
Elastic or conducting arteriesElastic or conducting arteries Largest diameters, pressure high and Largest diameters, pressure high and
fluctuatesfluctuates Muscular or medium arteriesMuscular or medium arteries
Smooth muscle allows vessels to regulate Smooth muscle allows vessels to regulate blood supply by constricting or dilatingblood supply by constricting or dilating
ArteriolesArterioles Transport blood from small arteries to Transport blood from small arteries to
capillariescapillaries
Structure of VeinsStructure of Veins Venules and small veinsVenules and small veins
Tubes of endothelium on delicate Tubes of endothelium on delicate basement membranebasement membrane
Medium and large veinsMedium and large veins ValvesValves
Allow blood to flow toward heart but Allow blood to flow toward heart but not in opposite directionnot in opposite direction
Atriovenous anastomosesAtriovenous anastomoses Allow blood to flow from arterioles to Allow blood to flow from arterioles to
small veins without passing through small veins without passing through capillariescapillaries
Capillaries:Capillaries: Capillary wall Capillary wall
consists mostly of consists mostly of endothelial cellsendothelial cells
Types classified by Types classified by diameter/permeabilitydiameter/permeability ContinuousContinuous
Do not have fenestraeDo not have fenestrae FenestratedFenestrated
Have poresHave pores SinusoidalSinusoidal
Large diameter with Large diameter with large fenestraelarge fenestrae
Capillary Network:Capillary Network:
Blood flows from Blood flows from arterioles through arterioles through metarteriolesmetarterioles, then , then through through capillary capillary networknetwork
Venules drain Venules drain networknetwork
Smooth muscle in Smooth muscle in arterioles, arterioles, metarterioles, metarterioles, precapillary precapillary sphincterssphincters regulates regulates blood flowblood flow
Pulmonary CirculationPulmonary Circulation
Moves blood to and from the lungsMoves blood to and from the lungs Pulmonary trunkPulmonary trunk
Arises from right ventricleArises from right ventricle Pulmonary arteriesPulmonary arteries
Branches of pulmonary trunk which Branches of pulmonary trunk which project to lungsproject to lungs
Pulmonary veinsPulmonary veins Exit each lung and enter left atriumExit each lung and enter left atrium
Systemic Circulation: Systemic Circulation: ArteriesArteries
AortaAorta From which all arteries are derived From which all arteries are derived
either directly or indirectlyeither directly or indirectly PartsParts
Ascending, descending, thoracic, abdominalAscending, descending, thoracic, abdominal
Coronary arteriesCoronary arteries Supply the heartSupply the heart
Systemic Circulation: Systemic Circulation: VeinsVeins
Return blood from body to right Return blood from body to right atriumatrium
Major veinsMajor veins Coronary sinus (Coronary sinus (heartheart)) Superior vena cava (Superior vena cava (head, neck, thorax, head, neck, thorax,
upper limbsupper limbs)) Inferior vena cava (Inferior vena cava (abdomen, pelvis, abdomen, pelvis,
lower limbslower limbs)) Types of veinsTypes of veins
Superficial, deep, sinusesSuperficial, deep, sinuses
Dynamics of Blood Dynamics of Blood CirculationCirculation
Interrelationships betweenInterrelationships between PressurePressure FlowFlow ResistanceResistance Control mechanisms that regulate blood Control mechanisms that regulate blood
pressurepressure Blood flow through vesselsBlood flow through vessels
Blood PressureBlood Pressure
Measure of force exerted by blood Measure of force exerted by blood against the wallagainst the wall
Blood moves through vessels Blood moves through vessels because of blood pressurebecause of blood pressure
Measured by listening for Korotkoff Measured by listening for Korotkoff sounds produced by turbulent flow sounds produced by turbulent flow in arteries as pressure released from in arteries as pressure released from blood pressure cuffblood pressure cuff
Pressure and Pressure and ResistanceResistance
Blood pressure Blood pressure averages averages 100 mm 100 mm HgHg in aorta and in aorta and drops to 0 mm Hg drops to 0 mm Hg in the right atriumin the right atrium
Greatest drop in Greatest drop in pressure occurs in pressure occurs in arterioles which arterioles which regulate blood flow regulate blood flow through tissuesthrough tissues
No large No large fluctuations in fluctuations in capillaries and capillaries and veinsveins
Pulse PressurePulse Pressure Difference between Difference between
systolic and systolic and diastolicdiastolic pressures pressures
Increases when Increases when stroke volume stroke volume increases or increases or vascular vascular compliance compliance decreasesdecreases
Pulse pressure can Pulse pressure can be used to take a be used to take a pulse to determine pulse to determine heart rate and heart rate and rhythmicityrhythmicity
Blood Flow, Poiseuille’s Blood Flow, Poiseuille’s LawLaw
and Viscosityand Viscosity Blood flowBlood flow
Amount of blood Amount of blood moving through a moving through a vessel in a given vessel in a given time periodtime period
Directly Directly proportional to proportional to pressure pressure differences, differences, inversely inversely proportional to proportional to resistanceresistance
Poiseuille’s LawPoiseuille’s Law Flow decreases when Flow decreases when
resistance increasesresistance increases Flow resistance Flow resistance
decreases when decreases when vessel diameter vessel diameter increasesincreases
ViscosityViscosity Measure of Measure of
resistance of liquid resistance of liquid to flowto flow
As viscosity As viscosity increases, pressure increases, pressure required to flow required to flow increasesincreases
Critical Closing Critical Closing Pressure, Laplace’s Law Pressure, Laplace’s Law
and Complianceand ComplianceCritical closing Critical closing
pressurepressure Pressure at which a Pressure at which a
blood vessel collapses blood vessel collapses and blood flow stopsand blood flow stops
Laplace’s LawLaplace’s Law Force acting on blood Force acting on blood
vessel wall is vessel wall is proportional to proportional to diameter of the vessel diameter of the vessel times blood pressuretimes blood pressure
Vascular complianceVascular compliance Tendency for blood Tendency for blood
vessel volume to vessel volume to increase as blood increase as blood pressure increasespressure increases
More easily the More easily the vessel wall stretches, vessel wall stretches, the greater its the greater its compliancecompliance
Venous system has a Venous system has a large compliance and large compliance and acts as a blood acts as a blood reservoirreservoir
Physiology of Systemic Physiology of Systemic CirculationCirculation
Determined byDetermined by Anatomy of circulatory systemAnatomy of circulatory system Dynamics of blood flowDynamics of blood flow Regulatory mechanisms that control Regulatory mechanisms that control
heart and blood vesselsheart and blood vessels Blood volumeBlood volume
Most in the veinsMost in the veins Smaller volumes in arteries and Smaller volumes in arteries and
capillariescapillaries
Laminar and Turbulent Laminar and Turbulent FlowFlow
Laminar flowLaminar flow StreamlinedStreamlined Outermost layer Outermost layer
moving slowest and moving slowest and center moving center moving fastestfastest
Turbulent flowTurbulent flow InterruptedInterrupted Rate of flow exceeds Rate of flow exceeds
critical velocitycritical velocity Fluid passes a Fluid passes a
constriction, sharp constriction, sharp turn, rough surfaceturn, rough surface
Aging of the ArteriesAging of the Arteries
ArteriosclerosisArteriosclerosis General term for General term for
degeneration degeneration changes in changes in arteries making arteries making them less elasticthem less elastic
AtherosclerosisAtherosclerosis Deposition of Deposition of
plaque on wallsplaque on walls
Capillary Exchange andCapillary Exchange andInterstitial Fluid Volume Interstitial Fluid Volume
RegulationRegulation
Blood pressure, capillary Blood pressure, capillary permeability, and osmosis affect permeability, and osmosis affect movement of fluid from movement of fluid from capillariescapillaries
A net movement of fluid occurs from A net movement of fluid occurs from blood into tissues. Fluid gained by blood into tissues. Fluid gained by tissues is removed by tissues is removed by lymphatic lymphatic systemsystem..
Vein Characteristics andVein Characteristics andEffect of Gravity on Effect of Gravity on
Blood PressureBlood PressureVein Vein
CharacteristicsCharacteristics Venous return to Venous return to
heart increases heart increases due to increase in due to increase in blood volume, blood volume, venous tone, and venous tone, and arteriole dilationarteriole dilation
Effect of GravityEffect of Gravity In a standing In a standing
position, hydrostatic position, hydrostatic pressure caused by pressure caused by gravity increases gravity increases blood pressure blood pressure below the heart and below the heart and decreases pressure decreases pressure above the heartabove the heart
Control of Blood Flow by Control of Blood Flow by TissuesTissues
Local controlLocal control In most tissues, blood flow is In most tissues, blood flow is
proportional to metabolic needs of proportional to metabolic needs of tissuestissues
Nervous SystemNervous System Responsible for routing blood flow and Responsible for routing blood flow and
maintaining blood pressuremaintaining blood pressure Hormonal ControlHormonal Control
Sympathetic action potentials stimulate Sympathetic action potentials stimulate epinephrine and norepinephrineepinephrine and norepinephrine
Local Control of Blood Flow Local Control of Blood Flow by Tissuesby Tissues
Blood flow can increase 7-8 times as a result of Blood flow can increase 7-8 times as a result of vasodilation of metarterioles and precapillary vasodilation of metarterioles and precapillary sphincters in response to increased rate of metabolismsphincters in response to increased rate of metabolism Vasodilator substances produced as metabolism increasesVasodilator substances produced as metabolism increases Vasomotion is periodic contraction and relaxation of Vasomotion is periodic contraction and relaxation of
precapillary sphinctersprecapillary sphincters
Short-Term Regulation Short-Term Regulation ofof
Blood PressureBlood Pressure Baroreceptor reflexesBaroreceptor reflexes
Change peripheral resistance, heart rate, and Change peripheral resistance, heart rate, and stroke volume in response to changes in blood stroke volume in response to changes in blood pressurepressure
Chemoreceptor reflexesChemoreceptor reflexes Sensory receptors sensitive to oxygen, carbon Sensory receptors sensitive to oxygen, carbon
dioxide, and pH levels of blooddioxide, and pH levels of blood
Central nervous system ischemic Central nervous system ischemic responseresponse Results from high carbon dioxide or low pH levels Results from high carbon dioxide or low pH levels
in medulla and increases peripheral resistancein medulla and increases peripheral resistance
Long-Term Regulation Long-Term Regulation of Blood Pressureof Blood Pressure
Renin-angiotensin-aldosterone Renin-angiotensin-aldosterone mechanismmechanism
Vasopressin (ADH) mechanismVasopressin (ADH) mechanism Atrial natriuretic mechanismAtrial natriuretic mechanism Fluid shift mechanismFluid shift mechanism Stress-relaxation responseStress-relaxation response
Long Term MechanismsLong Term MechanismsWhich Lower Blood Which Lower Blood
VolumeVolume Atrial natriuretic Atrial natriuretic
factorfactor Hormone released Hormone released
from cardiac muscle from cardiac muscle cells when atrial cells when atrial blood pressure blood pressure increases, simulating increases, simulating an increase in an increase in urinary production, urinary production, causing a decrease causing a decrease in blood volume and in blood volume and blood pressureblood pressure
Fluid shiftFluid shift Movement of fluid Movement of fluid
from interstitial from interstitial spaces into spaces into capillaries in capillaries in response to response to decrease in blood decrease in blood pressure to maintain pressure to maintain blood volumeblood volume
Stress-relaxationStress-relaxation Adjustment of blood Adjustment of blood
vessel smooth vessel smooth muscle to respond muscle to respond to change in blood to change in blood volumevolume
ShockShock
Inadequate blood flow throughout bodyInadequate blood flow throughout body Three stagesThree stages
CompensatedCompensated: Blood pressure decreases only a : Blood pressure decreases only a moderate amount and mechanisms able to moderate amount and mechanisms able to reestablish normal blood pressure and flowreestablish normal blood pressure and flow
ProgressiveProgressive: Compensatory mechanisms : Compensatory mechanisms inadequate and positive feedback cycle develops; inadequate and positive feedback cycle develops; cycle proceeds to next stage or medical treatment cycle proceeds to next stage or medical treatment reestablishes adequate blood flow to tissuesreestablishes adequate blood flow to tissues
IrreversibleIrreversible: Leads to death, regardless of medical : Leads to death, regardless of medical treatmenttreatment