BIOL226Lec11 Scrotum,Prostate
-
Upload
drravikumar-bhandari -
Category
Documents
-
view
230 -
download
0
Transcript of BIOL226Lec11 Scrotum,Prostate
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
1/30
PROSTATE GLAND
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
2/30
I. Introduction/General Information
A. Attached inferiorly to urinary bladder by
ligaments
B. Posterior to pubic symphysis
C. Surrounds superior portion of urethraD. Anterior to rectum (palpation, ultrasound)
E. Conical shape
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
3/30
Introduction, Prostate Gland, continued
F. Walnut sized
1. 4 cm trans x 2 cm A/P x 3 cm Sup/Inf
G. Lightly encapsulated
1. Fibrous connective tissue
2. Smooth muscle3. Capsule extends into lobes
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
4/30
II. Prostate Gland: Detailed Anatomy
A. Largest male
accessory
gland
B. Located in
subperitoneal
compartment(between pelvicdiaphragm &
peritoneum)Prostate Gland, Mid-sagittal Section
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
5/30
Prostate Gland: Detailed Anatomy
C. Enclosed in fascial sheath
(aka: prostatic sheath)
1. Inferiorly, sheath is continuous
with superior fascia of
urogenital diaphragm
2. Posteriorly, sheath forms part of
retrovesical septum
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
6/30
Prostate Gland: Detailed Anatomy
D. Double Capsule
1. Fibrous portion contacts gland2. External capsule formed by pelvic
fascia
3. Venous plexus lies between
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
7/30
Male Reproductive System, Posterior View
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
8/30
Detailed Anatomy, contined
E. Conical shape with base (sup), apex (inf),
four surfaces
1. Surfaces: posterior, anterior, right &left inferolateral
2. Base (aka: vesicular surface): superior
a. Attached to neck of urinary bladder
b. Prostatic urethra enters middle of
base close to anterior surface
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
9/30
Prostate Anatomy
Prostatic Urethra
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
10/30
Detailed Anatomy, contined
3. Apex: inferiora. Rests on superior fascia of urogenital
diaphragm muscle
b. Associated with sphincter urethraec. Contacts medial margins oflevator ani
muscles
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
11/30
Detailed Anatomy, contined
4. Posterior surface: triangular, flat
5. Anterior surface: narrow, convex
6. Inferiorolateral surfaces
a. Meet with anterior surface
b. Rest on levator ani fascia above
urogenital diaphragm
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
12/30
Detailed Anatomy, contined
F. Lobes of the Prostate
1. Divisions are arbitrary, indistinct
2. Usually divided into
a. two lateral lobesb. one median lobe
c. anterior and posterior lobes
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
13/30
Lobes of the Prostate, continued
3. Median lobe
a. Lies posterior and superior toprostatic utricle and ejaculatory
ducts
b. May project into urinary bladder
c. Utricle lies within lobe1. Vestigial remains of uterine
homolog
2. Sometimes called uterus
masculinis
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
14/30
Lobes of the Prostate, continued
4. Lateral lobes
a. Comprise the greatest mass ofthe gland
b. Contain most secretory tissue
c. Are continuous posteriorly
5. Glandular tissue with varying amounts
of fibrous tissue
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
15/30
Lobes of the Prostate, continued
Prostate Glandin situ
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
16/30
Detailed Anatomy, continued
G. Blood & lymph
1. Arteries derived
from:
a. Internal pudendalartery
b. Inferior vesicalartery
c. Middle rectalartery
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
17/30
Blood & Lymph, continued
2. Veins
a. Form venous plexusb. Drain into internal iliac veins
c. Communicate with vesical &
vertebral venous plexuses
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
18/30
Blood & Lymph, continued
3. Lymphatics
a. Most terminate in internal iliac &sacral nodes (unable to palpate)
b. From posterior: to external iliac
nodes (unable to palpate)
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
19/30
Detailed Anatomy, contined
H. Glandular tissue
1. 30 - 50 different glandular elements
a. Serous glands
b. 20 - 30 ducts empty into prostaticurethra
2. Most are posterior & lateral to urethra
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
20/30
Blood & Lymph, continued
3. Prostatic secretionsa. Thin, milky, alkaline (looks like
skim milk)
b. Discharged at ejaculation
c. Make up ~ 1/3 of semen
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
21/30
Detailed Anatomy, continued
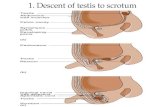
I. Prostate size changes
1. Small at birth2. Enlarges at puberty
3. Maximum at about 13
4. Progressive enlargement after 40
5. Sometimes: undergoes atrophy
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
22/30
III. Pathology
A. Benign
prostatichypertrophy
(BPH):
1. Affects ~90%
of men >50
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
23/30
BPH, continued
2. Common cause of urethral obstruction:
causes
a. Nocturiab. Dysuria
c. Urgency
d. Back-pressure effects
e. Complete obstruction can occur
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
24/30
Pathology, continued
B. Prostate cancer1. Most common
cancer in males
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
25/30
Pathology, continued
2. Metastasizes via blood (hematogenous)
or lymph (lymphogenous)3. Common sites: vertebrae, pelvis
a. Via venous plexus surrounding
prostateb. Bone or direct metastasis most
common
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
26/30
Prostate Cancer: Routes of Metastasis
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
27/30
Pathology, continued
C. Prostatitis (accompanied by cystitis)
1. Inflammation of gland
2. Gland enlarges, becomes tender
3. Causes: gonorrhea? Other UTIs?
STDs?
4. May require antibiotics, massage5. Symptoms: chills, painful urination,
back pain
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
28/30
Pathology, continued
A. Prostatic concretions (aka: corporaamylacea [starch bodies])
1. Small spherical or ellipsoid bodies
2. Number increases with age
3. May become calcified as male ages4. May simulate carcinoma
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
29/30
Digital Rectal Exam
-
7/28/2019 BIOL226Lec11 Scrotum,Prostate
30/30
Pathology, continued
E. Rarely, prostatic abscesses develop1. Frequently caused by gonorrhea2. May rupture through to rectum, bladder,
perineum
3. Other causes:a. Urethritis
b. Epididymitis















![Untitled-7 []include the growth and maturation of the prostate, seminal vesicles, penis, and scrotum; the development of male hair distribution, such as facial, pubic, chest, and axillary](https://static.fdocuments.net/doc/165x107/5f869ea8989b5908de490aa5/untitled-7-include-the-growth-and-maturation-of-the-prostate-seminal-vesicles.jpg)

