Body surface mapping of counterclockwise and clockwise typical ...
Transcript of Body surface mapping of counterclockwise and clockwise typical ...

Body Surface Mapping ofCounterclockwise and Clockwise TypicalAtrial Flutter: A Comparative AnalysisWith Endocardial Activation Sequence MappingArne SippensGroenewegen, MD,*† Michael D. Lesh, MD, FACC,*† Franz X. Roithinger, MD,*†Willard S. Ellis, PHD,*† Paul R. Steiner, MD,* Leslie A. Saxon, MD, FACC,*Randall J. Lee, MD, FACC,*† Melvin M. Scheinman, MD, FACC*San Francisco, California
OBJECTIVES This study was directed at developing spatial 62-lead electrocardiogram (ECG) criteria forclassification of counterclockwise (CCW) and clockwise (CW) typical atrial flutter (Fl) inpatients with and without structural heart disease.
BACKGROUND Electrocardiographic classification of CCW and CW typical atrial Fl is frequently hamperedby inaccurate and inconclusive scalar waveform analysis of the 12-lead ECG.
METHODS Electrocardiogram signals from 62 torso sites and multisite endocardial recordings wereobtained during CCW typical atrial Fl (12 patients), CW typical Fl (3 patients), both formsof typical Fl (4 patients) and CCW typical and atypical atrial Fl (1 patient). All the Fl waveepisodes were divided into two or three successive time periods showing stable potentialdistributions from which integral maps were computed.
RESULTS The initial, intermediate and terminal CCW Fl wave map patterns coincided with: 1)caudocranial activation of the right atrial septum and proximal-to-distal coronary sinusactivation, 2) craniocaudal activation of the right atrial free wall, and 3) activation of thelateral part of the subeustachian isthmus, respectively. The initial, intermediate and terminalCW Fl wave map patterns corresponded with : 1) craniocaudal right atrial septal activation,2) activation of the subeustachian isthmus and proximal-to-distal coronary sinus activation,and 3) caudocranial right atrial free wall activation, respectively. A reference set of typicalCCW and CW mean integral maps of the three successive Fl wave periods was computedafter establishing a high degree of quantitative interpatient integral map pattern correspon-dence irrespective of the presence or absence of organic heart disease.
CONCLUSIONS The 62-lead ECG of CCW and CW typical atrial Fl in man is characterized by astereotypical spatial voltage distribution that can be directly related to the underlyingactivation sequence and is highly specific to the direction of Fl wave rotation. The meanCCW and CW Fl wave integral maps present a unique reference set for improved clinicaldetection and classification of typical atrial Fl. (J Am Coll Cardiol 2000;35:1276–87) ©2000 by the American College of Cardiology
Clinical electrocardiography of typical atrial flutter (Fl)dates back to the early part of this century when thecontinuous “sawtooth” pattern of the Fl waves in leads IIand III was first reported (1,2) and attributed to an atrial
impulse circulating around both caval veins (3). Laterreports provided further evidence to the concept of anexcitation wave rotating in a counterclockwise (CCW)direction in the right atrium and giving rise to the distinct“sawtooth” pattern with predominantly negative Fl waves inthe inferior leads and V6 combined with a positive Fl wavein V1 (4,5). With the introduction of multisite endocardialmapping (6–13), entrainment techniques (6–15) and cath-eter ablative strategies in the therapeutic management of thetypical form of atrial Fl (8–11,13,16,17), Fl wave propaga-tion has been convincingly demonstrated to occur in amacroreentrant right atrial circuit confined anteriorly by thetricuspid annulus and posteriorly by the crista terminalis and
From the *Section of Cardiac Electrophysiology, Department of Medicine and the†Cardiovascular Research Institute, University of California, San Francisco, Califor-nia. This study was, in part, supported by the Royal Netherlands Academy of Arts andSciences and the National Institutes of Health (HL09602 and RO1-HL55227). Dataincluded in this study were, in part, presented at the 70th Scientific Sessions of theAmerican Heart Association, November 8–12, 1997, Orlando, Florida and the 19thScientific Sessions of the North American Society of Pacing and Electrophysiology,May 6–9, 1998, San Diego, California.
Manuscript received August 4, 1999; revised manuscript received November 9,1999, accepted December 29, 1999.
Journal of the American College of Cardiology Vol. 35, No. 5, 2000© 2000 by the American College of Cardiology ISSN 0735-1097/00/$20.00Published by Elsevier Science Inc. PII S0735-1097(00)00549-0

its inferior extension, the eustachian ridge, which act asnatural barriers of conduction (10,15). In addition to CCWrotation of the Fl wave, it has been shown that clockwise(CW) impulse rotation in the same right atrial circuit can befrequently observed (6,11–13,17). Although there is generalconcensus on the aforementioned distinct morphology ofthe 12-lead electrocardiogram (ECG) during CCW typicalatrial Fl (7,8,10–13,17), electrocardiographic features foundto be most specific for CW typical atrial Fl were morevariable and have included a predominantly positive Fl wavepolarity in the inferior leads (6,12,17) and, additionally, V6(13) as well as a short plateau phase with a wide negativecomponent in the inferior leads and an overall negative Flwave in V1 (11). Visual assessment of the Fl wave polarityon the 12-lead ECG is hampered by low-voltage, a contin-uously undulating signal (6,12) and QRST wave obscure-ment when a low degree of atrioventricular (AV) block ispresent (11). Moreover, the 12-lead ECG has been found tobe insufficient in distinguishing between CCW and CWtypical atrial Fl (11) or between the two forms of typical Fland atrial Fl not dependent on the subeustachian isthmus(13). Given our recent favorable clinical experience with theuse of body surface mapping in providing detailed spatiallocalization of ectopic right atrial activation (18), we feltthat the application of this technique might improve theperformance of the surface ECG in characterizing andclassifying typical atrial Fl (19).
This study features the application of 62-lead ECGmapping in conjunction with multisite endocardial cathetermapping in patients with typical atrial Fl to: 1) documentthe instant-by-instant changes of the CCW and CW Flwave patterns on the body surface, 2) compare the bodysurface Fl wave patterns with the underlying site of endo-cardial activation within the reentrant circuit, and 3) de-velop a reference set of body surface map patterns charac-teristic for CCW and CW Fl wave rotation.
METHODS
Patient cohort. A total of 20 consecutive patients withrecurrent typical atrial Fl referred for catheter ablation wereincluded in the study. There were 17 men and 3 women(mean age 66 6 8 years) of whom 13 patients (65%) hadconcomitant structural heart disease (Table 1). None of theenrolled patients had undergone prior ablation of typical
atrial Fl or atrial surgery for congenital heart disease. Fivepatients (25%) were receiving ongoing treatment withlow-dose amiodarone or had stopped taking this drug one tothree weeks before the study. All other antiarrhythmicagents were discontinued at least five drug half-lives beforethe study. Beta-adrenergic blocking agents or digitalistherapy was administered in seven patients (54%). Informedconsent was obtained from all patients in accordance withthe protocol approved by the Committee on Human Re-search of the University of California at San Francisco.
Multisite endocardial mapping. Four multipolar catheterswere introduced percutaneously and positioned using bi-plane fluoroscopic monitoring in the 45° right anterioroblique (RAO) and 45° left anterior oblique (LAO) projec-tions. A 7F 20-pole “Halo” catheter (2-10-2 mm interelec-trode spacing) (Cordis-Webster, Inc., Diamond Bar, Cali-fornia) was placed along the tricuspid annulus so that thedistal electrode pair was located at the lateral entrance of thesubeustachian isthmus (7:00 o’clock on LAO view) and theproximal electrode pair was situated at the high septum(2:00 o’clock on LAO view). A 6F octapolar catheter (2.5 or2.5–5-2.5 mm interelectrode spacing) (EP Technologies,Inc.) was positioned at the His bundle position or midsep-tum, while a 7F open-lumen decapolar catheter (5 mminterelectrode spacing) (DAIG, Inc., Minnetonka, Minne-sota) was advanced into the coronary sinus, thereby ensuringthat the proximal electrode pair was situated at the os of thecoronary sinus. When necessary, the exact position of thelatter catheter was verified fluoroscopically using injection ofcontrast dye. Finally, a 7F roving quadripolar catheter(2.5 mm interelectrode spacing) with a 4 mm tip electrode(EP Technologies, Inc., Sunnyvale, California) was used foractivation and entrainment mapping in the subeustachianisthmus.
Bipolar endocardial electrograms and the 12-lead surfaceECG were acquired, processed and analyzed using a 48-channel CardioLab system (Prucka Engineering, Inc.,Houston, Texas). The signals were filtered at a bandpasssetting of 30 to 500 Hz, digitized at a 1 kHz sampling rateand stored on optical disk. The signals were displayed on acolor monitor or produced as hard copy at variable gainsettings with a paper speed of 200 to 400 mm/s.
Arrhythmia induction was obtained with programmedatrial stimulation when sustained atrial Fl (.30 s duration)was not present at the onset of the mapping procedure.Verification of CCW or CW typical atrial Fl was based onthe characteristic sequence of activation and the demonstra-tion of concealed entrainment with pacing in the subeusta-chian isthmus (6–14). Entrainment mapping in the subeu-stachian isthmus was carried out according to previouslydescribed techniques (10,15).
Body surface mapping. Recording and processing of elec-trocardiographic data was performed using an on-line por-table body surface mapping system (20,21) and a radiotrans-parent carbon electrode array according to recently
Abbreviations and AcronymsAV 5 atrioventricularCCW 5 counterclockwiseCW 5 clockwiseECG 5 electrocardiogramFl 5 flutterLAO 5 left anterior obliqueRAO 5 right anterior oblique
1277JACC Vol. 35, No. 5, 2000 SippensGroenewegen et al.April 2000:1276–87 Body Surface Mapping of Typical Atrial Flutter

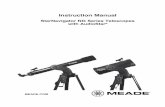
published methods (18). Briefly, unipolar ECG signals ofsingle heart beats were acquired simultaneously from 62 leadsites (Fig. 1A) using Wilson’s central terminal as a refer-ence. Lead sites in the array are referred to with a letter (Ato P) and numeric code (1 to 12) according to a division in16 columns and 12 rows, respectively; this means thatelectrode “A1” is located at the right anterior axillary linejust below the level of the suprasternal notch. Recordings ofthe surface ECG and endocardial catheter mapping ofspontaneous or electrically induced sustained atrial Fl wereperformed simultaneously during resting tidal volume res-piration. Whenever a low degree of AV block occurred (i.e.,#2:1 AV ratio) resulting in a partly obscured Fl wave due tothe superimposed QRST segment, adequate isolation of thecomplete Fl wave cycle was obtained using intravenousdelivery of adenosine (Table 1) (11). The ECG signals wereamplified, digitized at a 1 kHz sampling rate using a 14-bitsA/D converter, optically transmitted and stored on harddisk as well as removable hard disk cartridges. All leadtracings were visually screened in order to reject poor qualitysignals or signals from lead sites that were obscured bydefibrillation patches on the front and back of the chest(mean 4.2 6 4.3 per map). Replacement values were
interpolated based on adjoining lead recordings. Digitalfiltering to remove line frequency interference was per-formed when necessary with a 60-Hz notch filter. Correc-tion of interelectrode offset differences and linear baselinedrifting was performed using linear interpolation afterselecting an isoelectric time instant. Due to the absence of atrue isoelectric period in the Fl wave cycle, an interval wasselected in the signal near to the zero voltage level directlypreceding the negative inscription of the Fl wave (19). Aseries of potential maps of the entire Fl wave cycle wascomputed at 2-ms intervals. The potential maps werevisually evaluated to determine Fl wave onset and offset asthe point in time when one of the extreme values supersededa 630 mV voltage window around the zero line (18) and allextreme values had returned within this 630 mV voltagewindow, respectively. Integral maps of selected time inter-vals in the Fl wave cycle were computed for each recording(please refer to the “Data Analysis and Statistics” section forfurther details) (Fig. 1B).
Definitions. Counterclockwise typical atrial Fl was definedas a right atrial arrhythmia characterized by CCW wave-front rotation around the tricuspid annulus and critical
Table 1. Patient Details and Characteristics of Atrial Fl
Patient GenderAge(yr)
Directionof Rotation
CycleLength (ms)
AVConduction
Additional ClinicalArrhythmias/Conduction
System DiseaseStructural Heart
DiseaseAntiarrhythmic
Drugs
1 M 61 CCW 230 4:1 None None None2 M 71 CCW 260 Adenosine None MI, CABG Amiodarone*3 M 74 CW 210 6:1 PAF Idiopathic DCM None4 F 69 CCW 230 Adenosine None Dilated RA None
— — CW 230 Adenosine — — —5 M 63 CCW 230 6:1 None None Amiodarone*
— — CW 230 4:1 — — —6 M 61 CCW 230 Adenosine None None None7 F 77 CCW 220 6:1 PAF None None
— — CW 210 4:1 — — —8 M 58 CCW 300 Adenosine None Ischemic DCM,
CABGAmiodarone
9 M 56 CCW 250 4:1 None None None10 M 59 CCW 230 4:1 None MR None11 M 73 CCW 200 6:1 None None None12 M 73 CW 270 Adenosine PAF, AT Dilated RA 1 LA Amiodarone*13 M 79 CCW 230 4:1 Complete heart block** CABG, dilated LA None14 M 67 CCW 220 Adenosine PAF, SSS** CAD, CABG Amiodarone15 M 49 CCW 200 4:1 PAF Idiopathic DCM None
— — CW 200 2:1–3:1*** — — —16 M 64 CCW 220 4:1 None Idiopathic DCM None17 F 70 CCW 210 4:1 SSS** Dilated LA None18 M 64 CCW 200 4:1 PAF None None
— — atyp 170 6:1 — — —19 M 54 CCW 210 4:1 None Idiopathic DCM None20 M 72 CW 220 4:1 None Type I aortic
dissection repairNone
*Discontinued 1 to 3 weeks before procedure; **Dual chamber pacemaker implantation; ***Recordings were analyzed when 3:1 AV block occurred.AT 5 atrial tachycardia; atyp 5 atypical atrial flutter; AV 5 atrioventricular; CABG 5 coronary artery bypass grafting; CAD 5 coronary artery disease; CCW 5
counterclockwise typical atrial flutter; CW 5 clockwise typical atrial flutter; DCM 5 dilated cardiomyopathy; LA 5 left atrium; MI 5 myocardial infarction; MR 5 mitralregurgitation; PAF 5 paroxysmal atrial fibrillation; RA 5 right atrium; SSS 5 sick sinus syndrome.
1278 SippensGroenewegen et al. JACC Vol. 35, No. 5, 2000Body Surface Mapping of Typical Atrial Flutter April 2000:1276–87

dependence on the subeustachian isthmus (8 –10,13).Clockwise typical atrial Fl was defined as as a right atrialarrhythmia characterized by CW wavefront rotation aroundthe tricuspid annulus and critical dependence on the sub-eustachian isthmus (9,10,13). Atypical atrial Fl was definedas an atrial arrhythmia with a constant beat-to-beat intra-cardiac activation sequence different from either CCW orCW typical atrial Fl and not dependent on the subeusta-
chian isthmus (13). The medial and lateral part of thesubeustachian isthmus were defined as the zone between theinferior vena cava and the tricuspid annulus reaching from4:00 (i.e., the coronary sinus os) to 6:00 and 6:00 to 7:00o’clock on the LAO view, respectively. A multipolar bodysurface potential map was defined as the simultaneousoccurrence of three or more extremes at a single time instantwith an area of opposite polarity sandwiched between twoextremes of equal polarity (18). Sudden extreme movementon a body surface potential map was defined as the rapidshift of an extreme over more than two lead sites on thechest (18). The electrically silent zone of the Fl wave cycleon the surface ECG was arbitrarily defined as the timeinterval in which both the highest positive and negativepotentials were contained within a 630 mV voltage win-dow.
Data analysis and statistics. Endocardial mapping. Endo-cardial data were analyzed by determining the activationtime in each bipolar lead recording using on-screen digitalcalipers. The activation time in each bipolar signal was thenrelated to the same time instant on the simultaneouslyrecorded surface ECG, while the location of the endocardialrecording site was visually translated from biplane fluoro-scopic images to an adapted endocardial display of the rightatrial endocardium which was previously published byAnderson and Becker (22).
Body surface mapping. Electrocardiographic data wereanalyzed qualitatively by inspecting the temporal changes involtage distribution throughout the Fl wave cycle. Thisinspection entailed four steps. First, map pattern character-istics were evaluated by documenting the presence of qual-itative features representative for complex underlying pat-terns of wavefront propagation (18): 1) multipolar mappatterns; 2) pseudopod extensions, and 3) sudden extrememovement. Second, the spatial surface Fl wave morphologywas compared instant-by-instant with the actual site ofendocardial activation in the reentrant circuit. Third, theduration of the electrically silent zone in the Fl wave cyclewas determined and associated with the underlying area ofendocardial activation within the reentrant circuit. Fourth,distinct periods within the Fl wave cycle were identified atwhich stable voltage distributions occurred for a timeinterval of at least 20 ms. Subsequently, integral maps werecomputed over these selected time periods with stablevoltage distributions. In addition, mean maps were calcu-lated of all the CCW and CW typical Fl wave integral mapsto document their distinct surface map morphology.
Quantitative data evaluation was carried out by subjectingthe integral maps to a mathematical analysis using correla-tion coefficients in order to: 1) compare the intrapatientvariability of the Fl wave pattern obtained at various periodsof the Fl wave cycle with the purpose of mathematicallydetermining the surface expression of circular wavefrontpropagation, and 2) assess the interpatient comparability oftypical Fl wave patterns with the same direction of rotation
Figure 1. Display of the torso anatomy with the 62 lead positions(A) and a body surface Fl wave integral map (B). The lead arrayintegrates V1–V6 (six open circles in precordial area) and consistsof 14 vertically applied straps (marked A to P; no straps atpositions B and O; strap A located at right anterior axillary line)each containing up to 8 electrodes at 12 possible locations (marked1 to 12; electrode 1 situated at top of each strap). The integral mapwas computed over the initial time period (indicated by gray zonebetween two markers) of a CCW typical Fl wave episode obtainedin patient 16. The scalar waveform below the map is shown at ahigh gain setting and was recorded at the E9 electrode position(left lower anterior chest). The map layout relates to the torsoanatomy (panel A) in that the left and right part of the mapcorrespond to the front and back of the chest, respectively.Schematic locations of the sternum (left) and spinal column (right)are demarcated at the top of the map. Encircled plus and minussigns denote the location and amplitude of the maximum andminimum. Positive (solid in gray area), negative (dashed) and zerointegral contour lines (dotted) are additionally indicated. Theincremental step between positive and negative contour lines islinear and shown in mVms below the map under the extremeamplitudes. The integral map demonstrates right superiorly ori-ented electromotives forces during the initial part of this CCWtypical Fl wave episode.
1279JACC Vol. 35, No. 5, 2000 SippensGroenewegen et al.April 2000:1276–87 Body Surface Mapping of Typical Atrial Flutter

using a jackknife procedure (18). The latter computationswere performed using MATLAB (The MathWorks, Inc.,Natick, Massachusetts) on a Sun Sparc Station 4 (SunMicrosystems, Inc., Palo Alto, California).
All data were expressed as mean 6 SD. An unpairedtwo-tailed Student t test was performed if required with ap , 0.05 expressing statistical significance.
RESULTS
General features of atrial Fl. Counterclockwise typicalatrial Fl was found in 13 patients, CW typical atrial Fl in 3patients, both forms of typical atrial Fl in 4 patients andatypical atrial Fl in 1 patient (Table 1). The mean cyclelength of CCW and CW typical atrial flutter was 228 625 ms (range 200 to 300 ms) and 224 6 23 ms (range 200to 270 ms), respectively (Table 1). There was no significantdifference in the cycle length of typical atrial Fl betweenpatients with (229 6 28 ms) or without structural heartdisease (222 6 16 ms) (p 5 0.49). However, a significantdifference in the cycle length of typical atrial Fl was observedin patients who were presently or recently treated withamiodarone (252 6 31 ms) as opposed to patients notreceiving any antiarrhythmic drug treatment (218 6 14 ms)(p , 0.001).
Potential maps of typical atrial Fl. Map pattern character-istics. Visual evaluation of the instantaneous voltage distri-butions during typical atrial Fl showed a preponderance ofdipolar patterns although multipolarity was observed atshort periods within the Fl wave cycle in 53% and 57% ofthe CCW and CW Fl wave maps, respectively. Thesemultipolar patterns were particularly evident when rapidsurface map pattern transitions occurred, which coincidedwith the completion of right septal activation in both formsof typical Fl (60% of the multipolar Fl wave patterns). Astriking incidence of pseudopod extensions (92%) andsudden extreme movement (100%) was additionally foundwith the two Fl rotations.
Comparison of surface morphology with endocardialactivation-CCW rotation. Correlation of the temporal vari-ation in surface map pattern and the endocardial activationsequence of CCW atrial Fl is shown in the followingrepresentative example. Figure 2 displays a series of ninepotential maps obtained during CCW atrial Fl (panel C),which were each selected based on the local right atrialactivation time recorded at sites 1 to 9 (panels A and B).The first 48 ms of the Fl wave cycle (negative component ofFl wave in lead II) are characterized by a stable pattern witha maximum and minimum on the right upper and middlelower anterior chest, respectively; this coincides with acaudocranial spread of activation in the right atrial septum(sites 1 to 3) and a proximal-to-distal activation sequence ofthe coronary sinus. Then a rapid spatial transition occurs(50 ms) to a pattern reflecting a complete reversal of theextreme locations (62 ms). These phenomena occur uponarrival of the activation wavefront at the anterior free wall of
the right atrium near the superior crest (site 4). Themultipolar map pattern observed at 50 ms most probablyreflects both initial and terminal activation of the roof of theright (positive extreme at the middle anterior torso) and leftatrium (positive potentials at the left upper anterior torso),respectively. Subsequently, when the impulse travels inferi-orly down the trabeculated right atrium into the lateral partof the subeustachian isthmus (sites 5 to 9), the surfacepattern remains stable (from 56 to 148 ms) (positivecomponent in lead II) until the onset of the electricallysilent zone of the terminal Fl wave at 150 ms. One may notethat there is a subtle inferior shift of the minimum, resultingin more rightward inferiorly directed forces when activationof the lateral isthmus is nearly completed (site 9).
In the remaining 16 CCW Fl wave episodes, the spatialtransition and subsequent complete reversal of the surfacemap pattern was observed during activation of the high rightatrial septum or directly after completion of septal activation(i.e., from 2:00 to 12:00 o’clock on the LAO view). Inaddition, a proximal-to-distal activation of the coronarysinus coinciding with caudocranial septal activation wasalways found in these 16 CCW Fl wave episodes.
Comparison of surface morphology with endocardialactivation-CW rotation. Figure 3 highlights a direct com-parison of the characteristic sequential map pattern changesand the underlying site of endocardial activation within themacroreentrant circuit during CW atrial Fl. The early Flwave distribution (first 76 ms) (positive component of Flwave in lead II) shows a stable pattern with a maximum andminimum on the left middle and right upper chest, respec-tively. This pattern is the surface reflection of craniocaudalactivation of the medial part of the anterior right atrial freewall (site 1) and the entire septum until the coronary sinusos (site 2). Then, after invasion of the Fl wavefront in themedial subeustachian isthmus, a first pattern transition takesplace. The resulting map pattern features a slightly differentlocation of the maximum on the middle anterior thoraxwhile the minimum is now located on the middle left axilla(156 ms). This pattern remains stable for the next 80 msuntil isthmus activation is completed (site 3). Note that: 1)activation of the coronary sinus occurs in a proximal-to-distal direction in concert with isthmus activation, 2)completion of right atrial septal activation coincides withthe termination of the first part of the M-shaped positivecomponent of the Fl wave in lead II, and 3) concurrentactivation of the isthmus and floor of the left atrium isresponsible for the second part of the M-shaped positivecomponent of the Fl wave in lead II. Subsequently, thesurface map morphology undergoes a second transitionleading to a stable pattern with a maximum moving to theright upper chest and a slight shift of the minimum to thelower left axilla (from 170 to 220 ms). These surfacephenomena result from caudocranial activation of the rightatrial free wall (sites 4 to 9) (negative component of Fl wavein lead aVF).
1280 SippensGroenewegen et al. JACC Vol. 35, No. 5, 2000Body Surface Mapping of Typical Atrial Flutter April 2000:1276–87

All of the above described observations were also noted inthe remaining 6 CW Fl episodes: 1) complete reversal of thevoltage distribution occurred upon activation of the infero-lateral right atrial wall directly after completion of isthmusactivation (i.e., from 7:00 to 8:00 o’clock on the LAO view),2) proximal-to-distal excitation of the coronary sinus inconjunction with medial-to-lateral isthmus activation, and3) correspondence of the first and second part of the
M-shaped positive component in the inferior leads of thestandard ECG with activation of the right atrial septum(and roof of the left atrium) and combined activation of theisthmus and floor of the left atrium, respectively.
Electrically silent zone. There was a significant differencein the duration of the electrically silent zone of the typical Flwave cycle when comparing CCW (55 6 20 ms) with CWrotation (18 6 8 ms) (p , 0.0001). The electrically silent
Figure 2. Lead II and bipolar electrogram recordings (A), endocardial electrode positions (B) and body surface potential maps (C) of aCCW typical atrial Fl episode obtained in patient 17. Nine of the 11 electrograms are numbered in accordance to the temporal sequenceof their individual activation times. The encircled numbers in panels A and B relate these nine electrograms with their anatomical originin an adapted endocardial diagram of the exposed right atrium previously published by Anderson and Becker (22). The remaining twoelectrograms were recorded at the proximal (prox) and distal (dis) coronary sinus. The endocardial diagram depicts the location of thesuperior (SVC) and inferior vena cava (IVC), crista terminalis (CT), fossa ovalis (FO) and the coronary sinus os (CSO) and features theCCW direction of impulse propagation in the macroreentrant circuit. The encircled numbers in panels B and C relate the time at whicheach of the nine potential maps are displayed with the time of local activation at the numerically coded endocardial sites in the right atrialdiagram. The actual time instant is depicted below every map and marked by the vertical bar in the scalar ECG tracing. This ECG tracingwas obtained at lead position C11 (right lower anterior chest). Isopotential contours of positive and negative voltages are indicated by solid(gray area in the map) and dashed lines, respectively (see Fig. 1 for further explanation). The potential maps show a stable pattern withsuperiorly directed forces during the first 48 ms of the Fl wave while caudocranial activation of the right atrial septum (sites 1 to 3) andproximal-to-distal CS activation is taking place concurrently. After a rapid reversal in the potential map pattern, the remaining part of theFl wave (56 to 148 ms) demonstrates again pattern stability with inferiorly oriented forces while craniocaudal excitation of the free walland lateral isthmus is occurring (sites 5 to 9). Note, the complex multipolar pattern (50 ms) upon the onset of right free wall activation(site 4). The anatomic diagram of the right atrium is reproduced with permission of Gower Medical Publishing.
1281JACC Vol. 35, No. 5, 2000 SippensGroenewegen et al.April 2000:1276–87 Body Surface Mapping of Typical Atrial Flutter

zone in CCW and CW Fl episodes occurred duringactivation of the medial part of the isthmus (i.e., from 6:00to 4:00 o’clock on the LAO view) and anterolateral free wallof the right atrium (i.e., from 11:00 to 12:00 o’clock on theLAO view), respectively.
Integral maps of typical atrial Fl. CCW rotation. The Flwave cycle in CCW typical Fl could be divided in two (10of 17 episodes; 59%) or three successive time periods (7 of17 episodes; 41%) with a stable surface map pattern ofwhich integral maps were computed. A set of representativeintegral maps corresponding to a three-interval subdivisionof the Fl wave cycle is shown in Figure 4. Complete patternreversal can be observed when comparing the integral maps
of the initial with the terminal part of the Fl wave (r 520.93). It is interesting to observe that the downwarddeflection of the positive Fl wave component on the scalarECG recorded at the E9 electrode position (left loweranterior chest) is characterized by a steep, followed by agradual, decline in voltage. The first part of the gradualvoltage decline corresponds to the time interval duringwhich the third integral map was obtained and coincidedwith activation of the lateral subeustachian isthmus. Asteep-to-gradual voltage decline of the downward deflectionof the positive Fl wave component in the unipolar chestleads on the lower chest and the inferior leads of the standardECG was noted in 11 of the 17 CCW Fl episodes (65%). This
Figure 3. Display of lead II, bipolar electrograms (A) at 10 endocardial locations (B) and body surface potential maps (C) acquired duringCW typical atrial flutter in patient 5. The ECG waveform below each map was sampled at the C1 lead site (right upper anterior torso)(see Fig. 1 and 2 for further explanation). The potential maps obtained during the first 76 ms demonstrate stable inferiorly oriented forceswhile craniocaudal excitation of the medial anterior free wall (site 1), septum and CSO (site 2) is occurring. For the next 80 ms a secondstable map pattern emerges and shows leftward directed forces as a result of concurrent activation of the isthmus (site 3 is located at theexit) and CS in opposite directions. Finally, a third pattern may be observed featuring stable right superior forces during the remaining64 ms of the Fl wave when the entire free wall is activated in a caudocranial direction (sites 4 to 9). It may be noted that septal activationand subsequent combined isthmus and CS activation occur during the first and second part of the positive M-shaped component in leadII, respectively. The anatomic diagram of the right atrium is reproduced with permission of Gower Medical Publishing. CSO 5 coronarysinus os; CT 5 crista terminalis; FO 5 fossa ovalis; IVC 5 inferior vena cava; SVC 5 superior vena cava.
1282 SippensGroenewegen et al. JACC Vol. 35, No. 5, 2000Body Surface Mapping of Typical Atrial Flutter April 2000:1276–87

subset contained six of the seven CCW Fl episodes (86%) inwhich a three-interval subdivision could be obtained.
CW rotation. A division in two or three time periods witha stable map pattern was feasible in two (29%) and five ofseven CW typical Fl episodes (71%), respectively. Figure 5contains three representative integral maps of a CW Flcycle, which were each based on a time interval with a stablevoltage distribution. The integral maps corresponding withthe initial and terminal part of the Fl wave show completepattern reversal (r 5 20.81) compliant with circular rota-tion of the underlying current source. The same CW Flepisode featuring the changes in the potential distributionover time was shown in panel A of Figure 3. It can be notedthat the pattern of the initial, intermediate and terminalintegral map show a high resemblance with the potentialmaps at 66, 156 and from 196 ms, respectively.
Mean maps of CCW and CW rotation. Mean integralmaps of CCW and CW typical atrial Fl are demonstrated inFigure 6. The mean CCW integral map of the initial Flwave is characterized by a maximum on the right upper
anterior chest and a minimum on the lower left axilla(caudocranial activation of right atrial septum and proximal-to-distal activation of coronary sinus), the intermediate Flwave by a maximum on the middle anterior chest and aminimum on the right upper thorax (craniocaudal activationof the right atrial free wall) and the mean CCW integralmap of the terminal Fl wave by a maximum on the lower leftanterior torso and a minimum on the right upper anteriorchest (activation of the lateral subeustachian isthmus). InCW atrial Fl, the initial Fl wave produces a mean integralmap featuring a maximum on the right middle front and aminimum on the right upper front (craniocaudal activationof the right atrial septum); the intermediate Fl wavegenerates a map with a maximum on the right middle chestand a minimum on the middle left axilla (activation ofsubeustachian isthmus and proximal-to-distal activation ofcoronary sinus), and the terminal Fl wave leads to a meanintegral map showing a maximum on the right upper frontand a minimum on the left middle front of the torso(caudocranial activation of right atrial free wall). There
Figure 4. Set of three integral maps of the initial (T1–T2),intermediate (T2–T3) and terminal CCW typical Fl wave (T3–T4) recorded in patient 17. The ECG was acquired at the E9electrode position (left lower anterior chest) (see Fig. 1 for furtherexplanation). The maps corresponding with initial and terminal Flwave activation show a mirror image voltage distribution. It may benoted that the downward deflection of the positive Fl wavecomponent in the ECG waveform demonstrates a steep-to-gradual voltage decline; the T3–T4 time period coincides with theinitial part of this gradual voltage decline.
Figure 5. Three integral maps of successive intervals in a CWtypical atrial Fl episode obtained in patient 5. The lead tracingoriginates from the C1 lead site (right upper anterior chest) (seeFig. 1 and 4 for further explanation). Complete pattern reversal canbe noted when comparing the initial with the terminal Fl waveintegral maps.
Figure 6. Mean body surface integral maps of CCW (A) and CWtypical atrial flutter (B) showing the stereotypical dipolar mappatterns during the three successive time periods of the Fl wavecycle in each direction of rotation (see Fig. 1 and 4 for furtherexplanation). Note the high spatial resemblance between the meanintermediate CCW and initial CW Fl wave integral maps as wellas the mean initial CCW and terminal CW Fl wave integral maps.
1283JACC Vol. 35, No. 5, 2000 SippensGroenewegen et al.April 2000:1276–87 Body Surface Mapping of Typical Atrial Flutter

appeared to be a high spatial resemblance of the meanintegral maps corresponding to the intermediate CCW Flwave and the initial CW Fl wave. Similarly, the integralmaps of the initial CCW Fl wave and the terminal CW Flwave are morphologically very compatible.
Intrapatient variability. Mathematical comparison of theinitial and terminal integral map performed for each of the17 CCW typical Fl episodes shows clear evidence of thespatial map pattern reversal resulting from the underlyingrotation of the endocardial impulse and is reflected by a highnegative correlation (mean r 5 20.87 6 0.08; range 20.70to 20.96). Similar findings were obtained for the seven CWtypical Fl episodes although the negative correlations weresomewhat lower (mean r 5 20.55 6 0.29) and morevariable (range 20.05 to 20.95) compared with the resultsobtained with CCW Fl.
Interpatient comparability. Comparison among eitherCCW or CW typical Fl episodes obtained in differentpatients demonstrates a high degree of interpatient patternuniformity irrespective of the presence or absence of struc-tural heart disease. With CCW Fl, correlation coefficientsof initial integral maps ranged from 0.71 to 0.97 (mean r 50.89 6 0.09), intermediate integral maps from 0.67 to 0.97(mean r 5 0.86 6 0.10) and terminal integral maps from0.72 to 0.94 (mean r 5 0.83 6 0.09). Results with CWflutter yielded r values for initial integral maps ranging from0.64 to 0.90 (mean r 5 0.80 6 0.09), for intermediateintegral maps ranging from 0.67 to 0.97 (mean r 5 0.82 60.12) and for terminal integral maps ranging from 0.71 to0.81 (mean r 5 0.77 6 0.05).
Atypical atrial Fl. The one episode of atypical Fl showedthree successive periods in the Fl wave cycle during whichstable and predominantly dipolar map patterns were ob-served. The corresponding integral maps are shown inFigure 7. The initial 42 ms demonstrate a maximum andminimum on the middle anterior chest and upper left back,respectively (left panel). This time period is associated with:1) craniocaudal right septal activation followed by activationof the coronary sinus os, and 2) a predominantly positive Fl
wave polarity in the inferior leads of the standard 12-leadECG. Then, a first transition of the surface map patterntakes place and results in a slightly more superior position ofthe maximum on the anterior chest and a minimum locatedon the lower back (middle panel). This surface patternremains present for 52 ms and coincides with a complexendocardial activation sequence featuring concurrentcraniocaudal activation of the entire right atrial free wall,activation of the subeustachian isthmus and proximal-to-distal activation of the coronary sinus. Then, a secondsurface map pattern transition causes the maximum andminimum to move to the left upper and middle anteriorthorax, respectively (right panel). This pattern remainsstable for 38 ms until the electrically silent zone occurs at132 ms. No endocardial activity was noted in the rightatrium or coronary sinus during this last phase of the Flwave cycle. Thus, the terminal map pattern must be causedby left atrial activation, most probably by caudocranialwavefront propagation along the left atrial free wall. Inaddition, we speculate that the electrically silent zone (132to 170 ms) on the surface ECG is associated with activationof the roof of the left atrium. This atypical Fl with a probableunderlying left atrial macroreentrant circuit also showed po-tential maps featuring sudden extreme movement, pseudopodextensions and multipolarity during rapid pattern transitions.Furthermore, complete spatial reversal of the atypical Fl wavemap pattern can be noted when comparing the initial with theterminal integral map (r 5 20.77).
DISCUSSION
Main findings. This report contains the first comprehen-sive evaluation of the multiple lead surface ECG morphol-ogy of typical atrial Fl and was aimed at providing newinsight into the genesis of the Fl wave and outlining thepotential clinical utility of surface mapping techniques tocharacterize type and direction of Fl wave rotation. Byperforming simultaneous body surface and endocardialmapping during 17 episodes of CCW typical atrial Fl, sevenepisodes of CW typical atrial Fl and one episode of atypicalatrial Fl in 20 patients selected for ablative therapy, wefound that the temporal changes in Fl wave morphology onthe body surface can be directly related to the successiveactivation of major components in the atrial macroreentrantcircuit. The CCW and CW typical Fl wave cycle can eachbe divided in up to three time periods at which stable surfacemap patterns are observed; with CCW Fl, these periodscorrespond to caudocranial activation of the right atrialseptum in conjunction with proximal-to-distal activation ofthe coronary sinus (initial Fl wave), craniocaudal activationof the right atrial free wall (intermediate Fl wave) andactivation of the lateral subeustachian isthmus (terminal Flwave) (Fig. 2); with CW flutter, the time periods can beattributed to craniocaudal excitation of the right atrialseptum (initial Fl wave), excitation of the isthmus togetherwith proximal-to-distal excitation of the coronary sinus
Figure 7. Integral maps of three subsequent intervals in theatypical atrial Fl cycle recorded in patient 18. The scalar ECG wasacquired at the H1 lead site (upper left anterior axillary line) (seeFig. 1 and 4 for further explanation). One may note the spatialreversal in map pattern when comparing the initial with theterminal integral map. This surface map morphology was believedto be associated with a left atrial circuit.
1284 SippensGroenewegen et al. JACC Vol. 35, No. 5, 2000Body Surface Mapping of Typical Atrial Flutter April 2000:1276–87

(intermediate Fl wave) and caudocranial excitation of theright atrial free wall (terminal Fl wave) (Fig. 3). Potential aswell as integral maps of the initial and late period of eitherthe CCW or CW typical Fl wave cycle showed completespatial pattern reversal due to impulse propagation inopposite directions with excitation of the septal versus thefree wall section of the right atrial Fl circuit (Fig. 2 to 5). Ahigh level of quantitative interpatient concordance in bothCCW and CW typical Fl wave body surface integral mappatterns was found despite the presence of a variety oforganic heart conditions in two thirds of the patientpopulation. The atypical Fl episode was believed to beassociated with a left atrial reentrant circuit and demon-strated clearly different integral maps of the initial, inter-mediate and terminal period of the Fl wave cycle ascompared with the integral maps acquired during CCW orCW typical atrial Fl (Fig. 6 and 7).
The scalar surface ECG of typical atrial Fl and itsrelation to the intraatrial activation sequence. Puech etal. (5) showed that in patients with CCW typical atrial Fl,the positive component of the Fl wave in the inferior leadsof the 12-lead ECG represents craniocaudal activation ofthe right atrial free wall, while the negative component ofthe Fl wave relates to caudocranial propagation of theimpulse along the right atrial septum. Recently, multisiteendocardial mapping of typical atrial Fl with both directionsof rotation corroborated the earlier findings regarding thenature of the scalar CCW Fl wave (11,13). These studiesalso showed that a reversed phenomenon occurred with CWFl, i.e., craniocaudal septal and caudocranial lateral rightatrial activation while the positive and negative Fl wavecomponents in the inferior leads were inscribed. Saoudi etal. (11) demonstrated that coronary sinus activation in bothtypes of Fl rotation occurs in a proximal-to-distal directionand that the notch at the beginning of the plateau phase ofthe CW Fl wave in the inferior leads (i.e., the second partof the M-shaped component) is caused by excitation of thecoronary sinus (or floor of the left atrium). We haveobtained similar findings and noted that the first part of theM-shaped component correlates with the craniocaudal ac-tivation of the right atrial septum (and roof of the leftatrium). We additionally found that CCW impulse propa-gation in the lateral isthmus was often associated withdistinct scalar features in the lower chest leads and theinferior leads of the standard ECG. In almost two thirds ofthe CCW Fl episodes, the positive Fl wave componentdemonstrated a steep, followed by a gradual, voltage declinewith the initial part of the gradual voltage decline occurringsimultaneously with activation of the lateral isthmus (Fig. 4).
Role of the bystander atrium in generating the electro-cardiographic Fl wave. Sequential epicardial mapping ofCCW and CW macroreentrant activity in the canine sterilepericarditis model has demonstrated that the morphogene-sis of the surface Fl wave is predominantly determined bythe activation sequence of the left atrium, which appeared to
act electrically as a passive bystander (23). A similar expla-nation for the dominant Fl wave polarity in experimental Fldue to right atrial crush injury (24) as well as the typicalform of clinical atrial Fl (5,11,13) has been proposed byothers. Schoels et al. (25) stated that the Fl wave polarity inexperimental atrial Fl is related to the direction of activationof the bulk of atrial tissue. Assuming that the terms polarityor dominant component of the Fl wave relate to a deflectionof the waveform with a relatively high amplitude and rapidincrease or decrease in voltage, we feel that both thedirection of activation in the bystander atrium and thesynchronization of right and left atrial activity (i.e., theamount of simultaneously activated right and left atrialtissue mass) determine the polarity or dominant componentof the scalar Fl wave. Thus, synchronized excitation of theright atrial septum and left atrium in either a caudocranial orcraniocaudal direction will be responsible for the Fl wavepolarity in the typical form of atrial Fl where the reentrantcircuit is located in the right atrium. Although the remain-ing “nondominant” part of the scalar Fl wave in typical atrialFl, generated by sequential activation of the right atrial freewall in a craniocaudal or caudocranial direction, may bedifficult to evaluate visually due to its relatively low ampli-tude, it should be emphasized that the use of spatial ECGsampling with a high signal-to-noise ratio does enable adetailed instant-by-instant representation of the “nondomi-nant” Fl wave voltage distribution on the human torso.Indeed, the ability to spatially capture nearly the entire Flwave distribution using the surface mapping approachadditionally unveiled a striking pattern correspondence ofthe mean integral maps belonging to the intermediateCCW Fl wave and the initial CW Fl wave as well as themean integral maps belonging to the initial CCW Fl waveand the terminal CW Fl wave (Fig. 6). This intriguingfinding reiterates the importance of the direction of wave-front propagation in either the right atrial free wall orseptum (and left atrium) in determining the spatial distri-bution of typical atrial Fl waves on the torso surface.
Biatrial wavefront propagation and cancellation of elec-tromotive forces. Boineau et al. (26) obtained canineepicardial mapping data during naturally occurring CCWand CW right atrial Fl. They showed that synchrony indirection of wavefront propagation and cancellation ofopposing wavefront propagation determine the presence ornear absence of electromotive forces on the surface ECG,respectively. During clinical observations using multisiteright atrial endocardial mapping in patients with atrialfibrillation, Roithinger et al. (27) noted that the amplitudeand polarity in the V1 lead tracing were distinctly related tothe degree and direction of organized activation of the inclose proximity situated trabeculated right atrium, despitethe cancellation effects created by simultaneously occurringdisorganized activation on the right atrial septum. In theintermediate period of the CW typical Fl cycle, whileconcomitant activation of the subeustachian isthmus and
1285JACC Vol. 35, No. 5, 2000 SippensGroenewegen et al.April 2000:1276–87 Body Surface Mapping of Typical Atrial Flutter

concentric activation of the coronary sinus (and floor of theleft atrium) is taking place in opposite directions, we wereable to obtain a reproducible dipolar map pattern on thetorso surface (Fig. 3, 5 and 6). Thus, two simultaneousbiatrial wavefronts travelling in opposite directions do notcause complete cancellation but rather an interaction be-tween their respective electromotive forces that result in adistinct dipolar surface map distribution. Although one mayeven expect to see multipolarity of the surface map patternas a reflection of the aforementioned two activation wave-fronts, insufficient separation of the electrical sources mostprobably precluded the observation of such phenomena.
The electrically silent zone of the Fl wave cycle on thesurface ECG. In the Langendorff-perfused canine heart,Allessie and coworkers (28) performed endocardial mappingof pacing and acetylcholine induced left and right atrial Fl.These authors observed that continuous electrical activitywas only present in one of the two atria (i.e., the atriumcontaining the Fl circuit) and that the amount of instanta-neously activated myocardium was less than 5% during halfof the Fl wave cycle. They suggested that the endocardiallyquiescent part of the Fl wave cycle was due to activationthrough a narrow isthmus of atrial myocardium that waspart of the macroreentrant circuit and responsible for the“isoelectric” segment on the surface ECG. Subsequentclinical observations in patients with CCW typical atrial Flcorroborated these experimental results in that the “isoelec-tric” segment on the surface ECG relates to activation of thelow right atrium (i.e., the subeustachian isthmus) (7,13).Similarly, we found with CCW typical Fl that activation ofthe small muscle mass of the medial part of the subeusta-chian isthmus generates a low amount of electromotiveforces, which results in a period of relative electrical silenceon the surface ECG (i.e., voltages within a 630 mVwindow). In addition, it appeared that the timing of thesilent zone on the surface ECG is not only related to theabsolute muscle mass of a given segment of the right atrialFl circuit but also to the time at which passive activation ofthe bystander left atrium occurs. In fact, the electricallysilent zone in both rotations of typical atrial Fl can beobserved just before the onset of passive left atrial activation.While the silent zone in CCW typical Fl is noted to occurduring activation of the medial isthmus when caudocranialactivation of the bystander left atrium is about to commencevia a lower transseptal route, the silent zone in CW typicalFl appears to coincide with terminal activation of theanterolateral free wall of the right atrium at the level of thesuperior crest just before the start of craniocaudal excitationof the left atrium via Bachmann’s bundle. The fact that theduration of the electrically silent zone was significantlylonger in CCW (55 6 20 ms) as opposed to CW typical Fl(18 6 8 ms) most probably relates to differences in mass andpossibly conduction velocity due to the anatomic architec-ture of the rim of atrial muscle at the level of the isthmusand anterolateral free wall of the right atrium.
Study limitations. Because typical atrial Fl is characterizedby continuous macroreentrant activity around the tricuspidannulus, per definition the Fl waveform on the surface ECGwill not contain a true isoelectric interval. There are,however, distinct time instants in both the CCW and CWtypical Fl wave cycle when a minimal amount of electromo-tive forces is generated at which time the surface ECG canbe considered to be electrically silent. In our approach forbaseline correction and definition of the zero voltage level,we decided to select such a time instant directly precedingthe negative inscription of the Fl wave in accordance withthe methods described by Kawano et al. (19). Althoughunlikely, due to the high quantitative interpatient concor-dance in both CCW and CW Fl map patterns, we cannotexclude that minor artefacts may have been introduced bythe visually guided selection of the zero voltage.
Due to the lower clinical prevalence of CW as comparedwith CCW typical atrial Fl (11–13,17), we were only able toinclude a restricted number of CW Fl episodes in theanalysis of this report. Therefore, one may question whetherthe current findings on CW typical Fl can be extrapolated tolarger patient populations. However, we feel that the repro-ducibility of the visual CW Fl potential map analysis on apatient-to-patient basis, the high quantitative interpatientCW Fl map pattern correspondence and a comparabledistribution of patients with and without associated heartdisease in the CW typical Fl group (Table 1) justify the useof the currently developed set of mean CW typical Flintegral maps as a reference frame to guide future analysis.
The use of surface maps to improve detection of typicalatrial Fl or optimize electrocardiographic characterization ofFl circuit location may be particularly useful in the clinicalscenario where typical atrial Fl may not be recognized andconsidered for ablative therapy because the 12-lead ECGpattern during CW rotation is not “close to classic” (11) orwhen the 12-lead ECG pattern of a truly atypical atrial Flmay be mistakenly labeled as a typical Fl that would beamenable for ablation (13). It was beyond the scope of thisstudy to compare the performance of 62 versus 12-leadECG recordings in their ability to detect and classify typicalatrial Fl. Nevertheless, future prospective studies designedto address this issue are warranted in order to fully deter-mine the clinical role of spatial 62-lead ECG sampling inthe management of atrial Fl.
Clinical relevance and future directions. The presentdata show that application of 62-lead ECG mapping tocharacterize typical atrial Fl offers a comprehensive spatialrepresentation of the specific CCW and CW typical Fl wavemorphology on the human torso surface. This spatial ECGsampling approach allows for direct correlations of theinstantaneous surface map pattern during a given timeperiod in the Fl wave cycle with activation of distinctcomponents in the right atrial macroreentrant circuit. Inaddition, the mean integral maps of the three main stages inthe CCW or CW typical Fl wave cycle present a unique
1286 SippensGroenewegen et al. JACC Vol. 35, No. 5, 2000Body Surface Mapping of Typical Atrial Flutter April 2000:1276–87

reference set of map patterns that can be used for moresophisticated and less ambiguous clinical classification of theFl type and its direction of rotation than currently feasiblewith the existing algorithms based on scalar features of the12-lead ECG. Clinical application of the reference set ofmean CCW and CW typical Fl wave integral maps mayalso lead to improved noninvasive methods of patientselection so that treatment strategies can be better tailoredregarding the optimal choice of therapy before invasiveelectrophysiologic studies are carried out.
At present, we are unaware about the specificity of surfacemapping techniques in being able to discriminate typicalfrom atypical atrial Fl with either a nonisthmus dependentrightsided circuit (13) or a circuit located in the left atrium(29,30). Although we did find clearly different Fl waveintegral map patterns in the one example of atypical Flbelieved to be associated with a left atrial circuit, on a largerscale we do not know whether the spatial map pattern ofatypical Fl will contain particular features specific to a givenand potential leftsided circuit location. However, given theinvasive nature and risk of transseptal catheter manipulationwhen targeting ablation of anticipated leftsided circuits, it isobvious that the development of noninvasive techniquesthat allow predictions about atypical Fl circuit locations maybe of critical importance not only to guide the process ofclinical decision making but also to accelerate and focuscatheter activation and entrainment mapping to a confinedarea of interest. These issues should be the subject of study infuture clinical investigations so that improved and more com-plete multiple-lead ECG classification algorithms becomeavailable that cover the entire clinical spectrum of atrial Fl.AcknowledgmentsWe thank Mark Potse, MSc, and Andre C. Linnenbank,PhD, for their assistance in data processing.
Reprint requests and correspondence: Dr. Arne Sippens-Groenewegen, Section of Cardiac Electrophysiology, Departmentof Medicine, University of California at San Francisco, 500Parnassus Avenue, MU-East 4S, Box 1354, San Francisco, Cali-fornia 94143-1354. E-mail: [email protected].
REFERENCES
1. Jolly WA, Ritchie WT. Auricular flutter and fibrillation. Heart1910–1911;2:177–221.
2. Lewis T, Drury AN, Iliescu CC. A demonstration of circus movementin clinical flutter of the auricles. Heart 1921;8:341–59.
3. Lewis T, Feil HS, Stroud WD. Observations upon flutter andfibrillation. Part II. The nature of auricular flutter. Heart 1918–1920;7:191–245.
4. Rytand DA. The circus movement (entrapped circuit wave) hypothesisand atrial flutter. Ann Int Med 1966;65:125–59.
5. Puech P, Latour H, Grolleau R. La flutter et ses limites. Arch MalCoeur 1970;61:115–44.
6. Cosio FG, Goicolea A, Lopez-Gil M, et al. Atrial endocardialmapping in the rare form of atrial flutter. Am J Cardiol 1990;66:715–20.
7. Olshansky B, Okumura K, Hess PG, Waldo AL. Demonstration of anarea of slow conduction in human atrial flutter. J Am Coll Cardiol1990;16:1639–48.
8. Feld GK, Fleck PR, Chen PS, et al. Radiofrequency catheter ablation
for the treatment of human type I atrial flutter. Identification of acritical zone in the reentrant circuit by endocardial mapping tech-niques. Circulation 1992;86:1233–40.
9. Lesh MD, Van Hare GF, Epstein LM, et al. Radiofrequency ablationof atrial arrhythmias. Results and mechanisms. Circulation 1994;89:1074–89.
10. Olgin JE, Kalman JM, Fitzpatrick AP, Lesh MD. Role of right atrialendocardial structures as barriers to conduction during human type Iatrial flutter. Circulation 1995;92:1839–48.
11. Saoudi N, Nair M, Abdelazziz A, et al. Electrocardiographic patternsand results of radiofrequency catheter ablation of clockwise type I atrialflutter. J Cardiovasc Electrophysiol 1996;7:931–42.
12. Cosio FG, Arribas F, Lopez-Gil M, Nunez A. Catheter mappingstudies in atrial flutter. In: Waldo AL, Touboul P, editors. AtrialFlutter: Advances in Mechanisms and Management. Armonk, NY:Futura Publishing Company, 1996:269–83.
13. Kalman JM, Olgin JE, Saxon LA, et al. Electrocardiographic andelectrophysiologic characterization of atypical flutter in man. Use ofactivation and entrainment mapping and implications for catheterablation. J Cardiovasc Electrophysiol 1997;8:121–44.
14. Waldo AL, MacLean WAH, Karp RB, et al. Entrainment andinterruption of atrial flutter with pacing. Studies in man followingopen heart surgery. Circulation 1977;56:737–45.
15. Kalman JM, Olgin JE, Saxon LA, et al. Activation and entrainmentmapping defines the tricuspid annulus as the anterior barrier in typicalatrial flutter. Circulation 1996;94:398–406.
16. Saoudi N, Mouton-Schleiffer D, Letac B. Direct catheter fulgurationof atrial flutter. Lancet 1987;2:568–9.
17. Cosio FG, Arribas F, Lopez-Gil M, Gonzalez HD. Radiofrequencyablation of atrial flutter. J Cardiovasc Electrophysiol 1996;7:60–70.
18. SippensGroenewegen A, Peeters HAP, Jessurun ER, et al. Bodysurface mapping during pacing at multiple sites in the human atrium.P wave morphology of ectopic right atrial activation. Circulation1998;97:369–80.
19. Kawano S, Sawanobori T, Hiraoka M. Body surface maps in two casesof atrial flutter. Jpn Heart J 1984;25:283–92.
20. Metting van Rijn AC, Kuiper AP, Linnenbank AC, Grimbergen CA.Patient isolation in multichannel bioelectric recordings by digitaltransmission through a single optical fiber. IEEE Trans Biomed Eng1993;40:302–8.
21. Linnenbank AC. On-Site Recording, Analysis and Presentation ofMultichannel ECG Data. PhD Thesis, University of Amsterdam, theNetherlands, 1996.
22. Anderson RH, Becker AE. Cardiac Anatomy. An Integrated Text andColor Atlas. London, United Kingdom: Gower Medical Publishing,1980.
23. Okumura K, Plumb VJ, Page PL, Waldo AL. Atrial activationsequence mapping during atrial flutter in the canine pericarditis modeland its effects on the polarity of the flutter wave in the electrocardio-gram. J Am Coll Cardiol 1991;17:509–18.
24. Feld GK, Shahandeh-Rad F. Activation patterns in experimentalcanine atrial flutter produced by right atrial crush injury. J Am CollCardiol 1992;20:441–51.
25. Schoels W, Offner B, Brachmann J, et al. Circus movement atrialflutter in the canine sterile pericarditis model. Relation of character-istics of the surface electrocardiogram and conduction properties of thereentrant pathway. J Am Coll Cardiol 1994;23:799–808.
26. Boineau JP, Schuessler RB, Mooney CR, et al. Natural and evokedatrial flutter due to circus movement in dogs. Role of abnormal atrialpathways, slow conduction, nonuniform refractory period distributionand premature beats. Am J Cardiol 1980;45:1167–81.
27. Roithinger FX, SippensGroenewegen A, Karch MR, et al. Organizedactivation during atrial fibrillation in man: endocardial and electrocardio-graphic manifestations. J Cardiovasc Electrophysiol 1998;9:451–61.
28. Allessie MA, Lammers WJEP, Bonke IM, Hollen J. Intraatrialreentry as a mechanism for atrial flutter induced by acetylcholine andrapid atrial pacing in the dog. Circulation 1984;70:123–35.
29. Olgin JE, Jayachandran JV, Engesstein E, et al. Atrial macroreentryinvolving the myocardium of the coronary sinus: a unique mechanismfor atypical flutter. J Cardiovasc Electrophysiol 1998;9:1094–9.
30. Jais P, Haissaguerre M, Shah DP, et al. A new electrophysiologicalsubstrate for spontaneous left atrial flutter [abstract]. PACE 1998;21:794.
1287JACC Vol. 35, No. 5, 2000 SippensGroenewegen et al.April 2000:1276–87 Body Surface Mapping of Typical Atrial Flutter