Accelerated Bridge Construction (ABC) Accelerated Bridge ...
Bilateral Papillophlebitis in a Patient with Accelerated Essential Hypertension
-
Upload
arijit-mitra -
Category
Documents
-
view
215 -
download
1
Transcript of Bilateral Papillophlebitis in a Patient with Accelerated Essential Hypertension
C A S E R E P O R T
Bilateral Papillophlebitis in a Patient withAccelerated Essential Hypertension
ARIJIT MITRA, DO, MRCSEdA B S T R A C T
We describe a case of bilateral papillophlebitis with discedema, scattered cotton-wool spots, flame-shaped hemor-rhages, and exudates around the optic discs and in themacula of a 33-year-old patient with essential hyperten-sion. The pathophysiology and natural course of the diseaseis discussed.
INTRODUCTION
Central retinal vein occlusion (CRVO) is usually seen
in older adults and is often associated with systemic
vascular disease. Inflammation of the central retinal
vein has been proposed as a cause of the occlusion in
young adults and, for that reason, it has been called
papillophlebitis. We report a case of bilateral
papillophlebitis in a 33-year-old healthy male with
accelerated essential hypertension. The pathophysi-
ology and natural course of the condition is discussed.
CASE REPORT
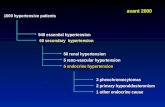
A 33-year-old healthy male patient presented to the
Emergency Department with mild loss of vision in the
left eye. He had high myopia and was a contact lens
wearer. On presentation, the best corrected vision in
the right eye was 6/9 and in the left eye it was 6/12. He
had no history of headaches or medical problems, was
not on any medications, and had no significant ocular
history in the past. Anterior segment examination and
intraocular pressures were within normal limits.
There was no relative afferent papillary defect. Fun-
dus examination showed bilateral papillophlebitis,
with disc edema, scattered cotton-wool spots, flame-
shaped hemorrhages, and exudates around the optic
discs and in the macula. The fovea was largely spared
in both eyes (Figs. 1 and 2). There was no evidence of
long-standing hypertensive retinopathy changes.
Blood pressure readings in the Emergency Depart-
ment were 246/136 mm Hg. Capillary blood sugar
R E P R I N T SArijit Mitra, DO, MRCSEd, Specialist Registrar, Wolverhampton and Midland
Counties Eye Infirmary, Compton Road, Wolverhampton, West Midlands WV3
9QR, UK. E-mail: [email protected].
The author has stated that he does not have a significant financial interest or
other relationship with any product manufacturer or provider of services dis-
cussed in this article. The author also does not discuss the use of off-label
products, which include unlabeled, unapproved, or investigative products or
devices.
The author describes a case of bilateral papillophlebitis in a patient with
essential hypertension in which significant visual improvement is seen following
stabilization of the blood pressure.
Submitted for publication: 3/12/07. Accepted: 6/29/07.
Annals of Ophthalmology, vol. 39, no. 4, Winter 2007
� Copyright 2007 by ASCO
All rights of any nature whatsoever reserved.
1530-4086/07/39:337–339/$30.00. ISSN 1558-9951 (Online)
ANN OPHTHALMOL. 2007;39 (4) ..............................................337
level was normal. The patient was admitted to the
Medical Assessment Unit, where he underwent
extensive blood investigations and had an ultrasound
scan of the kidneys to rule out any secondary causes
of hypertension. No apparent cause was detected
from the investigations and the patient was treated
for essential hypertension. No other end-organ dam-
age was detected.
Within two weeks, the patient’s blood pressure
stabilized to around 150/100 mm Hg with treatment.
His vision improved to 6/4 in the right eye and 6/5 in
the left. Fundoscopy revealed fewer exudates, cotton-
wool spots, and flame-shaped hemorrhages.
DISCUSSION
A hypertensive emergency is a condition in which
elevated blood pressure results in target organ dam-
age. The systems primarily involved include the cen-
tral nervous system, the cardiovascular system, the
kidneys, and the retina. Hypertensive urgency must
be distinguished from emergency. Urgency is defined
as severely elevated blood pressure (i.e., sys-
tolic>220 mm Hg or diastolic>120 mm Hg) with
no evidence of target organ damage. Hypertensive
emergencies require immediate therapy to decrease
the blood pressure within minutes to hours. In con-
trast, no evidence suggests a benefit from rapidly
reducing the blood pressure in patients with hyper-
tensive urgency. In fact, such aggressive therapy may
harm the patient, resulting in cardiac, renal, or cere-
bral hypoperfusion.
The pathogenesis of accelerated hypertension is not
fully understood. The characteristic vascular lesion is
the fibrinoid necrosis of arterioles and small arteries,
which causes the clinical manifestations of end-organ
damage. Red blood cells are damaged as they flow
through vessels obstructed by fibrin deposition,
resulting in microangiopathic hemolytic anemia. In
patients without hypertension, flow is kept constant
over a mean pressure of 60–120 mm Hg. In patients
with hypertension, flow is constant over a mean
pressure of 110–180 mm Hg because of arteriolar
thickening. When blood pressure is raised above the
upper limit of autoregulation, arterioles dilate. This
results in hyperperfusion and end-organ damage.
Papillophlebitis is the term that is often used to
describe a CRVO with preserved visual acuity in a
young patients (1), typically under the age of
50 years. Historically, papillophlebitis has been re-
ferred to as big blind spot syndrome (BBSS), benign
retinal vasculitis, presumed phlebitis of the optic disc,
optic disc vasculitis, and non-ischemic CRVO. While
CRVO develops in elderly patients due to arteriolo-
sclerosis and thrombus formation, this does not seem
to be the case in papillophlebitis. It is thought that the
underlying lesion is optic disc swelling with resultant
secondary venous congestion. Histopathological sec-
tions in papillophlebitis have demonstrated extensive
phlebitis and obliteration of lumens of arterioles and
mononuclear inflammatory infiltration of the central
retinal veins.
Papillophlebitis is usually unilateral. The patient
with papillophlebitis is generally healthy. Hyperten-
sion has been noted in 23–42% of patients with pa-
pillophlebitis. Diabetes has been found in only 3–9%
of patients. Hyperlipidema, hyperviscosity, and
hypercoagulable states have not been found in pa-
tients with papillophlebitis in greater incidence than
age-matched controls.
Fundus fluorescein angiographic findings include
dilated and tortuous retinal veins, prominent vascular
staining, blocked fluorescence, microaneurysms, disc
Figure 1—Right eye showing papillophlebitis with mildinvolvement of the fovea.
Figure 2—Left eye showing papillophlebitis without involve-ment of the fovea.
ANN OPHTHALMOL. 2007;39 (4) ..............................................338
edema, and peripapillary dye spillage. Typically, pa-
pillophlebitis is a non-ischemic occlusion that can be
expected to resolve in three to six months. Monthly
observation (preferably with ocular photography) is
indicated.
Occasionally, however, as with true CRVO, papil-
lophlebitis may develop extensive areas of retinal
non-perfusion with subsequent neovascularization of
the posterior or anterior segment and neovascular
glaucoma (2). Most eyes recover vision to better than
20/40, about one-fifth have significant visual loss, and
many suffer ocular sequelae (3). Although many
treatment modalities have been attempted for this
entity, no conclusive evidence exists that any treat-
ment alters its natural history.
Although young patients with CRVO usually
present with no history of contributory systemic dis-
ease, a thorough physical examination may prevent
life-threatening complications, as has been high-
lighted by this case. To the best of our knowledge,
bilateral papillophlebitis secondary to accelerated
hypertension has not been reported before. The nat-
ural clinical course of this condition is one of spon-
taneous resolution and treatment is usually
unnecessary (4). However, all of these patients
should be referred to a primary care physician for
systemic evaluation. If any abnormalities are found,
they must be aggressively treated.
REFERENCES
1. D’Amato RJ, Miller NR, Fine SL, et al. The effect of age and
initial visual acuity on the systemic and visual prognosis of central
retinal vein occlusion. Aust N Z J Ophthalmol 1991;19:118–122.
2. Sachdev MS, Sood NN, Mohan M, et al. Optic disc vasculitis in
epidemic dropsy. Jpn J Ophthalmol 1987;31:467–474.
3. Fong AC, Schatz H. Central retinal vein occlusion in young adults.
Surv Ophthalmol 1993;37:393–417. Erratum in: Surv Ophthalmol
1993;38:88.
4. McLoone EM, Best RM. Pregnancy-related papillophlebitis. Eur J
Ophthalmol 2004;14:65–66.
ANN OPHTHALMOL. 2007;39 (4) ..............................................339