BASIC LIFE SUPPORT NurseWest - Amazon S3€¦ · NurseWest ge 4 Section one: Basic Life Support...
Transcript of BASIC LIFE SUPPORT NurseWest - Amazon S3€¦ · NurseWest ge 4 Section one: Basic Life Support...

health.wa.gov.au
BASIC LIFE SUPPORT
NurseWest

NurseWest
Pa
ge2
Contents
PURPOSE .......................................................................................................................................................................................... 3
SECTION ONE: BASIC LIFE SUPPORT CHAIN OF SURVIVAL ................................................................................................. 4
SECTION TWO: DISCOVERING A COLLAPSED PATIENT ........................................................................................................ 6
DANGERS? ............................................................................................................................................................................................... 6 RESPONSIVE? .......................................................................................................................................................................................... 6 SEND FOR HELP ....................................................................................................................................................................................... 6 OPEN AIRWAY .......................................................................................................................................................................................... 7 NORMAL BREATHING? ............................................................................................................................................................................. 7 START CPR ............................................................................................................................................................................................. 7 ATTACH DEFIBRILLATOR .......................................................................................................................................................................... 8
SECTION THREE: OPEN AIRWAY................................................................................................................................................. 9
SECTION FOUR: NORMAL BREATHING? .................................................................................................................................. 11
SECTION FIVE: START CPR ......................................................................................................................................................... 12
COMPRESSIONS ..................................................................................................................................................................................... 12 POSITION OF HANDS ............................................................................................................................................................................... 12 DEPTH OF COMPRESSION ...................................................................................................................................................................... 13 RATE (SPEED) OF COMPRESSION ........................................................................................................................................................... 13 FATIGUE ................................................................................................................................................................................................. 13 RESCUE BREATHS .................................................................................................................................................................................. 14 MOUTH TO MOUTH RESCUE BREATHING ................................................................................................................................................. 15
SECTION SIX: SPECIAL CIRCUMSTANCES .............................................................................................................................. 16
PREGNANCY ........................................................................................................................................................................................... 16 FOREIGN BODY AIRWAY OBSTRUCTION (CHOKING) ............................................................................................................................... 17
Management of Foreign Body Airway Obstruction .................................................................................................................... 18
SECTION SEVEN: INFANTS AND CHILDREN ............................................................................................................................ 19
AIRWAY................................................................................................................................................................................................... 19 INITIAL BREATHS ..................................................................................................................................................................................... 20 EXTERNAL CARDIAC COMPRESSIONS .................................................................................................................................................... 21 POSITION OF COMPRESSION .................................................................................................................................................................. 21 DEPTH OF COMPRESSION ...................................................................................................................................................................... 21 RATE OF COMPRESSION ......................................................................................................................................................................... 22 CHOKING CHILD ...................................................................................................................................................................................... 22
Summary of CPR in Infants and Children ................................................................................................................................... 24
SUMMARY ....................................................................................................................................................................................... 25
REFERENCES ................................................................................................................................................................................. 25
Appendix 1: ARC and NZRC BLS Algorithm 2010 ..................................................................................................................... 26

NurseWest
Pa
ge3
These symbols will guide you through the Self Directed Learning Package (SDLP):
PURPOSE
Welcome to the Basic Life Support Resource. This package is designed to assist healthcare workers with direct patient contact to prepare for achieving competency in Basic Life Support (BLS). For details of Fremantle Hospital and Health Services (FHHS) guidelines, competencies and policies on cardiopulmonary resuscitation (CPR) please refer to the Nursing Practice Manual.
Aim
The aim of this resource is to facilitate the growth of a comprehensive knowledge and skills base in the area of BLS and as such other resources should be utilised. Further resources available to staff include:
Copies of the Australian Resuscitation Council (ARC) guidelines that are available from the ARC Website: www.resus.org.au
Reading material suggested at the conclusion of each section
Learning Outcomes
After studying this package you will be able to: discuss the importance of BLS in the Chain of Survival assess and manage the airway of the unresponsive patient assess for normal breathing and perform external cardia compressions and
ventilation on a collapsed patient perform BLS in accordance with ARC guidelines.
Assessment
After reading this resource you may complete the theory quiz and then arrange to complete the practical assessment.
Module Summary Take some time out
Required Reading Important information

NurseWest
Pa
ge4
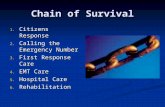
Section one: Basic Life Support Chain of Survival
Figure 1 Chain of survival
(Morley et al, 2006, p. 1)
The interventions that contribute to a successful outcome after cardiac arrest can be conceptualised as a chain – the Chain of Survival (Morley et al, 2006). The chain is only as strong as its weakest link.
1. Early Recognition. Someone suspects or determines the patient is in danger or is in sudden cardiac arrest and calls for emergency assistance.
2. Early CPR. Effective cardiopulmonary resuscitation maintains a cardiac output and oxygenation until more definitive measures become available.
3. Early Defibrillation. Someone trained in defibrillation shocks the patient as quickly as possible when required.
4. Post Resuscitation Care. Trained personnel provide advanced care, which may include airway support, medications and other hospital services

NurseWest
Pa
ge5
The purpose of CPR is to temporarily maintain a circulation sufficient to preserve brain function until Advanced Life Support (ALS) measures commence. In victims who need resuscitation, bystander CPR dramatically increases the chance of survival.
Cardiopulmonary Resuscitation can be separated into two components:
External Cardiac Compression (ECC)
Rescue Breathing
ANY ATTEMPT AT RESUSCITATION
IS BETTER THAN NO ATTEMPT

NurseWest
Pa
ge6
Section two: Discovering a Collapsed Patient
Upon discovering a collapsed patient it is recommended that the rescuer follow the established pathway determined by the acronym: DRSABCD
D Dangers? Please see the Basic Life Support Algorithm on page 23 for further detail
R Responsive?
S Send for help
A Open Airway
B Normal Breathing?
C Start CPR
D Attach Defibrillator
Dangers?
In the first instance the rescuer should ensure it is safe to commence resuscitation and not put themselves at risk of ill health or death. In the second instance the safety of subsequent rescuers should be considered and then finally the safety of the patient. If the rescuer determines that the situation is safe and progresses to full resuscitation they should also bear in mind that circumstances can change. If the circumstances change detrimentally to the rescuer’s health then thought should be given to discontinuing the resuscitation.
Responsive?
It is important to determine if the patient is conscious or unconscious. This can be done by tactile and verbal stimulation. Squeeze the patient’s shoulders and ask such simple questions as “Are you OK?” “What is your name?’ or “Can you squeeze my hand?”.
Send for Help
If the patient is responsive they should be placed in the lateral position and assistance sought. If the patient proves to be unresponsive they can therefore be considered as unconscious and assistance should be sought.
It is extremely difficult to reverse the underlying causes of cardiac arrest with simple BLS. Treating and reversing the underlying cause will require ALS measures. It is therefore imperative that help is summoned.

NurseWest
Pa
ge7
Open Airway
Assessment of the airway and steps to establish a patent airway should be followed as discussed in Section three.
Normal Breathing?
Assess whether the patient is breathing normally and if not commence CPR immediately as explained in Section four.
Start CPR
In the event that the patient is unresponsive and not breathing normally, then External Cardiac Compressions (ECC) should commence immediately in combination with rescue breathing, with a ratio of 30 compressions to 2 breaths. This combination of rescue breathing and ECC is known as CPR. Further details are provided in Section five.
Hospital
Press emergency nurse call button if available
Press nurse call bell three times
Dial 55 and state “Code Blue” and the exact location
Community
Call 000 – state the nature and exact location of the emergency
(112 can be used for mobile phones in rural and
remote locations)
CPR should be commenced immediately if the patient is
unresponsive and not breathing normally
Compression to Ventilation ratio
Compressions 30:2 Breaths

NurseWest
Pa
ge8
Attach Defibrillator
The likelihood of successful defibrillation decreases rapidly with time. A defibrillator should be attached to the collapsed patient as soon as available and utilised to analyse the need for defibrillation. Good CPR may increase the likelihood of defibrillation occurring and interruptions to CPR for attachment of leads, rhythm analysis etc. should be minimised. In the event of an out of hospital resuscitation an Automated External Defibrillator (AED) should be accessed if available as soon as possible. AED patch position
Correct patch position ensures that maximum defibrillation energy passes through the heart and improves the chances of successful defibrillation. Patches are most commonly placed in the sternal and apex positions, as shown below. Follow manufacturer guidelines for individual defibrillators. Figure 2 Correct sternal/apex patch position
Sternal patch- Middle of patch over
2nd intercostal space, midclavicular line
Apex patch- Middle of patch over
6th intercostal space, midaxillary line
(Wikimedia Commons, 2007)
Once CPR has commenced it should be continued without interruption, until:
the patient starts to breathe normally or shows signs of regaining consciousness, such as coughing, opening his eyes, speaking, or moving purposefully
the rescuer is exhausted and unable to continue the resuscitation attempt
Help arrives and takes over the resuscitation effort
a change in circumstances puts the rescuer at risk, e.g. fire
a doctor declares the patient dead.

NurseWest
Pa
ge8
Recommended Reading
Australian Resuscitation Council. (2010). Guideline 2 – Priorities in an Emergency. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_2/Priorities_in_an_Emergency.htm
Australian Resuscitation Council. (2010). Guideline 3 – Unconsciousness.
Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_3/Unconsiousness.htm
Australian Resuscitation Council. (2010). Guideline 7 – External Automated Defibrillation in Basic Life Support. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_7/External_Automated_Defibrillation_in_Basic_Life_Sup port.htm
Australian Resuscitation Council. (2010). Guideline 8 – Cardiopulmonary Resuscitation.
Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_8/Cardiopulmonary_Resuscitation.htm

NurseWest
Pa
ge9
Section three: Open Airway
The first step to successful airway management is to ensure that it is clear. It is important to look for and remove foreign material from the mouth before opening the airway. This is in order to avoid migration of any foreign material into the trachea, from where it would be difficult to remove and may impede delivery of breaths. In a hospital setting this may be performed by the use of suction. If the airway is found to be clear of foreign material it is important to ensure the tongue does not cause an obstruction. The collapsed patient experiences a loss of tone in the muscles of the throat and neck which may result in the tongue falling back into the oropharynx and obscuring the airway. The two most common methods for ensuring the tongue does not obstruct the airway are head-tilt and chin-lift (see Figure 4) and jaw- thrust (see Figure 5). Both are performed with the patient in the supine position.
OPENING OF THE AIRWAY TAKES PRECEDENCE OVER C-SPINE INJURIES

NurseWest
Pa
ge1
0
Figure 4 Head tilt and chin lift
(Jevon & Pooni, 2002, p. 44)
Both the tilt and the lift are designed to help displace the tongue forward from the oropharynx in order to open the airway. Jaw thrust can be used if a Cervical spine (C-spine) injury is suspected. The rescuer places their fingers beneath the patient’s ears on the corners of the lower mandible and gently moves the lower mandible forward. This allows the head, neck and thorax to remain in alignment and avoid exacerbating any C-spine injury. However if this technique is unsuccessful in opening the airway or in any way impedes the delivery of rescue breaths, then an alternative must be sought. This may mean having to risk exacerbating the C-spine injury by using the head-tilt and chin-lift. Failure to maintain head tilt and chin lift is the most common cause of airway obstruction during resuscitation.
Recommended Reading
Australian Resuscitation Council. (2010). Guideline 4 – Airway. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_4/Airway.htm
Figure 5 Jaw Thrust
(Resuscitation.110mb. n.d)

NurseWest
Pa
ge1
1
Section four: Normal Breathing?
Following clearance of the airway the next step is to determine if the patient is breathing normally. There is a high incidence of abnormal gasping (agonal breathing) following cardiac arrest; care should be taken NOT to confuse this for normal breathing. It is also important to ensure that any observed respiratory effort is as a result of chest inflation and not from abdominal movement which may occur in the patient with a lower respiratory obstruction. Abnormal breathing should be treated as if there is no breathing. Looking, listening and feeling for effort of breathing should assist in determining this.
Assessment of a patient’s circulation by use of a pulse check has been shown to be inaccurate and CPR should be commenced on unresponsive apnoeic patients.
Recommended Reading
Australian Resuscitation Council. (2010). Guideline 5 – Breathing.
Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_5/Breathing.htm
Look for movement of the lower chest or upper abdomen
Listen for the escape of air from nose and mouth
Feel for the movement of the lower chest or upper abdomen

NurseWest
Pa
ge1
2
Section five: Start CPR
Compressions
If the patient is unresponsive and not breathing normally external cardiac compressions should be commenced immediately. In order to ensure that chest compressions are performed at their most efficient the following three determinants should be properly addressed:
Position of hands
Depth of compression
Rate of compression
Position of hands
The rescuer’s hands need to be in the optimal position to ensure that the compressions are contributing as much as possible to the forward flow of blood. The correct position is the lower half of the sternum in the centre of the chest, as shown below (Figure 6).
Figure 6 the correct hand position for ECC
(First Aid Reference, 2010)
It is perfectly acceptable to simply place the hands in the centre of the chest over the lower half of the sternum. Positioning the hands too high on the chest will result in ineffective compression of the chest; positioning the hands too low may cause regurgitation and/or damage to internal organs.

NurseWest
Pa
ge1
3
Depth of compression
The chest should be compressed with the hands in the above position; the elbows locked and as much of the rescuer’s weight above the heels of their hands as is practicable. The sternum should be compressed approximately one third of the depth of the chest – more than 5 cm in adults. The rescuer should then relax the pressure without removing their hands from the patient’s chest, allowing the chest to recoil. The compression and relaxation phase should be of equal lengths of time. It is important that the depth of compression be consistently maintained with every compression for the duration of the resuscitation attempt.
Rate (speed) of compression
The recommended rate of compression is 100 per minute (approximately 2 per second). This does not imply that 100 compressions will be delivered in one minute since the number will be reduced by interruptions for breaths.
Fatigue
When feasible, rescuers should alternate responsibility for delivery of compressions every two minutes, regardless of whether they feel fatigued, to ensure consistently effective compressions are delivered. This change over should occur as quickly as possible to minimise interruptions to compressions and if possible only at breaks in the cycle, i.e. at the time of rhythm checks. Reduce fatigue and ensure adequate compression depth by adopting an ergonomic position for compressions with arms locked straight and using body weight to compress the chest directly downwards.
Figure 7 Position for effective ECC
(Emergency Response Training UK, 2008)
Position - Lower half of sternum in the middle of the chest
Depth - One third of the depth of the chest
Rate (Speed) - 100 compressions per minute

NurseWest
Pa
ge1
4
Rescue Breaths
In the hospital situation mouth to mask or bag and mask ventilation, as described in the Hospital Life Support (HLS) and HLS+ resources, are recommended.
Mouth to mask rescue breathing
It is advisable to use a pocket mask to deliver rescue breaths and hence avoid mouth to mouth contact if a bag and mask is not available.
Figure 8 Mouth to Mask ventilation technique
(U.S. Training Council, 2002)
As shown in Figure 6 the patient should be placed supine with the neck slightly flexed and the mask applied to the patient’s face using the thumbs of both hands. Lift the jaw into the mask using the fingers of both hands behind the angles of the jaw (jaw thrust), at the same time applying pressure with the thumbs to seal the mask on the face. Breaths are then delivered through the valve/opening at the top of the mask, watching for chest rise and fall. Oxygen can be applied via the port if the mask has this feature or otherwise by simply inserting tubing connected to the oxygen flow meter under the corner of the mask, with the flow rate at 10 L per minute. In order to ensure that each breath is being delivered correctly the chest should be observed for movement during administration. On observing that the chest has risen, the rescuer should then allow the breath to be released and observe the chest falling. This ensures that the rescuer does not over inflate the patient’s lungs. Each breath should take approximately one second.
If ventilation equipment is not available continue uninterrupted compressions at a rate of 100 compressions per minute

NurseWest
Pa
ge1
5
If at any stage during rescue breathing it is noticed that the abdomen is rising during inflation, the rescuer should stop, ensure there is no obstruction in the airway, and reposition the patient’s airway before carrying on. If at any time during resuscitation the patient should vomit, the rescuer should stop and clear the airway, turning the patient on their side only if necessary and, after returning to the supine position, re-establish an airway and recommence rescue breathing.
Mouth to mouth rescue breathing
In the absence of pocket mask or bag and mask, mouth to mouth technique may be used to deliver rescue breaths. This should not be necessary in hospital where equipment is readily available. The patient should be positioned supine and an open airway maintained by head tilt and chin lift or jaw thrust. The mouth should be opened and the rescuer’s lips used to form a seal around the patient’s lips; the nose can be sealed with the rescuer’s cheek or pinching with fingers. The rescuer should then exhale steadily into the lungs and observe the patient’s chest rise then fall. Each breath should take approximately one second.
Recommended Reading
Bohm, K., Rosenqvist, M., Herlitz J, Hollenburg. J., Svensson, l. (2007). Survival is similar after standard treatment and chest compressions only in out of hospital bystander cardiopulmonary resuscitation. Circulation, 116 (25), 2908-12.
In the event that you are unable or unwilling to perform rescue breaths, continuous chest compressions at a rate of 100 compressions per minute should be performed.

NurseWest
Pa
ge1
6
Section six: Special Circumstances
Certain circumstances require different interventions or slight alterations to the process of DRSABCD. These special circumstances include:
Pregnancy
Foreign body airway obstruction (choking)
Infants and children as discussed in Section Seven
Pregnancy
During the third trimester of pregnancy the enlarged uterus of a pregnant woman may interfere with blood flow. Whilst the mother is lying supine the uterus presses on the major abdominal veins and consequently venous return and cardiac output is impeded. This may result in the heavily pregnant woman dropping her blood pressure and becoming light- headed and eventually unconscious. If CPR is required in a heavily pregnant woman it should be performed with the patient lying
in the left lateral tilt position of up to 30o. To achieve this, place a wedge under the patient’s right hip. Alternatively if a second rescuer is available the uterus may be manually moved to the left side. The intention with either method is to shift the uterus off the major abdominal vessels.
Figure 9 Left lateral tilt using a firm wedge
(Vanden Hoek et al, 2010, p. S835)
Recommended Reading
Vanden Hoek, T. L., Morrison, L. J.; Shuster, M.; Donnino, M.; Sinz, E., Lavonas, Eric, J.; . . . Gabrielli, A. T. (2010) Part 12: cardiac arrest in special situations: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 122 (18),S829–S861. doi: 10.1161/CIRCULATIONAHA.110.9709
Figure 10 Left uterine displacement
(Vanden Hoek et al, 2010, p. S835)

NurseWest
Pa
ge1
7
Foreign body airway obstruction (Choking)
A foreign object can partially or completely obstruct the airway and is a life threatening emergency that can result in hypoxia and respiratory or cardiac arrest. The simplest way to assess the severity of obstruction is to assess for effective cough.
Effective cough (Mild airway obstruction)
In the event of a mild obstruction the patient should be kept as calm as possible and encouraged to continue coughing until the obstruction is relieved. If the obstruction persists, the patient deteriorates and/or displays an ineffective cough then assistance should be summoned (Code Blue Medical Emergency or ambulance as appropriate to situation) and attempts to relieve the obstruction should be made as outlined below.
Ineffective cough (Severe airway obstruction)
- Conscious (responsive) victim
1. Attempt up to five back blows with the heel of your hand between the shoulder blades. Check to see if the object has been cleared between blows. 2. If the obstruction is unrelieved - attempt up to five chest thrusts.
Identify the lower half of the middle of the sternum (see section on Compressions). The thrusts should be performed in the same manner as cardiac compressions but sharper and at a reduced rate.
3. If the obstruction remains unrelieved but the patient remains responsive continue to alternate between sets of up to five back blows and up to five chest thrusts. If the patient becomes unresponsive then full CPR should commence.
- Unconscious (unresponsive) victim
A finger sweep or suction may be used to relieve the obstruction; care should be taken not to further impact the obstruction. If the obstruction remains unrelieved and the patient is unresponsive then full CPR should commence.

NurseWest
Pa
ge1
8
Management of Foreign Body Airway Obstruction
Access Severity
Ineffective cough
Severe airway obstructions
Effective cough
Mild airway obstructions
Unconscious Conscious Encourage coughing
Continue to check casualty until recovery or
deterioration
Summon assistance
Summon Assistance
Commence CPR
Summon assistance
Give up to five back blows
If not effective
Give up to five chest thrusts
(Australian Resuscitation Council, 2010)

NurseWest
Pa
ge1
9
Section seven: Infants and Children
The same pathway of DRSABCD and the principles of assessment, external chest compressions and breathing remain relevant to children. However important anatomical differences exist between children and adults and these differences may alter the administration of the above techniques. For the purposes of paediatric resuscitation the following age descriptions can be applied:
Infant - under one year of age
Young child - a child between the ages of one and eight years
Older child – a child from nine to fourteen years of age.
Older children are generally treated as adults. However the rescuer must take into consideration the physical maturity of each individual.
Airway
Infants and young children have very soft oral structures, therefore care should be taken when removing objects from the oral cavity, particularly when using suction, to avoid damage and bleeding which maybe aspirated. Also note that the trachea in an infant is very narrow and pliable. This means that any bending of the trachea may actually result in an airway obstruction. It is recommended that the breathing assessment and breaths for an infant should be performed with the head in a neutral position and without any head tilt. As in the adult, the tongue of a child may cause an airway obstruction. In order to overcome this chin support with the head in a neutral position should be used (See Figure 11).
Figure 11 Infant with head in neutral position
(Safety Squad, 2011)

NurseWest
Pa
ge2
0
The first hand should be placed on the infant’s forehead to help maintain the neutral position. The index finger of the second hand should then be placed on the point of the infant’s chin with slight upward pressure to raise it. Care should be taken not to press the soft tissue below the point of the chin or raise the head. In this position the thumb can then be used to open the mouth.
As the child matures a small degree of head tilt may be employed. The older the child is, the greater the degree of head tilt that will be required.
Initial breaths
The ARC now recommends Basic Paediatric CPR (performed by laypersons) to commence with compressions at a ratio of 30:2, regardless of the number of rescuers, without prior breaths. However, for Advanced Paediatric CPR (performed by healthcare professionals) the ARC and Advanced Paediatric Life Support Australia/New Zealand recommend giving 2 initial breaths prior to commencing compressions.
If no equipment is available and mouth to mouth breaths are to be delivered the following technique is recommended:
While maintaining the open airway, as described above, the rescuer seals their mouth over the child’s mouth or mouth and nose for infant/small child. If the mouth alone is used the nose should be pinched close.
Each breath should be delivered as a slow exhalation; lung volume/size should always be considered when providing breaths to infants and children. They will not require the same volume delivery as an adult.
When delivering a breath the rescuer should observe carefully for chest movement and once this has been achieved - stop, and allow the child to exhale. Do not use the full capacity of your own lungs!
Head position of child during resuscitation
Infants – neutral with chin support
Young child – slight head tilt with chin support
Older child – full head tilt and chin lift as maturity allows

NurseWest
Pa
ge2
1
External Cardiac Compressions
The same three determinants of chest compression apply to children as for adults:
Position of compression
Depth of compression
Rate of compression
Position of compression
The position of compression is the same as in adult CPR, the lower half of the sternum in the centre of the chest.
Depth of compression
The depth of compression also remains the same - one third of the depth of the chest. The amount of weight applied to achieve this depth will have to be reduced because of the size difference from an adult to a child; too much weight can result in chest injuries. The amount of weight applied is reduced by adjusting the contact with the child’s chest.
Figure 12 Infant compressions – Two fingers
(Department of Health, n.d.)
Chest compressions in a child
Infants – use the tips of the middle and index fingers of one hand or two thumbs, with hands encircling the chest
Young child – use the heel of one hand
Older child – use two hands as degree of maturity allows
Figure 13 Infant compressions – Two thumbs
(Student BMJ, 1998)

NurseWest
Pa
ge2
2
Rate of compression
The rate of compression is also the same as in adult CPR, 100 compressions per minute.
Choking child
The techniques to deal with a choking child are the same as those used for an adult. Due to the smaller size of a child consideration may be given to performing the back blows with the young child or infant laying across the rescuer’s knee, face down, thereby allowing gravity to assist. The chest thrusts may be performed with the infant/small child across the rescuer’s lap in the supine position.
Figure 14 Back blows and chest thrusts for the choking infant
(Discovery Health, 2011)
Infant and Child Cardiopulmonary Resuscitation
For non-healthcare or a single person rescuers:
Compressions 30:2 Breaths
For multiple healthcare rescuers:
Compressions 15:2 Breaths

NurseWest
Pa
ge2
3
Recommended Reading
Australian Resuscitation Council. (2010). Guideline 4 – Airway. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_4/Airway.htm
Australian Resuscitation Council. (2010). Guideline 5 – Breathing. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_5/Breathing.htm
Australian Resuscitation Council. (2010). Guideline 6 Compressions.
Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_6/Compressions.htm
Australian Resuscitation Council. (2010). Guideline 8 – Cardiopulmonary
Resuscitation. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_8/Cardiopulmonary_Resuscitation.htm

NurseWest
Pa
ge2
4
Summary of CPR in Infants and Children
Infants
( under 1 year )
Young Child
(1-8 years )
Older Child
(9-14 years)
Airway
Neutral head position and chin support
Sniffing position and chin
support
Head tilt and chin lift as per
adults
Breathing
.
Healthcare
professionals
2 Rescue breaths in drowning incidents
Seal over mouth and nose
for mouth to mouth
Healthcare
professionals
2 Rescue breaths in drowning incidents
Seal over mouth only or
mouth and nose, dependent upon size of
child, for mouth to mouth
Healthcare
professionals
Seal over mouth only for
mouth to mouth
Compressions
1. Hand position
COMMENCE CPR IF Heart
rate less than 60bpm
Lower half of sternum 2
fingers/ 2 thumbs
COMMENCE CPR IF Heart
rate less than 40bpm
Lower half of sternum
heel of 1 hand
COMMENCE CPR IF Heart
rate less than 40bpm
Lower half of sternum
heel of both hands
2. Depth of
compression
One third of the depth of
the chest
One third of the depth of
the chest
One third of the depth of
the chest
3. CPR ratio
Single rescuer/lay people
Two healthcare professionals
30 compressions: 2 breaths
15 compressions:
2 breaths
30 compressions: 2 breaths
15 compressions:
2 breaths
30 compressions: 2 breaths
15 compressions:
2 breaths

NurseWest
Pa
ge2
5
Summary
In any emergency situation it is vitally important that the responders adopt a systematic approach to a rescue attempt. The DRSABCD system is the one endorsed by the Australian Resuscitation Council (ARC). The 2010 ARC guidelines highlight the importance of good quality and minimally interrupted CPR. If a person has collapsed and does not seem to be responding, commencing chest compressions is never inappropriate.
References
AllRefer Health [Image]. (2011). Retrieved from http://health.allrefer.com/pictures-images/recovery-position-series- 3.html
Australian Resuscitation Council [Image]. 2010. Retrieved from http://www.resus.org.au.fhlibresources.health.wa.gov.au/policy/guidel ines/section_4/Airway.htm Bohm, K., Rosenqvist, M., Herlitz J, Hollenburg. J., Svensson, l. (2007).
Survival is similar after standard treatment and chest compressions only in out of hospital bystander cardiopulmonary resuscitation. Circulation, 116 (25), 2908-12.
Department of Health [Image]. (n.d). Retrieved from http://www.health.wa.gov.au/education/tracheostomy/me_compressi ons.cfm
Discovery Health [Image]. (2011) Retrieved from http://healthguide.howstuffworks.com/choking-first-aid-infant-under-1- year-picture.htm
Emergency Response Training UK [Image]. (2008). Retrieved from http://blog.ertuk.co.uk/
First Aid Reference [Image]. (2010). Retrieved from http://www.firstaidreference.com/cpr-circulation-and-chest- compressions/108/
Jevon, P. & Pooni, J.S. (2002).Cardiopulmonary resuscitation: Tracheal intubation—1, preparation. Nursing Times, 98 (2), 43-44.
Morley, P., Jacobs, I., Walker, T., Nolan, J., Soar, J., Lockey, A., Pitcher, D. … Mitchell, S. (Eds). (2006). Advanced life support (5th ed.). London, UK: Resuscitation Council (UK)
Resuscitation.110mb.com [Image]. (2011). Retrieved from http://resuscitation.110mb.com/05_00_00.html
Safety Squad [Image]. 2011. Retrieved from http://blog.safetysquad.com/.a/6a00e54ef4b2b888330128757ad3459 70c-pi
Student BMJ [Image]. (1998). Retrieved from http://archive.student.bmj.com/back_issues/0898/data/0898ed4.htm
U.S. Training Council [Image]. (2002). Retrieved from http://ustc- ecc.com/Hand-OnlyCPR.htm
Vanden Hoek, T. L., Morrison, L. J.; Shuster, M.; Donnino, M.; Sinz, E., Lavonas, Eric, J.; . . . Gabrielli, A. T. (2010) Part 12: cardiac arrest in special situations: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 122 (18),S829–S861. doi: 10.1161/CIRCULATIONAHA.110.970954

NurseWest
Pa
ge2
6
Appendix 1: ARC and NZRC BLS Algorithm 2010