Biomechanical Stability of a Posterior-Alone Fixation Technique After Craniovertebral Junction...
-
Upload
roy-thomas-daniel -
Category
Documents
-
view
212 -
download
0
Transcript of Biomechanical Stability of a Posterior-Alone Fixation Technique After Craniovertebral Junction...

PEER-REVIEW REPORTS
Biomechanical Stability of a Posterior-Alone Fixation Technique After CraniovertebralJunction Realignment
Roy Thomas Daniel1, Aditya Muzumdar 2, Aditya Ingalhalikar 2, Mark Moldavsky2, Saif Khalil2tbr
imbnTdcnt(St
oai
M
SSsm(sa5t
cwas
INTRODUCTION
Craniovertebral junction anomalies (non-traumatic) are primarily of two types: reduc-ible atlantoaxial dislocation and basilar in-vagination. Basilar invagination syndrome ischaracterized by upward migration of theodontoid process of the second cervical verte-bra. Basilar invagination is usually seen in pa-tients with bone diseases such as rheumatoidarthritis, hyperparathyroidism, Paget disease,osteogenesis imperfecta, and rickets. It maylead to narrowing and stenosis of the fora-men magnum and result in fatal compres-sion of the brain stem, manifesting as sud-den death (2).
The standard and most accepted form oftreatment of patients with basilar invagina-tion is a transoral decompression (3, 5, 22).Because of the instability of the region result-ing from this procedure, many authors haverecommended simultaneous posterior occip-itoaxial or atlantoaxial fixation surgery (3, 5,6, 12, 23, 26, 28). An alternate technique, anoccipitocervical fixation after cervical tractionto reduce basilar invagination, has been pro-
Key words� Basilar invagination� Biomechanics� Craniovertebral junction realignment
Abbreviations and AcronymsMLW: Midline wiringPI: Posterior instrumentationROM: Range of motionS: Spacers
From the 1Centre HospitalierUniversitaire Vaudois, Lausanne,
Switzerland; and 2Globus Medical, Inc., Audubon,Pennsylvania, USA
To whom correspondence should be addressed:Aditya Muzumdar, M.S.[E-mail: [email protected]]
Citation: World Neurosurg. (2012) 77, 2:357-361.DOI: 10.1016/j.wneu.2011.06.039
Journal homepage: www.WORLDNEUROSURGERY.org
Available online: www.sciencedirect.com
1878-8750/$ - see front matter © 2012 Elsevier Inc.All rights reserved.
posed (12). Nevertheless, in some of the pa- t
WORLD NEUROSURGERY 77 [2]: 357-361
ients, transoral decompression was requiredecause the implants could not sustain theeduction of basilar invagination.
Recently, a new technique to treat basilarnvagination by distraction and realign-
ent through a posterior approach haseen developed and is similar to the tech-ique popularized by Goel et al (8-10, 16).he initial clinical results with this proce-ure have been favorable (16). Long-termlinical and radiological assessments areow in progress, and the early data ob-
ained attest to the stability of the fixationChacko AG et al., oral communication,eptember 4, 2008). The biomechanics ofhis surgical procedure would further quan-
� OBJECTIVE: The aim of the current sstability and fixation strength providetechnique to realign the craniovertebr
� METHODS: We tested seven humaiput-C4) by applying pure moments ofas tested in the following modes: 1) i
rticulation (S); 4) spacers plus C1-C2pacers plus C1-C2 posterior instrume
C1-C2 range of motion for each conslateral bending, and axial rotation.
� RESULTS: In all the loading modesignificantly reduced range of motiocondition (P < 0.05). There was no statinstrumentation constructs (P > 0.05).
� CONCLUSIONS: This study investiapproach technique for realignmentmade comparisons with additional powere stable in all three loading modestability as compared to stand-alone sout by using midline wiring, increasednot much difference in the stabilitywithout. The present study highlights threaffirms the view that distraction oarticular joint atlantoaxial fixation wobasilar invagination.
ify the stability provided by it. The objective g
, FEBRUARY 2012 ww
f this study was to biomechanically evalu-te the surgical constructs performed dur-ng this procedure.
ATERIALS AND METHODS
pecimen Preparationeven fresh human cadaver occipitocervicalpines (occiput-C4) were used. The speci-ens were obtained from the MedCure
Portland, Oregon, USA) tissue bank. Thepecimens were harvested from two femalend five male cadavers (mean age of death,3 � 4 years) and stored at �20°C beforehawing. The spines had been radio-
was to investigate the biomechanicala posterior approach reconstructionnction.
adaver occipito-cervical spines (oc-Nm on a spine tester. Each specimen
t; 2) injured; 3) spacers alone at C1-C2terior Instrumentation (S�PI); and 5)
on plus midline wiring (S�PI�MLW).t was obtained in flexion-extension,
, S�PI, and S�PI�MLW constructsmpared with the intact and injuredal difference between any of the three
d the biomechanics of the posteriore craniovertebral junction and also
or fixations. The stand-alone spacerssterior instrumentation increased thers. The third point of fixation, carriedstability further. However, there wasrted with the midline wiring versusomechanics of this novel concept ande C1-C2 articular facets and directe an ideal method of management of
tudyd byal ju
n c�1.5ntacPos
ntatitruc
s, Sn coistic
gateof thsteris. Popace
theimpae bif th
uld b
raphed previously in the anteroposterior
w.WORLDNEUROSURGERY.org 357

Ca(astato
FTaa
wspEtptrctelp
tTcscmar
tt(�flatq
SEaalsmaCam(
PEER-REVIEW REPORTS
ROY THOMAS DANIEL ET AL. POSTERIOR-ALONE FIXATION TECHNIQUE
and lateral planes to ensure the absence offractures, deformities, and any metastaticdisease. The spines were carefully denudedof paravertebral musculature while preserv-ing the spinal ligaments, joints, and diskspaces. Each spine was potted proximally atthe occiput and distally at C4 in a 3:1 mix-ture of Bondo auto body filler (Bondo Mar-Hyde Corp, Atlanta, Georgia, USA) and fi-berglass resin (Home-Solution All Purpose;Bondo MarHyde Corp).
Plexiglas markers, each having three infra-red light-emitting diodes, were secured rig-idly to the anterior aspect of the occiput, C1,C2, C3, and C4 vertebral bodies by the use of
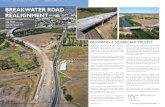
Figure 1. Surgical constructs. (A) Spacers alone aposterior instrumentation (S�PI). (C) Spacers pluwiring construct (S�PI�MLW)
bone screws to track its motion with Optotrak t
358 www.SCIENCEDIRECT.com
ertus (NDI, Inc. Waterloo, Canada) motionnalysis system. The location of the markersdenoting a rigid body) was approximatelyligned sagittally along the curvature of thepine. The Optotrak Certus software was ableo superimpose the coordinate systems of twodjacent vertebral bodies to inferentially de-ermine the relative Eularian rotations in eachf the three planes.
lexibility Testinghe specimen was fixed to the load frame ofsix degree of freedom spine simulator andpure moment was applied to the occiput
2 articulation (S). (B) Spacers plus C1-C2C2 posterior instrumentation plus midline
hrough servomotors (7, 24). The specimen
WORLD NEUROSURGE
as kept moist throughout the test bypraying it with 0.9% saline. All tests wereerformed at a room temperature of 25°C.ach of the test constructs were subjected to
hree load– unload cycles in each of thehysiologic planes generating flexion-ex-
ension, right-left lateral bending, andight-left axial rotation load-displacementurves. This was achieved by programminghe motors to apply continuous moments inach physiologic plane. A typical load-un-oad cycle in the sagittal plane was com-osed of neutral � full flexion � full exten-
sion � neutral (three times). Data from thehird cycle were considered for analysis.he design of the load frame enables un-onstrained motion of the spine in re-ponse to an applied load. There was noompressive preload applied on the speci-en. A load control protocol was used to
pply a maximum moment of � 1.5 Nm at aate of 1°/sec (7, 17, 24, 30).
The three-dimensional intervertebral ro-ation was obtained from the Optotrak Cer-us data files in the form of Euler anglesdegrees) about the X, Y, and Z axes: �Rx/
Rx, �Ry/�Ry, and �Rz / �Rz denotingexion-extension, right-left axial rotation,nd right-left lateral bending range of mo-ion (ROM), respectively. The Euler se-uence used in this study was xzy.
tudy Designach specimen (occiput-C4) was tested bypplying pure moments of �1.5 Nm. ROMt C1-C2 was obtained in flexion-extension,ateral bending, and axial rotation. Eachpecimen was tested in the followingodes: 1) intact; 2) injured; 3) spacers alone
t C1-C2 articulation (S); 4) spacers plus1-C2 posterior instrumentation (S�PI);nd 5) spacers plus C1-C2 posterior instru-entation plus midline wiring construct
S�PI�MLW; Figure 1). After the intacttesting, injury was simulated by disruptingthe articulation between C1 and C2 bilater-ally. Spacers (COLONIAL 5-mm small 0°;Globus Medical Inc, Audubon, Pennsylva-nia, USA) typically used for cervical inter-body fusion were inserted between C1 andC2 articulations bilaterally. Posterior in-strumentation was carried out at C1-C2 bythe use of C1 lateral mass screws (4 � 32mm) and C2 pedicle screws (4 � 22 mm)with the use of PROTEX CT (Globus Medi-cal Inc) polyaxial screws. A poly-ether-
t C1-Cs C1-
ether-ketone spacer was wedged between
RY, DOI:10.1016/j.wneu.2011.06.039

dtaTpc
S
P � 0.
PEER-REVIEW REPORTS
ROY THOMAS DANIEL ET AL. POSTERIOR-ALONE FIXATION TECHNIQUE
the posterior arch of atlas and the C2 spi-nous process, and then a midline C1-C2modified Gallie’s fixation was performedwith the use of 1.1-mm stainless-steel wire.Subsequent to intact testing, the instru-mented constructs were subjected to thesame load control protocol for flexibilitytesting as described previously.
Data AnalysisROM data were normalized to intact (100%).Statistical analysis was performed on raw
Figure 2. Comparison of C1-C2 ROFigure shows comparison betwee(S�PI); and 3) spacers plus C1-C2significantly different than intact (
Table 1. C1-C2 ROM (% values) During DIntact; Injured; S; S�PI; and S�PI�MLW
Loading Modes Intact Injured
Flexion-extension 100 � 0 131 � 37
Lateral bending 100 � 0 106 � 51
Axial rotation 100 � 0 140 � 76
S, spacers alone at C1-C2 articulation; S�PI, spacers � Cposterior instrumentation � midline wiring construct.
*Represents significantly different than intact condition (P†Represents significantly different than injured condition (
conditions have not been presented in
WORLD NEUROSURGERY 77 [2]: 357-361
ata. Comparison of data was performed byhe use of repeated-measures analysis of vari-nce for independent samples followed byukey’s post-hoc analysis for multiple com-arison procedures. Significance was ac-epted at P � 0.05.
RESULTS
The means � SD for ROM (%) in all loadingmodes are presented in Table 1 and Figure 2.
values) in flexion-extension, lateral bending, andpacers alone at C1-C2 articulation (S); 2) spacerserior instrumentation plus midline wiring construc.05). †Represents significantly different than injure
nt Loading Modes (Mean � SD) for
S S � PI S � PI � MLW
8 � 9*† 13 � 9*† 10 � 7*†
8 � 6*† 4 � 3*† 4 � 3*†
2 � 1*† 1 � 0.5*† 1 � 1*†
osterior instrumentation; S�PI�MLW, spacers � C1-C2
5).05).
the graph to appreciate the difference between the inst
, FEBRUARY 2012 ww
Flexion-ExtensionThe injured ROM increased to 131% � 37%(P � 0.05) as compared with intact. The S(18% � 9%), S�PI (13% � 9%), andS�PI�MLW (10% � 7%) constructs signif-icantly reduced ROM when compared withintact (P � 0.05). When compared with theinjured state, all three constructs signifi-cantly reduced ROM (P � 0.05).
Lateral BendingThe injured ROM increased to 106% � 51%(P � 0.05) as compared with intact. The S(8% � 6%), S�PI (4% � 3%), andS�PI�MLW (4% � 3%) constructs signif-icantly reduced the ROM when comparedwith intact (P � 0.05). When comparedwith the injured state, all three constructssignificantly reduced ROM (P � 0.05).
Axial RotationThe injured ROM increased to 140% � 76%(P � 0.05) as compared with intact. The S(2% � 1%), S�PI (1% � 0.5%), and�PI�MLW (1% � 1%) constructs signifi-
otation. The intact ROM is 100%.1-C2 posterior instrumentationI�MLW). �Represents
� 0.05). Intact and Injured
M (% axial rn 1) s plus Cpost t (S�P
P � 0 d (P
iffere
1
1-C2 p
� 0.0
rumentation constructs.
w.WORLDNEUROSURGERY.org 359

ost-o
PEER-REVIEW REPORTS
ROY THOMAS DANIEL ET AL. POSTERIOR-ALONE FIXATION TECHNIQUE
cantly reduced the ROM when compared tointact (P � 0.05). When compared with theinjured state, all three constructs signifi-cantly reduced ROM (P � 0.05). There wasno statistical significance between the ROMof the instrumented constructs in any of theloading modes (Table 1 and Figure 2).
DISCUSSION
Basilar invagination may be possibly re-duced by distracting the articular surfacesbetween atlas and axis. In this technique,the patient is placed prone with the headend of the table elevated to approximately35°. Cervical traction is given, and theweights are progressively increased to amaximum of one-fifth of the body weight toattain optimum realignment of the cranio-vertebral junction. The distracted positionis maintained by insertion of spacers intothe lateral atlantoaxial joints. Stand-alonespacers may be used in select cases (such as
Figure 3. Sagittal computed tomogjoints (patient with basilar invaginshow the reduction of the listheswith the spacers. (A) Pre-op. (B) P
Figure 4. Midsagittal computed tom
achieved. (A) Pre-op. (B) Post-op.360 www.SCIENCEDIRECT.com
in children, in whom the posterior pediclescrew fixation may be difficult because ofthe size of the lateral masses and pedicle orbecause of anatomical variations). Addi-tional fixation could be provided by poste-rior instrumentation and midline wiringconstructs to further stabilize the joint.
Several authors have shown that the useof screw/rod systems with placement of C1lateral mass screws and C2 pedicle screws isa safe and effective system for achievingC1-C2 fusion. It has a good safety profile, isassociated with a low complication rate,and may also be applicable to most patients(1, 11, 13-15, 18-20). For a patient with moreposterior instability, standard cable con-structs provide adequate stability in con-junction with additional posterior instru-mentation (25). In basilar invagination,either congenital or of acquired causes suchas rheumatoid arthritis or tuberculosis, theligamentous structures supporting theC1-C2 lateral facetal joints are diseased orincompetent. This technique focuses on the
scans through the lateral C1-C2ttributable to rheumatoid arthritis)maintenance of the distraction
p.
phy scans showing the distraction
WORLD NEUROSURGE
realignment at these joints and thereforehas the advantage of effectively immobiliz-ing the joint with preparation of the articu-lar surfaces and implantation of adequatelysized spacer filled with bone chips. Thisjoint treatment not only reduces the disloca-tion, but also favors the development of astrong bony lateral pillar fusion that wouldimpart added stability to the craniovertebraljunction.
Our clinical results with this procedurehave been favorable (Figures 3 and 4). Aprospective study of 27 patients with basilarinvagination who underwent this proce-dure is currently in progress. The estima-tion of the distraction achieved was as-sessed by well-established craniometricmeasurements. The median distractionachieved at the midline by the use of Cham-berlain (4), McRae (21), and Thiebaut et al.(29) lines were 8.7 mm, 8.8 mm, and 12.4mm, respectively.
The present study highlights the biome-chanical stability provided by stand-alonespacers combined with the posterior instru-mentation and midline wiring constructs.For this evaluation, human cadaveric cervi-cal spines were used. Human spines areideal for performing in vitro spinal recon-struction and biomechanical testing. How-ever, in vitro biomechanical evaluationshave inherent limitations, such as exclusionof the effect of muscles, weight of the torsoabove the instrumented level, and complexmovements occurring in vivo. The spinesimulator currently doesn’t have the capa-bility of applying follower load (preload)(27) to the specimen.
With clinical basilar invagination, thereis pathological vertical settling, presumablyas the result of deformation of the bonesand laxity of the ligaments. However, theinjury model simulated in our study doesnot closely approximate this condition. Theinjured model did not have any ligamentouslaxity, which were then jacked up to a newheight far exceeding the physiologicalheight. Ligaments were likely stretched ex-tremely tight in this model, which might bedifferent than the case in which height isrestored to normal in a patient with pathol-ogy. This difference would account for thestability in the condition of spacers only.
This study investigated the biomechanicsof the posterior-alone fixation technique,compared with additional posterior fixa-
raphyation ais and
ogra
tions. The stand-alone spacers were stable
RY, DOI:10.1016/j.wneu.2011.06.039

1
1
1
1
1
1
1
1
1
1
2
2
2
2
2
2
2
2
2
2
3
CdeeGM
r
CD
J
A
PEER-REVIEW REPORTS
ROY THOMAS DANIEL ET AL. POSTERIOR-ALONE FIXATION TECHNIQUE
in all three loading modes, and additionalposterior instrumentation further increasedstability. The third point of fixation per-formed with the use of midline wiring in-creased the stability further. However, therewas not much difference in the stability im-parted with the midline wiring versus with-out. Hence, spacers with posterior instru-mentation may provide adequate stability toreduce basilar invagination. Considering thatthis is a biomechanical cadaveric study andnot a model that would replicate dynamics ofa long-standing bone fusion after realign-ment, it would not be possible to concludeelimination of the third point of fixation fromthe procedure in clinical practice. It shouldalso be noted that in this study we evaluatedthe initial stability offered by the constructsand do not account for the effect of fatiguetesting (sequential loading) on the con-structs. Long-term clinical results with thissystem of realignment and fixation, therefore,need to be studied to assess stability at thecraniovertebral junction after bony fusion hasoccurred.
This technique of craniovertebral junc-tion realignment provides neural decom-pression and stabilization through a solelyposterior approach and has demonstratedfavorable short-term clinical results (16).The present study effectively highlights thebiomechanics of this novel concept. It reaf-firms the view that distraction of the C1-C2articular facets and direct articular joint at-lantoaxial fixation in the distracted positionwould be an ideal method of managementof basilar invagination.
REFERENCES
1. Aryan HE, Newman CB, Nottmeier EW, Acosta FL Jr,Wang VY, Ames CP: Stabilization of the atlantoaxialcomplex via C-1 lateral mass and C-2 pedicle screwfixation in a multicenter clinical experience in 102patients: modification of the Harms and Goel tech-niques. J Neurosurg Spine 8:222-229, 2008.
2. Bhagra A, Stead LG: Basilar invagination, a rare con-dition mimicking posterior circulation stroke. Neu-rocritical Care 5:213-214, 2006.
3. Bonney G, Williams JP: Trans-oral approach to the
upper cervical spine. A report of 16 cases. J BoneJoint Surg Br 67:691-698, 1985.WORLD NEUROSURGERY 77 [2]: 357-361
4. Chamberlain WE: Basilar impression (platybasia): abizarre developmental anomaly of the occipitalbone and upper cervical spine with striking and mis-leading neurologic manifestations. Yale J Biol Med11:487-496, 1939.
5. Crockard HA: Anterior approaches to lesions of theupper cervical spine. Clin Neurosurg 34:389-416,1988.
6. Di Lorenzo N: Craniocervical junction malforma-tion treated by transoral approach: A survey of 25cases with emphasis on postoperative instability.Acta Neurochir (Wien) 118:112-116, 1992.
7. Gabriel JP, Muzumdar AM, Khalil S, Ingalhalikar A:A novel crossed rod configuration incorporatingtranslaminar screws for occipitocervical internalfixation: an in vitro biomechanical study. Spine J11:30-35, 2011.
8. Goel A: Atlanto-axial joint distraction in the treat-ment of select cases of basilar invagination, syrin-gomyelia and fixed atlanto-axial dislocation. Nepal JNeurosci 2:1-6, 2005.
9. Goel A: Progressive basilar invagination after trans-oral odontoidectomy: treatment by atlantoaxialfacet distraction and craniovertebral realignment.Spine 30:E551-E555, 2005.
0. Goel A: Treatment of basilar invagination by atlan-toaxial joint distraction and direct lateral mass fixa-tion. J Neurosurg Spine 1:281-286, 2004.
1. Goel A, Achwal S: The surgical treatment for Chiarimalformation association with atlantoaxial disloca-tion. Br J Neurosurg 9:67-72, 1995.
2. Goel A, Bhatjiwale M, Desai K: Basilar invagination:a study based on 190 surgically treated patients. JNeurosurg 88:962-968, 1998.
3. Goel A, Gupta S: Vertebral artery injury with trans-articular screws. J Neurosurg 90:376-377, 1999.
4. Goel A, Laheri VK: Plate and screw fixation for at-lanto-axial subluxation. Acta Neurochir (Wien) 129:47-53, 1994.
5. Goel A, Muzumdar D, Dindorkar K, Desai K: Atlan-toaxial dislocation associated with stenosis of canalat atlas. J Postgrad Med 43:75-77, 1997.
6. Goel A, Shah A: Atlantoaxial joint distraction as atreatment for basilar invagination: a report of anexperience with 11 cases. Neurol India 56:144-150,2008.
7. Goel VK, Panjabi MM, Patwardhan AG, Dooris AP,Serhan H, American Society for Testing and Materi-als: Test protocols for evaluation of spinal implants.J Bone Joint Surg Am 88:103-109, 2006.
8. Gupta S, Goel A: Quantitative anatomy of the lateral
masses of the atlas and axis vertebrae. Neurol India48:120-125, 2000.1A
, FEBRUARY 2012 ww
9. Harms J, Melcher RP: Posterior C1-C2 fusion withpolyaxial screw and rod fixation. Spine 15:2467-2471, 2001.
0. Levine AM, Edwards CC: The management of trau-matic spondylolisthesis of the axis. J Bone Joint SurgAm 67:217-226, 1985.
1. McRae DL: Bony abnormalities in the region of fo-ramen magnum: correlation of the anatomic andneurologic findings. Acta Radiol 40:335-354, 1953.
2. Menezes AH: Primary craniovertebral anomaliesand hindbrain herniation syndrome (Chiari I): database analysis. Pediatr Neurosurg 23:260-269, 1995.
3. Menezes AH, VanGilder JC: Transoral-transpharyn-geal approach to the anterior craniocervical junc-tion. Ten-year experience with 72 patients. J Neuro-surg 69:895-903, 1988.
4. Moon SM, Ingalhalikar A, Highsmith JA, VaccaroAR: Biomechanical rigidity of an all-polyehterether-ketone anterior thoracolumbar spinal reconstruc-tion construct: an in vitro corpectomy model. SpineJ 9:330-335, 2009.
5. Papagelopoulos PJ, Currier BL, Hokari Y, Neale PG,Zhao C, Berglund LJ, Larson DR, An KN: Biome-chanical comparison of C1-C2 posterior arthrodesistechniques. Spine 32:E363–E70, 2007.
6. Pasztor E: Transoral approach for epidural cranio-cervical pathological processes. Adv Tech StandNeurosurg 12:125-170, 1985.
7. Patwardhan AG, Havey RM, Ghanayem AJ, DienerH, Meade KP, Dunlap B, Hodges SD: Load-carryingcapacity of the human cervical spine in compressionis increased under a follower load. Spine 25:1548-1554, 2000.
8. Spetzler RF, Dickman CA, Sonntag VK: The trans-oral approach to the anterior cervical spine. Con-temp Neurosurg 13:1-6, 1991.
9. Thiebaut F, Wackenheim A, Vrousos C: New me-dian sagittal pneuomostratigraphical finding con-cerning the posterior fossa. J Radiol Electrol 42:1-7,1961.
0. Wilke HJ, Wenger H, Claes L: Testing criteria forspinal implants: recommendations for the stan-dardization of in vitro stability testing of spinal im-plants. Eur Spine J 7:148-154, 1998.
onflict of interest statement: Dr. Roy Daniel, surgeonesign team, Globus Medical Inc; Aditya Muzumdar,mployee, Globus Medical Inc; Aditya Ingalhalikar,mployee, Globus Medical Inc; Mark Moldavsky, employee,lobus Medical Inc; and Saif Khalil, employee, Globusedical Inc.
eceived 25 February 2011; accepted 23 June 2011
itation: World Neurosurg. (2012) 77, 2:357-361.OI: 10.1016/j.wneu.2011.06.039
ournal homepage: www.WORLDNEUROSURGERY.org
vailable online: www.sciencedirect.com
878-8750/$ - see front matter © 2012 Elsevier Inc.ll rights reserved.
w.WORLDNEUROSURGERY.org 361