Biomanufacturing Laboratory, The University of Iowa, Iowa...
Transcript of Biomanufacturing Laboratory, The University of Iowa, Iowa...

Bioprinting scale-up tissue and organconstructs for transplantationIbrahim T. Ozbolat
Biomanufacturing Laboratory, The University of Iowa, Iowa City, IA, 52242, USA
Opinion
Bioprinting is an emerging field that is having a revolu-tionary impact on the medical sciences. It offers greatprecision for the spatial placement of cells, proteins,genes, drugs, and biologically active particles to betterguide tissue generation and formation. This emergingbiotechnology appears to be promising for advancingtissue engineering toward functional tissue and organfabrication for transplantation, drug testing, researchinvestigations, and cancer or disease modeling, and hasrecently attracted growing interest worldwide amongresearchers and the general public. In this Opinion, Ihighlight possibilities for the bioprinting scale-up of func-tional tissue and organ constructs for transplantation andprovide the reader with alternative approaches, theirlimitations, and promising directions for new researchprospects.
Bioprinting: a promising technology to revolutionizemedicineBioprinting can be defined as the spatial patterning ofliving cells and other biologics by stacking and assemblingthem using a computer-aided layer-by-layer depositionapproach to develop living tissue and organ analogs fortissue engineering, regenerative medicine, pharmacoki-netic, and other biological studies [1]. It uses fourapproaches to deposit living cells: inkjet [2], extrusion[3], acoustic [4] and laser [5] based. Given its great benefitin spatially arranging multiple cell types to recapitulatetissue biology, bioprinting is a game-changer in the rapiddevelopment of tissue constructs and is receiving enor-mous attention. Although bioprinting of functional 3Dwhole organs for transplantation remains in the realmof science fiction, the field is moving forward, providinghope that shortages in tissue grafts and organ transplan-tation will be mitigated to some extent in the future[6]. While current tissue-engineering strategies cannotenable fabrication of fully functional tissues or organs[7], bioprinting enables precise placement of biologics torecapitulate heterocellular tissue biology to some degree.Current technology enables the development of organ ortissue constructs that do not require substantial vascu-larization, as well as mini-tissue models mimicking the
0167-7799/
� 2015 Elsevier Ltd. All rights reserved. http://dx.doi.org/10.1016/j.tibtech.2015.04.005
Corresponding author: Ozbolat, I.T. ([email protected]).Keywords: bioprinting; bioprinting for transplantation; vascularized-tissue printing;in situ bioprinting.
biology of natural counterparts for pharmaceutical testingor cancer studies [8].
Here I present recent approaches to the bioprintingscale-up of functional tissue and organ constructs fortransplantation, including bioprinting vascularized tissueand organ constructs in vitro and in situ bioprinting tech-nology to build tissues directly in defect sites. I discussmajor roadblocks to this approach and provide potentialsolutions and future directions.
Bioprinting of vascularized tissue and organ constructsin vitro
Organ bioprinting holds great promise for the future, butwhole-organ bioprinting has remained elusive due toseveral limitations associated with biology, bioprintingtechnology, bioink material, and the post-bioprinting mat-uration process [9]. The bioprinting of functional tissues isan intermediate stage toward achieving organ-level com-plexity. In vitro fabrication of functional tissues is asophisticated phenomenon comprising a hierarchical ar-rangement of multiple cell types, including a multiscalenetwork of vasculature in stroma and parenchyma, alongwith lymphatic vessels and, occasionally, neural and mus-cle tissue, depending on the tissue type. In vitro engineeredtissue models that incorporate all of these components arestill far on the horizon. Bioprinting technology offers agreat benefit in the hierarchical arrangement of cells orbuilding tissue blocks in a 3D microenvironment, but thebioink and the post-bioprinting maturation phase are asimportant as the bioprinting process itself. The bioinkmaterial is crucial because it should provide the spectrumof biochemical (i.e., chemokines, growth factors, adhesionfactors, or signaling proteins) and physical (i.e., interstitialflow, mechanical and structural properties of extracellularmatrix) cues to promote an environment for cell survival,motility, and differentiation [10]. In addition, the bioinkshould exhibit high mechanical integrity and structuralstability without dissolving after bioprinting, enable dif-ferentiation of autologous stem cells into tissue-specific celllineages, facilitate engraftment with the endogenous tis-sue without generating an immune response, demonstratebioprintability with ease of shear thinning, rapid solidifi-cation and formability, and be affordable, abundant, andcommercially available with appropriate regulations forclinical use [11]. A variety of bioinks, including naturallyand synthetically derived materials, has been used fortissue regeneration, as detailed in the literature[12,13]. The post-bioprinting process is also crucial andnecessitates mechanical and chemical stimulation and
Trends in Biotechnology, July 2015, Vol. 33, No. 7 395

Opinion Trends in Biotechnology July 2015, Vol. 33, No. 7
signaling to regulate tissue remodeling and growth, thedevelopment of new bioreactor technologies enabling rapidmaturation of tissues, multiscale vascularization for sur-vivability of tissues, and mechanical integrity and inner-vation for transplantation.
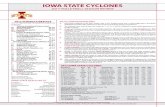
Although several researchers have studied bioprintingof tissue constructs, the fabrication of scale-up tissues witha high volumetric oxygen-consumption rate, such as cardi-ac, pancreas, or liver tissue, is still a challenge. One majorroadblock is associated with the integration of the vascularhierarchical network spanning arteries and veins down tocapillaries. To bioprint vascularized thick tissues, highlyrepeatable and straightforward technologies and protocolsshould be developed in logical steps, from simple to com-plex. Since it is difficult to print capillaries at the submi-cron scale using current technology, an alternative could beto bioprint the macrovasculature and then leave nature tocreate the capillaries. To this end, two alternativeapproaches have been considered: (i) indirect bioprintingby utilizing a fugitive ink that is removed by thermallyinduced decrosslinking, leaving a vascular network behind[14,15]; and (ii) direct bioprinting of a vasculature networkin a tubular shape [16–19] (Figure 1).
Several recent attempts have been made to bioprint afugitive bioink to create vascular channels [15,20–22]. Cellladen hydrogels were used to fabricate the tissue construct,and integration of the vascular network demonstratedincreased cell viability inside the construct; regions nearchannels exhibited significant differences compared withregions away from channels. Although most researchershave attempted to create a vascular network on a macro-scale and generate an endothelium lining inside the lumenvia gluing endothelial cells through perfusion, Lee et al.[21] took one step forward and successfully achieved an-giogenesis by sprouting endothelial cells within a fibrinnetwork loaded with other pericyte-like supporting cells(Figure 1A,B). Their study demonstrated that endothelialspouting generated a considerable increase in the perme-ability of the tissue construct. More advanced angiogenesisand vasculogenesis have already been developed in micro-fluidic devices; several supporting cells have beenattempted and used in cancer metastasis studies [23]. De-spite the flexibility in bioprinting channels and the abilityto create angiogenesis, this technology still faces majorchallenges. First, loading cells in hydrogels does not sup-port cell–cell interactions, because those take place in vivo,and limited phenotypic stability and activity of cells areobserved during prolonged in vitro incubation. Second,while fibrin is a suitable environment for angiogenesisbecause it has a crucial role in blood clotting [24], it isnot a convenient environment for tissue-specific cells, suchas islets in a pancreas or follicles in a lymph node; ascaffold-free environment should be considered for these.A recent article [25] demonstrated contiguous vasculariza-tion of cell aggregates in tumor spheroid models and robustangiogenesis into the fibrin matrix where spheroids wereencapsulated, showing the possibility of generating anas-tomosis of vascular networks of stromal and parenchymaltissues in vitro.
The other approach is direct bioprinting of a vascularnetwork via: (i) bioprinting of scaffold-free branched
396
vascular tubes [19] using tissue spheroids as buildingblocks [26] that are printed inside a mold pattern; and(ii) bioprinting of vasculature using direct extrusion of atubular network [16–18]. A recent study [3] demonstratedhybrid biofabrication of vasculature in tandem with tissuestrands, where fibroblast tissue strands quickly fuse toeach other, maturate, and form the tissue around thevasculature (Figure 1C–E). Tissue strands were madescaffold free and used as building blocks to construct thescale-up tissue due to their quick fusion, folding, andmaturation capabilities. This approach demonstrated theproof of concept toward larger-scale perfusable tissues;further work is needed to demonstrate a complex vascularnetwork within larger tissues with vascularization onmultiple scales that can be envisioned using a Multi-Arm BioPrinter [27]. Although vascularization is impor-tant for larger-scale tissue constructs for transplantation,anastomosis to the circulatory system and functionalitypost-transplantation should also be considered. The vas-cular network should be designed and bioprinted so that itcan be sutured to a vascular network easily, and it shouldhave certain properties, such as enough mechanical prop-erties to satisfy suture retention and burst pressure, suffi-cient intactness of endothelium to prevent thrombosis, anda high patency rate to support occlusion-free circulation[28]. Compared with indirect bioprinting of a vascularnetwork, the direct bioprinting of vasculature can be moreconvenient, suturing to the host at the time of implanta-tion.
From in vitro to in situ: regenerating tissues throughdirect bioprinting into defect sitesBioprinting living tissue constructs or cell laden scaffoldsin vitro has been well studied, and thin tissues or tissuesthat do not need vascularization, including skin, cartilage,and blood vessels, have been grown [12]. However, in situbioprinting can enable the growth of thick tissues in criticaldefects with the help of vascularization driven by nature inlesions. Therefore, it is a promising direction for the bio-printing of porous tissue analogs that can engraft withendogenous tissue and regenerate new tissue along withvasculogenesis through the migration of progenitor cellsinto the tissue construct and sprouting of capillaries fromthe endogenous tissue.
The idea of in situ bioprinting was first proposed byWeiss using inkjet technology [29]; however, translatingbioprinters into operating rooms was considered to bechallenging due to the perception that surgeons can beconsidered artists and prefer off-the-shelf solutions, suchas using prefabricated tissue constructs and cutting orcarving them into a form to be implanted into the defectsite. Limited research has been performed on in situ bio-printing since Weiss proposed this technology. Inkjet-based bioprinting of skin cells has been tested for burnwounds [30], and laser-assisted bioprinting has been per-formed to test the feasibility of printing nanohydroxyapa-tite particles on a mouse model [31]. The idea of bioprintingskin cells (fibroblasts and keratinocytes zonally) has beenconsidered feasible for transitioning the technology toclinical settings, with the hope of repairing major wounddefects of soldiers on the battlefield.

Vascular channels
Fibrin
Stage 1
(A)
(B)
(E)
(C)
(D)
Stage 2
Stage 3Stage 1 Stage 2 Stage 3
Embed endothelialand suppor�ng cells
Capillary network is formedwithin fibrin scaffold
Vasculature
Tissuestrands
Angiogenic sprou�ng is formedfrom vascular channels to thecapillary network
Assembly throughhybrid bioprin�ng
Par�al fusion of �ssuestrands around thevasculature
Complete fusion of �ssuestrands �ghtly adheringto the vasculature
Capillarynetwork
Sprou�ng
100µm
Endothelium
Collagen
Endothelial cellsKey:
Suppor�ng cells
Detachablenozzle
Co-axialnozzle
TRENDS in Biotechnology
Figure 1. Vascularized tissue construct bioprinting in vitro. In the first approach, (A) a fugitive ink is bioprinted to create vascular channels inside a collagen support
structure along with deposition of endothelial and fibroblast cells in a fibrin scaffold, resulting in capillary network formation in fibrin scaffold followed by endothelial
sprouting from vascular channel to capillary network in 9 days, where (B) a immunohistochemistry image shows integration of large sprouts from the parental vascular
channel (red) to the capillary network (green). In the second approach, (C) a hybrid bioprinting approach can be applied using a Multi-Arm BioPrinter, where (D) the tissue
assembly is created by placing the vasculature in the middle, resulting in fusion and maturation of scaffold-free tissue strands around the vasculature, further resulting in
(E) the tight fusion of the fibroblast tissue to the vasculature in 1 week [3]. The co-axial nozzle used in that study can enable continuous printing of a single lumen
vasculature throughout the fabrication of larger-scale hybrid tissue constructs. Reproduced and adapted, with permission, from [21] (B).
Opinion Trends in Biotechnology July 2015, Vol. 33, No. 7
In situ bioprinting is challenging, and further system-atic research is required to take the technology into arobust state. There are major limitations associated withits biological, biomaterial, and engineering aspects, such asprinting difficulties on nonhorizontal surfaces, the need forhighly advanced robotics bioprinters coupled with comput-er-aided design technologies (i.e., scanning the defect siteand providing an interactive user interface for surgeons),the requirement for a highly effective extrudable bioinkenabling instant solidification in a living body (without theneed for an external solidifier, such as a ultraviolet light ora chemical crosslinker), the need for a biologically appeal-ing ink for enhanced tissue formation, the requirement fortechnologies that do not interfere with in vivo conditions
and regulatory issues related to animals or humans neces-sitating safe delivery of the tissue construct under anes-thesia. In addition, in situ bioprinting can sometimesincrease the duration and cost of surgery.
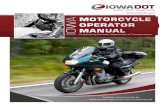
Bioprinting ex vivo on explants can be considered atransitional stage (Figure 2A) in which tissue constructscan be built and engineered inside explants [32]. In situbioprinting is promising for developing tissue analogsdirectly on the defect model in operating rooms(Figure 2B), which paves the way to developing associatedenabling technologies for humans in the future. When thetechnology is translated into clinics, it will have severalbenefits: (i) direct bioprinting of tissue constructs intodefects can eliminate the need for preshaping or reshaping
397

TRENDS in Biotechnology
Bioprinternozzle
Defect
Explant
Fixture
Bioprinter
Bioprinternozzle
Stem cellsPlasmid
DNA
Bioink
Biodegradablemicropar�cle
Bioprinternozzle
Calvarialdefects
Rat
In situbioprin�ng
Printedcells
Cells migra�ngfrom defect
Printed �ssue inside acar�lage defect
In situ hybridbioprin�ng in
opera�ng roomsLarge
defects
Dura subs�tute(biological or
syneth�c)Printed frame
made ofbiodegradablehard polymer
Printedhydrogel
compositeloaded with
stem cells andgenes
(C)
(A) (B)
Figure 2. In situ bioprinting. (A) Bioprinting cells into explants in situ can be considered an intermediate step toward (B) bioprinting tissue constructs directly into animal
models, where DNA can also be printed for bioprinting mediated gene therapy to transfect and differentiate printed stem cells into multiple lineages. This will have a great
impact on (C) transitioning in situ bioprinting technology into operating rooms for humans in the near future; for example, large, deep calvarial defects can be regenerated
on a synthetic or biological Dura substitute, where a hard polymeric biodegradable frame can be printed along with stem cells and genes loaded in hydrogels to generate
the vascularized bone tissues. Image in (C) reproduced courtesy of Christopher Barnatt.
Opinion Trends in Biotechnology July 2015, Vol. 33, No. 7
the scaffold based on the defect geometry. This can avoidthe laborious nature of scaffold preparation and the risksassociated with contamination and limited activity of cellsin vitro; (ii) for bioprinting of cell-laden tissue constructsfor critical- or large-size defects, in situ bioprinting caneliminate the need for differentiation of stem or progenitorcells in vitro, which might be expensive and time consuming.
398
When bioprinting stem or progenitor cells in situ, cells areexposed to the natural environment with growth factors thatcan induce their differentiation into the desired lineages;(iii) in situ bioprinting can enable the precise deposition ofcells, genes, or cytokines inside the defect, unlike manualinterventions, such as prefabricated scaffolds, in which theshape can alter due to swelling, contraction, or deformations.

Opinion Trends in Biotechnology July 2015, Vol. 33, No. 7
Localized control via bioprinting, such as printing differentcytokines at different layers, is an asset for future bioprint-ing research; (iv) standard defects made by surgery tools areeasily addressed by manipulation and bioprinting of tissueanalogs. However, naturally occurring defects resultingfrom trauma, surgical excision, or other issues are randomin morphology and geometry and need to be captured pre-cisely; laser- or image-based scanning systems can overcomethis challenge. In situ bioprinting can eliminate the need formultiple operations because the tissue constructs can bebioprinted into the defect immediately; and (v) twistingmulti-axis robotic arms can enable angled deposition andprinting of the bioink into nonhorizontally oriented defects.Defects on the live model can be at random locations, and it isnot convenient for the surgeon to change the position of theanesthetized model during bioprinting.
As a result of these benefits, in situ bioprinting of tissueanalogs can be applied to various sites on the body, such asdeep dermal or extremity injuries and calvarial or cranio-facial defects during maxillofacial or neurosurgeries. In thefuture, in situ bioprinting technology could be consideredfor humans (Figure 2C). For large calvarial defects thatneed a great deal of microvascularization along with struc-tural support, one can envision bioprinting a frame (usinghard osteoconductive polymers, such as a blend of poly-caprolactone, copolymers, and hydroxyapatite) in tandemwith stem cells (loaded in blends of hydrogels, such ascollagen and fibrin) to be differentiated toward multiplelineages, including osteoblasts and endothelial cells forbone generation and angiogenesis, respectively [33]. Insitu bioprinting of porcine aortic endothelial cells in fibringel has already demonstrated vascularization in the sub-cutaneous tissue of mice 1 week after implantation [34]. Inanother long-term future application, in situ bioprintingcould assist placement of different cell types in differentcompartments in large, deep defects for composite tissueregeneration, where manual surgical interventions arerequired for suturing supplement blood vessels and nerves.In that case, bioprinting can be performed with a deposi-tion head mounted on a six-axis robotic arm controlled bythe surgeon. The printed bioink should have a highlyporous microstructure or could be mixed with a sacrificial(quickly bioresorbable) biomaterial, leaving porosity upontransplantation, which would enable diffusion and inter-stitial flow of blood for survivability of cells until neovas-cularization is completed. A major challenge is the lack ofgrowth factors far from the defect periphery, which areneeded to induce differentiation of printed stem cells orprogenitor cells that migrate from the host tissue. This canbe overcome with gene therapy, where gene delivery can besustained and controlled using gene-activated matrices(GAMs), such as microparticles loaded with genes, forthe long-term release of genes for the transduction anddifferentiation of autologous cells into multiple lineages[35]. Printing nonviral vectors in GAMs is safe and efficientfor transfecting target cells and surpasses the benefits ofdirect delivery of growth factors during in situ bioprinting.
Concluding remarksHere, I present the state of the art in bioprinting technologyfor biofabrication of scale-up tissue and organ constructs.
Two approaches are discussed: (i) in vitro bioprinting oftissue and organ constructs with a focus on alternativetechnologies in bioprinting a multiscale vascular networkin tandem with the rest of the tissue construct, and (ii) in situbioprinting of tissue construct for regeneration of largedefects that will one day enable the repair of body partsdirectly in patients in operating rooms. Although the tech-nology shows a great deal of promise for bioprinting atorgan-level complexity, there is still a long way to go torealize this ambitious vision. There is a need for advance-ment in several areas, including new cell sources and stemcell technology, novel bioinks, and advanced fully automat-ed bioprinter technologies and bioprinting processes. Over-coming current impediments in these technologies alongwith advancements in in vivo integration is essential fordeveloping seamlessly automated technology from autolo-gous stem cell isolation to tissue or organ construct trans-plantation.
AcknowledgmentsThis work has been supported by National Science Foundation AwardsCMMI 1462232, CAREER 1349716, Diabetes in Action Research andEducation Foundation, and the Grow Iowa Values Funds. The authorwould like to express his gratitude to G. Dai, Christopher Barnatt, YinYu, and Kerim Moncal for providing some of the high-quality images inthe figures.
References1 Guillemot, F. et al. (2010) Bioprinting is coming of age: report from the
International Conference on Bioprinting and Biofabrication inBordeaux (3B’09). Biofabrication 2, 010201
2 Xu, C. et al. (2014) Study of droplet formation process during drop-on-demand inkjetting of living cell-laden bioink. Langmuir 30, 9130–9138
3 Yu, Y. et al. (2014) A hybrid bioprinting approach for scale-up tissuefabrication. J. Manuf. Sci. E-T. 136, 061013
4 Gurkan, U.A. et al. (2014) Engineering anisotropic biomimeticfibrocartilage microenvironment by bioprinting mesenchymal stemcells in nanoliter gel droplets. Mol. Pharmaceutics 11, 2151–2159
5 Guillemot, F. et al. (2011) Laser-assisted bioprinting to deal with tissuecomplexity in regenerative medicine. MRS Bull. 36, 1015–1019
6 Dababneh, A.B. and Ozbolat, I.T. (2014) Bioprinting technology: acurrent state-of-the-art review. J. Manuf. Sci. E-T. 136, 061016
7 Atala, A. et al. (2012) Engineering complex tissues. Sci. Transl. Med. 4,160rv112
8 Melchels, F.P.W. et al. (2012) Additive manufacturing of tissues andorgans. Prog. Polym. Sci. 37, 1079–1104
9 Ozbolat, I.T. and Yin, Y. (2013) Bioprinting toward organ fabrication:challenges and future trends. IEEE Trans. Biomed. Eng. 60, 691–699
10 Griffith, L.G. and Swartz, M.A. (2006) Capturing complex 3D tissuephysiology in vitro. Nat. Rev. Mol. Cell Biol. 7, 211–224
11 Murphy, S.V. et al. (2013) Evaluation of hydrogels for bio-printingapplications. J. Biomed. Mater. Res. A 101A, 272–284
12 Murphy, S.V. and Atala, A. (2014) 3D bioprinting of tissues and organs.Nat. Biotech. 32, 773–785
13 Derby, B. (2012) Printing and prototyping of tissues and scaffolds.Science 338, 921–926
14 Lee, V.K. et al. (2014) Creating perfused functional vascular channelsusing 3D bio-printing technology. Biomaterials 35, 8092–8102
15 Kolesky, D.B. et al. (2014) Bioprinting: 3D bioprinting of vascularized,heterogeneous cell-laden tissue constructs. Adv. Mater. 26, 2966
16 Zhang, Y. et al. (2013) Characterization of printable cellular micro-fluidic channels for tissue engineering. Biofabrication 5, 024004
17 Zhang, Y. et al. (2013) Direct bioprinting of vessel-like tubularmicrofluidic channels. J. Nanotechnol. Eng. Med. 4, 021001
18 Dolati, F. et al. (2014) In vitro evaluation of carbon-nanotube-reinforced bioprintable vascular conduits. Nanotechnology 25,145101
19 Norotte, C. et al. (2009) Scaffold-free vascular tissue engineering usingbioprinting. Biomaterials 30, 5910–5917
399

Opinion Trends in Biotechnology July 2015, Vol. 33, No. 7
20 Bertassoni, L.E. et al. (2014) Hydrogel bioprinted microchannelnetworks for vascularization of tissue engineering constructs. LabChip 14, 2202–2211
21 Lee, V. et al. (2014) Generation of multi-scale vascular network systemwithin 3D hydrogel using 3D bio-printing technology. Cell. Mol. Bioeng.1–13
22 Miller, J.S. et al. (2012) Rapid casting of patterned vascular networksfor perfusable engineered three-dimensional tissues. Nat. Mater. 11,768–774
23 Zervantonakis, I.K. et al. (2012) Three-dimensional microfluidic modelfor tumor cell intravasation and endothelial barrier function. Proc.Natl. Acad. Sci. U.S.A. 109, 13515–13520
24 Janmey, P.A. et al. (2009) Fibrin gels and their clinical andbioengineering applications. J. R. Soc. Interface 6, 1–10
25 Ehsan, S.M. et al. (2014) A three-dimensional in vitro model of tumorcell intravasation. Integr. Biol. 6, 603–610
26 Mironov, V. et al. (2009) Organ printing: tissue spheroids as buildingblocks. Biomaterials 30, 2164–2174
27 Ozbolat, I.T. et al. (2014) Development of ‘Multi-arm Bioprinter’ forhybrid biofabrication of tissue engineering constructs. Robot. Comput.Integr. Manuf. 30, 295–304
400
28 Quint, C. et al. (2011) Decellularized tissue-engineered bloodvessel as an arterial conduit. Proc. Natl. Acad. Sci. U.S.A. 108,9214–9219
29 Campbell, P.G. and Weiss, L.E. (2007) Tissue engineering with the aidof inkjet printers. Expert Opin. Biol. Ther. 7, 1123–1127
30 Skardal, A. et al. (2012) Bioprinted amniotic fluid-derived stem cellsaccelerate healing of large skin wounds. Stem Cells Transl. Med. 1,792–802
31 Keriquel, V. et al. (2010) In vivo bioprinting for computer- and robotic-assisted medical intervention: preliminary study in mice.Biofabrication 2, 014101
32 Cui, X. et al. (2012) Direct human cartilage repair using three-dimensional bioprinting technology. Tissue Eng. Part A 18,1304–1312
33 Temple, J.P. et al. (2014) Engineering anatomically shapedvascularized bone grafts with hASCs and 3D-printed PCL scaffolds.J. Biomed. Mater. Res. A 102, 4317–4325
34 Xu, T. et al. (2008) Inkjet-mediated gene transfection into living cellscombined with targeted delivery. Tissue Eng. Part A 15, 95–101
35 Evans, C.H. (2012) Gene delivery to bone. Adv. Drug Deliv. Rev. 64,1331–1340