B33E11 Complete TB
-
Upload
jennifer-lopata -
Category
Documents
-
view
217 -
download
0
description
Transcript of B33E11 Complete TB
-
Cancer Biology and Chemotherapy
Tracey D Bradshaw
E-mail: [email protected]
Outline:
Introduction to cancer
Cytotoxic and Target-directed cancer chemotherapy
-
Appreciate the size of the cancer problem and the challenge facing
patients, clinicians and researchers
Incidence
Mortality
Objectives (i)
-
Appreciate the size of the cancer problem and the challenge facing
patients, clinicians and researchers
Incidence
Mortality
Recognise common cancer terminology
Apreciate some causes of cancer epidemiology
Objectives (i)
-
Appreciate the size of the cancer problem and the challenge facing
patients, clinicians and researchers
Incidence
Mortality
Recognise common cancer terminology
Apreciate some causes of cancer epidemiology
Cancer is a genetic disease
Oncogenes
Tumour suppressor genes
DNA repair genes/mechanisms gatekeepers
Objectives (i)
} drivers
-
Appreciate the size of the cancer problem and the challenge facing
patients, clinicians and researchers
Incidence
Mortality
Recognise common cancer terminology
Apreciate some causes of cancer epidemiology
Cancer is a genetic disease
Oncogenes
Tumour suppressor genes
DNA repair genes/mechanisms gatekeepers
An understanding of the processes of tumourigenesis and the
hallmarks of cancer
Objectives (i)
} drivers
-
CANCER; TUMOUR; NEOPLASM
Benign: normal chromosomes
differentiated
rare division/slow growing
encapsulated
do not metastasise
Malignant: abnormal chromosomes
poorly differentiated
may be frequent division
capable of invasion and
metastasis
All multicellular organisms can be afflicted by cancer:
Apparent rising incidence - expanding knowledge - earlier diagnosis
- increased lifespan
-
An estimated 12.7 million new cancer cases were diagnosed worldwide in 2008.
Lung, female breast, colorectal and stomach cancers were the most commonly diagnosed
cancers, accounting for >40% of all cases.
Worldwide, an estimated 7.6 million deaths from cancer occurred in 2008.
Lung, stomach, liver, colorectal and female breast cancers were the most common causes, accounting
for >50% of all cancer deaths.
Cancer: Global Statistics (2008)
-
Cancer: The U.K. Statistics
Cancer will affect one in three of the UK population, and be responsible for one in four deaths (>324K new cases in UK in 2010)
There are more than 200 different types of cancer, but four of them lung, breast, colorectal and prostate account for over half of new cases
65% of cases occur in those over 65
In children, leukaemia is the most common cancer
-
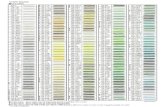
Cancer Incidence statistics 2005
-
Cancer Mortality statistics 2007
Female Male
-
5 year Cancer Survival 2001 (England and Wales)
Breast 79%
Prostate 61%
Lung 6%
CRC
-
21 Common Cancers: 2005 - 2009 and Followed up to 2010 Five-Year Relative Survival, Adults Aged 1599, England
Breast >80%
Prostate >80%
Lung
-
Cancer Classification
Carcinomas: the most common types of cancer, arise from cells of embryonic endoderm or ectoderm, cover external and internal body surfaces, e.g. epithelia of lung, breast, colon
Sarcomas: arise from cells of embryonic mesoderm, the supporting tissues of the body such as bone, cartilage, fat, connective tissue and muscle
Lymphomas: cancers that originate in the lymph nodes and tissues of the bodys immune system
Leukaemias: cancers of the immature wbcs that grow in the bone marrow and accumulate in large numbers in the bloodsteam
-
Cancer: General Considerations
Cancer is a disease of abnormal differentiation:
consider leukaemia, neuroblastoma
Cancer arises from loss of normal growth control
Cancer is a disease of genetic origin
A tumour arises from one ancestral genetically
aberrant cell
Tumourigenesis is a multi-stage process
-
Cancer: General Considerations
Cancer is a disease of abnormal differentiation:
consider leukaemia, neuroblastoma
Cancer arises from loss of normal growth control
Cancer is a disease of genetic origin
A tumour arises from one ancestral genetically
aberrant cell
Tumourigenesis is a multi-stage process
-
Apoptosis
Proliferation
Homeostasis perturbed
Homeostasis
Proliferation Apoptosis (Cell division) (Cell death)
cancer
-
Cancer: General Considerations
Cancer is a disease of abnormal differentiation:
consider leukaemia, neuroblastoma
Cancer arises from loss of normal growth control
Cancer is a disease of genetic origin
A tumour arises from one ancestral genetically
aberrant cell
Tumourigenesis is a multi-stage process
-
Cellular
metabolism
UV
light
Ionising
radiation Chemical
exposure Replication
errors
DNA damage: Single strand break
Double strand break
Chemical crosslink
DNA-protein crosslink
DNA-DNA crosslink
Base oxidation, alkylation
Abasic site
Pyrimidine dimer
>200 000 events / cell / day
Cell cycle
checkpoint
activation
Apoptosis
DNA Repair:
Direct repair
Base Excision Repair (BER)
Nucleotide Excision Repair (NER)
Mismatch Repair (MMR)
Homologous Recombination
Non Homologous End Joining
DNA Repair
Genetic origins of Cancer
-
Cancer: General Considerations
Cancer is a disease of abnormal differentiation:
consider leukaemia, neuroblastoma
Cancer arises from loss of normal growth control
Cancer is a disease of genetic origin
A tumour arises from one ancestral genetically
aberrant cell
Tumourigenesis is a multi-stage process
-
Tumourigenesis is a multistep process:
May take decades
Age-dependent cancer incidence e.g. prostate cancer
Initiation Single genetic event
Promotion Clonal expansion
Progression Increased genetic / chromosomal instability,
accumulation of mutations, increasingly aggressive
phenotype
Metastasis
*
* *
-
Causes of Cancer
Tobacco Body weight Physical activity Diet Hormones (reproductive factors - late age at first
pregnancy a factor in breast cancer)
Sunlight (UV radiation) Occupational carcinogens (asbestos, benzene,
pesticides)
Infectious agents - Viruses (papillomavirus (HPV) in cervical cancer)
- Bacteria (H. Pylori gastric ulcers/cancer
Medical treatment (radio- and chemotherapy)
Pollution (diesel exhaust, xenoestrogens) Heritable cancer predisposition syndromes
-
Smoking- and lung cancer incidence in the
20th Century
Cigarette smoke is a toxic
cocktail of > 4000 chemicals.
>43 known carcinogens are
inhaled.
-
Smoking- and lung cancer incidence in the
20th Century
Cigarette smoke is a toxic
cocktail of > 4000 chemicals.
>43 known carcinogens are
inhaled.
HO
OH
O
Benzopyrene[a]pyrene from cigarette
smoke condensate damages DNA of
lungs contributing to pathogenesis of lung
cancer
-
Smoking- damages many parts of the body
-
Causes of Cancer
Tobacco Body weight Physical activity Diet Hormones (reproductive factors - late age at first
pregnancy a factor in breast cancer)
Sunlight (UV radiation) Occupational carcinogens (asbestos, benzene,
pesticides)
Infectious agents - Viruses (papillomavirus (HPV) in cervical cancer)
- Bacteria (H. Pylori gastric ulcers/cancer
Medical treatment (radio- and chemotherapy)
Pollution (diesel exhaust, xenoestrogens) Heritable cancer predisposition syndromes
-
Infectious causes of cancer
Oncogenic human viruses:
Hepatitis C RNA virus
Causes hepatocellular carcinoma through
cycles of inflammation, repair and regeneration.
Oncogenic bacteria:
Heliobacter pylori, a spiral flagellated
Gram negative bacterium which underlies
pathogenesis of gastric carcinoma
causes gastritis, peptic ulceration and cancer.
Half the world`s population infected
Barry Marshall
http://discovermagazine.com/2010/mar/07-dr-drank-broth-gave-
ulcer-solved-medical-mystery
-
1. Self-sufficiency in growth signals
2. Insensitivity to growth-inhibitory signals
3. Evasion of programmed cell death
(apoptosis)
4. Limitless replicative potential
5. Sustained angiogenesis
6. Tissue invasion and metastasis
7. Reprogramming energy metabolism
8. Evasion of immune destruction
The Hallmarks of Cancer (Hanahan and Weinberg, Cell, 2011, 144, 646-674)
Cancer is complex but can be understood in terms of
underlying Principles of Tumourigenesis.
-
Apoptosis
Proliferation
Homeostasis perturbed
Homeostasis
Proliferation Apoptosis (Cell division) (Cell death)
cancer
-
Homeostasis
Proliferation Apoptosis
Proto-Oncogenes
Tumour suppressor genes
C-abl p53
Cancer cells acquire mutations in genes which encode
proteins whose roles in regulatory circuits control
normal cell proliferation and homeostasis
-
Homeostasis
perturbed
Proliferation
Carcinogenic Oncogenes
Apoptosis
Tumour suppressor genes
bcr-abl
p53
X
Cancer
-
Proto-oncogenes and Signalling Systems
Proto-oncogenes encode proteins that relay growth-stimulatory signals from outside the cell to the nucleus
Growth factors bind to specific receptors on the cell membrane
Receptor binding activates proliferative signal transduction cascades within the cytoplasm
The succession of relay proteins results in activation of transcription factors which drives transcription of genes producing proteins which usher the cell through its growth cycle
-
Oncogenes and Signalling Systems A Some oncogenes force cells to
overproduce growth factors e.g. sarcomas and gliomas release excessive platelet-derived growth factor
B Some oncogenes produce aberrant or elevated receptors which release proliferative signals even in the absence of growth factor, e.g. Erb-B2 (Her2) receptors in breast cancer cells
C Some oncogenes perturb signalling cascades in the cytoplasm, e.g. mutant Ras protein found in carcinomas of the colon, pancreas and lung
D Some oncogenes alter the activity of nuclear transcription factors, e.g. c-myc in the absence of growth factors in leukaemias, breast, stomach and lung cancers
Ras
Her2
Her2
cytoplasm
nucleus
c-myc
-
The Hallmarks of Cancer (1)
Self-Sufficiency in Growth Signals
Proto oncogenes Oncogenes
mutated
inappropriately expressed
constitutively activated
Cancer
-
q 34
q 11 bcr
c-abl proto-oncogene
145 kDA
Chr 9 22 9q+ Ph1
t (9;22)
Translocation mutation
bcr-abl 210 kDa
Carcinogenic oncogene
- tyrosine kinase activity
constitutively active
9q+ Ph1
Pathogenesis of Chronic Myeloid Leukaemia (CML)
-
Point Mutations:
If a point mutation occurs, - a single base is altered
- an altered codon
- different amino acid
- protein function
Point mutations in codons 12, 13 or 61 lead to constitutive activation of growth stimulatory signals and tumour formation:
Codon 61: CAA AAA; glutamine - lysine
Ras Most common carcinogenic oncogene in human
cancer (25%): 90% pancreas, 50% colon; 50% thyroid.
-
The Hallmarks of Cancer (2):
Insensitivity to growth-inhibitory signals
Cancer cells evade or ignore braking signals issued by normal cells
Tumour suppressor genes (P53, PTEN) are mutated, thereby inactivated
In a point mutation: - a single base is altered
- an altered codon
- different amino acid
- protein function
In P53 protein: G A; codon 273 results in Arginine - Histidine and inactivation of function.
-
The Hallmarks of Cancer (2):
Insensitivity to growth-inhibitory signals
P53 protein (the guardian of the genome) can halt cell cycle progression in response to DNA
damage, promoting DNA REPAIR or inducing
APOPTOSIS (programmed cell death)
Mutant p53 is found in over half of all human tumours
-
You have access to different types of cancer either
via the menu on the left or by clicking on a specific
cancer name on the map below.
-
Cell Cycle
G1 Production of RNA proteins
and enzymes needed for
DNA synthesis
S DNA synthesis
G2 preparation for mitosis,
specialised proteins are
synthsised
M prophase, metaphase,
anaphase, telophase
Division to form 2 daughter
cells.
P53
P53
p53
Division of cells with carcinogenic DNA lesions
X Cell cycle arrest DNA Repair MMR,
BER,
NER,
HR
-
The Hallmarks of Cancer (3):
Evasion of programmed cell death (apoptosis)
Tumour growth is determined not only by the rate of cell proliferation but also by the rate of cell attrition, Programmed Cell Death: APOPTOSIS
P53 protein helps to trigger cell suicide; its inactivation by many tumour cells reduces the likelihood of elimination of damaged cells
Cancer cells also synthesise excessive amounts of survival proteins (eg Bcl-2), which inhibit apoptosis
-
Cellular
metabolism
UV
light
Ionising
radiation Chemical
exposure Replication
errors
Genetic origins of Cancer
P53
Apoptosis
X
Cells with damaged DNA, harbouring
carcinogenic lesions survive and proliferate
-
Cellular
metabolism
UV
light
Ionising
radiation Chemical
exposure Replication
errors
Genetic origins of Cancer
X
Cells with damaged DNA, harbouring
carcinogenic lesions survive and proliferate
BCL-2
MCL-1
SURVIVAL
-
:
Proto-oncogenes
Tumour supressor genes
Genes encoding proteins involved in DNA repair:
Nucleotide Excision Repair (NER): XP
Homologous Recombination: BRCA1/2
DNA Damage leading to Genetic Mutations.
Tumour initiation
Cellular
metabolism
UV
light
Ionising
radiation Chemical
exposure Replication
errors
-
Li-Fraumeni syndrome: Heritable Cancer Predispositions conferred by germline
mutation in P53.
Germline mutation in P53
tumour suppressor gene 17p13
Predisposes sufferers to
wide variety of cancer types
Young age at onset of
malignancies
Multiple primary sites during
lifetime:
Breast, brain, leukaemia, soft
tissue / bone sarcoma.
BBC Radio 4 Inside the Ethics Committee Series 9 episode 3; 22. 08. 2013.
-
So far
Cancer is a genetic disease
Oncogenes
Tumour suppressor genes
Genes encoding DNA repair proteins
Hallmarks of cancer
Self sufficient growth
Overcome growth inhibitory signals
Evasion of apoptosis
-
Hallmarks of cancer
Self sufficient growth
Overcome growth inhibitory signals
Evasion of apoptosis
Limitless replicative potential
Sustained angiogenesis
Invasion
Metastasis
-
DNA segments at the ends of chromosomes,
known as telomeres (TTAGGG in humans)
protect chromosomal integrity, tally the
number of replicative generations and initiate
senescence and crisis.
The Hallmarks of Cancer (4):
Infinite replicative potential
Thus, the number of divisions a cell can
undergo is finite
The telomerase enzyme complex restores
telomeres to the ends of chromosomes,
enabling endless replication
Telomerase is active in >85% cancers but
inactive in most normal cells
-
The Hallmarks of Cancer (4):
Infinite replicative potential
-
The Hallmarks of Cancer (5):
Sustained angiogenesis
Proliferation of new capillaries is known as angiogenesis (or neovascularisation), it is typically short-lived (one or two weeks).
Tumour cells however can switch on angiogenesis. Angiogenesis is crucial for:
Primary tumour growth (promotion of a small cluster of mutated cells to a large malignant growth)
Metastasis.
-
Blood vessel
Oxygenated area
Hypoxic tumour mass
Necrotic region
Why is angiogenesis important for tumours?
-
In situ carcinoma: undetectable microscopic mass of tumour cells
Tumour cells secrete molecules (e.g. vascular endothelial growth
factor, VEGF)
Signalling activates genes/ protein synthesis in normal host tissue
encouraging growth of new blood
vessels to the tumour
-
In normal tissues, cells adhere to cells and to extracellular matrix (ECM): growth is anchorage dependent.
In cancer cells, cell adhesion molecules: E-cadherin are compromised or absent. Growth becomes anchorage independent.
Cancer cells release matrix metalloproteinase enzymes which dissolve basement membranes allowing invasion and escape.
Invasion of vascular beds of distant organs allows secondary tumours, metastases to establish.
The Hallmarks of Cancer (6):
Tissue Invasion and metastasis
-
Cancers are capable of spreading through the body by:
Invasion: Penetration of cancer cells into neighbouring tissues:
Mammary carcinoma invading the surrounding breast tissue
The Hallmarks of Cancer (6):
Tissue Invasion and metastasis
-
(6) Tissue Invasion and metastasis
Secondary tumours are more aggressive and resistant to therapy.
Metastases account for ~ 90% cancer deaths.
Metastasis: Systemic circulation and invasion of distant tissues:
lung,
liver,
bone.
-
Cancer is a genetic disease
Oncogenes
Tumour suppressor genes
Genes encoding DNA repair proteins
Hallmarks of cancer
Self sufficient growth
Overcome growth inhibitory signals
Evasion of apoptosis
Infinite replicative ability
Sustained angiogenesis
Invasion and metastasis
Cell 2011 Mar 4;144(5):646-74. D Hanahan and RA Weinberg Hallmarks of cancer: the next generation.
-
Current Treatment Options
Surgery (localised tumour)
Radiotherapy (localised tumour)
Chemotherapy (disseminated tumour)
-
Cancer Chemotherapy
Chemotherapy uses chemical agents, which may be:
natural products, natural product-derived (semi- synthetic), natural product-inspired,
synthetic small molecule or antibody anticancer drugs to destroy or control the growth of cancer cells.
Because chemotherapy treats the whole body, it can
treat cancer cells that have already escaped the
primary tumour.
-
Objectives
Understand the mechanisms of action of major clinically used cytotoxic anticancer drugs.
A knowledge of mechanisms of acquired / inherent resistance to chemotherapeutic agents, and
appreciate rationale underpinning combination
therapy.
Appreciate the side effects associated with chemotherapeutic agents and their cause.
-
Cell Cycle
G1 Production of nucleotide
bases, RNA proteins and
enzymes needed for DNA
synthesis
S DNA synthesis
G2 preparation for mitosis,
specialised proteins are
synthesised
M prophase, metaphase,
anaphase, telophase
Division to form 2 daughter
cells.
G0 Dormant phase
G0
-
Cytotoxic chemotherapy interferes primarily with DNA synthesis and mitosis (the (G1) S and M phases of the
cell cycle) to destroy cancer cells.
Chemotherapeutic drugs do not distinguish between normal cells and cancer cells. Adverse reactions to
chemotherapy are a consequence of cytotoxicity to normal cells.
However, cytotoxic chemotherapeutic agents do show selectivity for cancer cells over normal cells:
Normal cells are able to repair DNA; normal tissues
recover. Injury caused by chemotherapy is rarely
permanent.
-
Mustard Gas was first used in September 1917 during WWI. It was one of the most
lethal of all the poisonous chemicals used in warfare.
British soldiers blinded by mustard gas
Cytotoxic Chemotherapy: History
-
During WWII, it was found that soldiers who were
exposed to mustard gas, sulfur mustard suffered
from lower white blood cell counts.
This discovery led to the use of nitrogen mustard, a
similar but less toxic chemical agent, to cure patients
with high white blood cells counts (lymphoid
leukaemia) and lymphomas.
Cytotoxic Chemotherapy: History
S
CH2--CH2--Cl
CH2--CH2--Cl
-
During WWII, it was found that soldiers who were
exposed to mustard gas, sulfur mustard suffered
from lower white blood cell counts.
This discovery led to the use of nitrogen mustard, a
similar but less toxic chemical agent, to cure patients
with high white blood cells counts (lymphoid
leukaemia) and lymphomas.
Cytotoxic Chemotherapy: History
S
CH2--CH2--Cl
CH2--CH2--Cl
N
CH2--CH2--Cl
CH2--CH2--Cl
H3C
In 1942, Nitrogen Mustard chlormethine, became the first antineoplastic chemotherapeutic agent used medicinally.
This agent forms a covalent bond with DNA,
Alkylating specific sites on purine (A, G) bases of DNA
Crosslinking DNA
Causing cell death
This ALKYLATING AGENT is the pioneer of Antineoplastic Chemotherapy
-
4 (nucleo)bases: A G C T
Base + deoxyribose sugar = nucleoside
Base + deoxyribose sugar + phosphate =
nucleotide
Nucleotide polymers = nucleic acid (DNA)
Deoxyribonucleic acid (DNA)
-
Nuceotide polymers:
DNA double helix
-
CH3
N7 methyl guanine
Nuceotide polymers:
DNA double helix Pyrimidines
Purines
-
Alkylating agents
The oldest class of anticancer drugs
Major cornerstone of treatment for leukaemias, lymphomas and solid
tumours.
Other nitrogen mustard analogues:
Chlorambucil
Melphalan,
Ifosfamide
Cyclophosphamide:
One of most widely used cytotoxic agents in combination or sequentially with other antineoplastic drugs. Used to treat cancers of:
Brain, breast, bladder, cervix, endometrium, lung, testis, ovary, Burkitt`s, and other
non-Hodgkin`s lymphoma, multiple myeloma, gestational trophoblastic tumours,
childhood malignancies neuroblastoma, retinoblastoma, Wilms`, Ewing`s, leukaemias: CLL, ALL, CML, AML.
NCH2--CH2--Cl
CH2--CH2--ClHO2C(H2C)3
NH
P
O
NCH2--CH2--Cl
CH2--CH2--Cl
O
-
Cyclophospahmide - Mechanism of action:
Cyclophosphamide is a prodrug requiring biotransformation by
cytochrome P450 (CYP 3A4 in the liver) to exert toxicity.
NH
P
O
NCH2--CH2--Cl
CH2--CH2--Cl
ONH
P
O
NCH2--CH2--Cl
CH2--CH2--Cl
O
HO
CYP 3A4
4-OH-CPA
NCH2--CH2--Cl
CH2--CH2--ClP
O
H2N
O-
H
O
+
Phosphoramide mustard + acrolein
active alkylating species unwanted by-product
Cross-links RNA and DNA haemorrhagic cystitis
-
Alkylating agents 2: Nitrosourea derivatives
The anticancer activity of this class of compounds was discovered in 1959 at the NCI
Activity against solid and non-solid tumours
Lipophilic allowing access across BBB
Chloroethylate DNA
Therapeutic efficacy limited by development of resistance, involving multiple repair pathways
ClNNO
NH
Cl
O
-
Alkylating agents 2: Nitrosourea derivatives
The anticancer activity of this class of compounds was discovered in 1959 at the NCI
Activity against solid and non-solid tumours
Lipophilic allowing access across BBB
Chloroethylate DNA
Therapeutic efficacy limited by development of resistance, involving multiple repair pathways
ClNNO
NH
Cl
OCarmustine
Used alone or adjuvant treatment of
brain, colon, lung cancers, Hodgkin`s,
non-Hodgkin`s lymphoma, melanoma,
multiple myeloma, mycosis fungoides.
-
Alkylating agents 2: Nitrosourea derivatives
The anticancer activity of this class of compounds was discovered in 1959 at the NCI
Activity against solid and non-solid tumours
Lipophilic allowing access across BBB
Chloroethylate DNA
Therapeutic efficacy limited by development of resistance, involving multiple repair pathways
Carmustine
Used alone or adjuvant treatment of
brain, colon, lung cancers, Hodgkin`s,
non-Hodgkin`s lymphoma, melanoma,
multiple myeloma, mycosis fungoides.
Antineoplastic and toxic effects caused by active metabolites. Chloroethyl carbonium
ion leads to formation of DNA cross links during all phases of cell cycle, causing cell
cycle arrest and apoptosis.
-
N N
NN
N
CH3
H2NOC
O
Alkylating agent
Treatment of high grade Glioma recurrent anaplastic astrocytoma
and gliobastoma multiforme
Malignant melanoma and brain
metastases from solid tumours
Alkylating agents 3: Triazenes
NH
NN
N
H2NOC
N
CH3
CH3
Alkylating agent
Treatment of metastatic
malignant melanoma (response
rate 15-25%)
Hodgkin`s lymphoma (in combination with doxorubicin,
bleomycin and vinblastine)
Dacarbazine Temozolomide
-
Malignant Melanoma
-
Ed Newlands
-
11C (Me)-Temozolomide in positron emission tomography (PET) after oral administration
Saleem et al, Cancer Res., 2003, 63, 2409-2415
-
11C methylation of DNA
N N
N
N
O
N
H2NOC
Me14C 11C
11C
15N
Isotopic labelling of temozolomide
Expired 11CO2
Expired N2
NH
N
H2NOC
14C
NH2
Excretion
Protonation
-
N N
NN
N
CH3
H2NOC
O
Major Mechanism of Resistance inherent or acquired:
Repair of methylated DNA O6methyl guanine by methyl guanine methyl transferase MGMT.
Tumours whose cells express MGMT are resistant to
Temozolomide
-
Alkylating Agents
Transfer an alkyl group onto DNA
CH3 methyl
CH3CH2Cl chloroethyl
DNA damage :
in S phase (block DNA synthesis), G2
arrest
DNA single strand breaks- double
strand breaks.
Cross link the 2 strands.
-
Antimetabolites
Bastion of Cancer Chemotherapy
Chemicals structurally similar to either FOLATE or NUCLEOBASES
DNA building blocks
FOLIC ACID growth factor, provides
carbon atoms for nucleotide precursors
in synthesis of RNA and DNA
FOLATE ANTAGONISTS inhibit one
(or more) folate-dependent enzymes
-
Purine antagonists inhibit
production of A and G in DNA and
RNA
Guanine
Adenine
Cytosine
Thymine
Uracil
Pyrimidine antagonists block
synthesis of C and T in DNA; C
and U in RNA
Thus, the antimetabolites
BLOCK DNA SYNTHESIS
-
Methotrexate
Most commonly used folate antagonist.
Enters cell via folate receptors
Binds DHFR
Inhibits synthesis of FH4
Cell cannot create new purine and thymidine nucleotides
DNA and RNA synthesis blocked
-
Methotrexate
Administered alone or in combination with other chemotherapeutic agents to treat:
leukaemia, lymphoma
gestational choriocarcinoma
solid tumours: breast, head and neck, lung, bladder,
oesophagus
Methotrexate can be given by many routes: po, iv, sc, im, intra-arterial, intrathecal.
It is the only cytotoxic drug for which there is a role for routine PK monitoring:
leucovorin / folinic acid rescue bypasses inhibited DHFR,
replenishing intracellular reduced folate pools.
Other clinical folate antagonists: Permetrexed, Ralitrexed, Nolatrexed
-
Pyrimidine Analogues
5-FLUOROURACIL and CAPECITABINE decrease the biosynthesis of
pyrimidine nucleotides by inhibiting thymidylate synthase, the enzyme
that catalyses the rate limiting step in DNA synthesis.
CAPECITABINE is converted to 5-FLUOROURACIL in cancer cells
5-FU cannot be methylated by thymidylate synthase, causing sustained
inhibition of the enzyme and decreased production of Thymine.
5-FU is incorporated into DNA (via dUMP or dTMP) or RNA (via UTP),
leading to cytotoxicity via DNA strand breakage and decrease in protein
synthesis
5-FU
-
Pyrimidine Analogues
5-FLUOROURACIL and CAPECITABINE decrease the biosynthesis of
pyrimidine nucleotides by inhibiting thymidylate synthase, the enzyme
that catalyses the rate limiting step in DNA synthesis.
Clinical Applications:
In a number of iv combination chemotherapies for treatment of bowel,
breast, gastric, oesophageal, pancreatic, head and neck, anal and
ovarian cancers.
Oral analogues are also used, and topical application for superficial basal
cell carcinoma.
5-FU
Additional pyrimidine antagonists: Gemcitabine, Tegafur, Sapacitabine
-
Purine Antagonists
In clinical use since 1953
Mercaptopurine
Adenine analogue
Treatment of ALL, AML, Hodgkin`s lymphoma in children,
lymphoblastic lymphoma.
Dose-related toxicity bone marrow suppresssion
Thioguanine
Synthetic guanine analogue inhibition of purine synthesis
-
Antimetabolites
Inhibit production of DNA building blocks
Antifolates
Purine antagonists
Pyrimidine antagonists
Act in G1 cell cycle phase
(Prevent DNA synthesis)
-
Antimicrotubule agents
The Company of Biologists Ltd 2005
Paralyse tubulin (which forms
microtubules) or microtubules
Critical for cell division
Block cell cycle during Mitosis
Microtubules allow segregation of chromosomes during mitosis
-
Antimicrotubule agents 1
Paclitaxel (Taxol) Isolated from Pacific Yew:
Taxus brevifolia
Problem: limited supply and extraction
Semi-synthetic Docetaxel (Taxotere) from the more abundant taxane precursor
found in needles of European Yew:
Taxus baccata
Taxanes
Microtubule poisons
- stabilise microtubules
- inhibit depolymerisation
cause G2/M cell cycle arrest
Treatment of Breast, Ovarian, Lung carcinomas
-
Antimicrotubule agents 2
Vinca Alkaloids
Isolated from Madagascan
periwinkle Catharanthas roseus.
> 70 alkaloids identified in sap
from C roseus used historically in
folk (traditional) medicine.
Vincristine (Oncovin) Vinblastine (Velbe)
Used in treatment of leukaemia, lymphoma,
melanoma, soft tissue sarcoma,
neuroblastoma, breast and lung cancers.
Mechanism of action:
Bind -tubulin
Inhibit tubulin polymerisation
Destabilise (depolymerise)
microtubules:
Destruction of mitotic spindle, leaving
cells stranded in mitosis.
-
Antimicrotubule agents
The Company of Biologists Ltd 2005
Tubulin Microtubules Polymerisation
depolymerisation
Vinca alkaloids
Taxanes
Preventing cells from completing mitosis
-
control
taxol
vincristine
Antimicrotubule agents
Prevent successful mitoses
-
Cytotoxic chemotherapy So far.
Alkylating agents Nitrogen mustard
Cyclophosphamide
Temozolomide
-
Cytotoxic chemotherapy So far.
Alkylating agents Nitrogen mustard
Cyclophosphamide
Temozolomide
Antimetabolites Methotrexate folate antagonist 5-Fluorouracil pyrimidine antagonist Thioguanine purine antagonist
-
Cytotoxic chemotherapy So far.
Alkylating agents Nitrogen mustard
Cyclophosphamide
Temozolomide
Antimetabolites Methotrexate folate antagonist 5-Fluorouracil pyrimidine antagonist Thioguanine purine antagonist
Spindle poisons Taxanes stabilise microtubules Vinca alkaloids inhibit tubulin polymerisation
Anticancer Therapeutics: Ed Sotiris Missailidis, Wiley-Blackwell, 2008.
-
Platinum drugs
Pt
H3N
Cl
Cl
H3N
Cisplatin
Discovery 1965
Clinical application 1970s
Intravenous short term infusion in saline
Treatment of solid/epithelial malignancies:
First line and in combination: testicular, ovarian, cervix uterus, lung, head and neck, oesphagus, stomach, colon,
bladder.
Second line: advanced breast, pancreas, liver, kidney, prostate,
peritoneal and pleural mesotheliomas.
-
Cisplatin: Mechanism of Action:
Cisplatin crosslinks DNA causing interstrand and intrastrand GG,
AG Pt adducts.
Replication inhibition,
Transcription inhibition,
Cell cycle arrest,
DNA repair mechanisms
triggered - failure,
Cell Death
-
Carboplatin
Adverse Cisplatin reactions
Renal, GastroIntestinal Toxicity, Peripheral Neuropathy.
Markedly less toxic to kidneys and nervous system causing less nausea and vomiting.
-
Platinum agents
Cross link DNA
Damage triggers cell cycle arrest and DNA repair mechanisms
Which fail (initially)
Activating apoptosis
S cell cycle phase
-
Antitumour Antibiotics
Substances produced by micro-organisms (or plants, or
marine invertebrates) that exert anticancer activity by
DNA interaction.
Multiple modes of action, may be subject to alternative
classification - alkylating agents
- DNA cleavage agents
- non covalent binding agents
- topoisomerase inhibitors
Actinomycin D
Mitomycin C
Bleomycin
Doxorubicin - anthracycline
Etoposide - podophyllotoxin
Irinotecan - camptothecin
-
Bleomycin
Linear glycosylated peptide antibiotic
Isolated from Streptomyces verticellus in 1960s
There are > 200 members of bleomycin family,
blenoxane = bleomycin A2 + bleomycin B2
Treatment of: Hodgkin`s, non-Hodgkin`s lymphomas, squamous
cell carcinoma, testicular carcinoma, malignant
pleural effusions, Kaposi`s sarcoma.
Mechanism of Action:
DNA damage generation of DNA Double Strand Breaks (DSBs) and single strand breaks (SSBs).
RNA cleavage caused by bleomycin-induced oxidative damage.
Nucleic acid cleavage dependent on presence of Fe2+ and molecular
oxygen.
-
Bleomycin
Linear glycosylated peptide antibiotic
Isolated from Streptomyces verticellus in 1960s
There are > 200 members of bleomycin family,
blenoxane = bleomycin A2 + bleomycin B2
Treatment of: Hodgkin`s, non-Hodgkin`s lymphomas, squamous
cell carcinoma, testicular carcinoma, malignant
pleural effusions, Kaposi`s sarcoma.
Serious Adverse Reaction:
Cumulative pulmonary toxicity Lung fibrosis
Mortality in 1-2% bleomycin treated patients.
Manageable adverse reactions:
nausea, vomiting, appetite loss, alopoecia, allergic reactions, skin damage
-
Doxorubicin
Anthracycline antibiotic tetracyclic chromophore with
anthraquinone motif.
Antibacterial,
Immunosuppressive,
Antiparasitic and wide spectrum
Antitumour activity.
First isolated in 1960s from
cultures of Streptomyces peucetius.
Large scale prep developed in 1970s involve semisynthetic
process starting from daunoubicin
Doxorubicin and Daunorubicin, used clinically for four
decades, are amongst most efficient antitumour drugs.
-
Doxorubicin
Frequent Indications include:
Breast, ovarian, transitional cell bladder cancer, bronchogenic
lung cancer, thyroid and gastric cancer, soft tissue and
osteogenic sarcomas, neuroblastoma, Wilms` tumour,
malignant lymphoma (Hodgkin`s and non Hodgkin`s, acute
myeoloblastic leukaemia, acute lymphoblastic leukaemia and
Kaposi`s sarcoma
Clinical Limitations:
Development of Acquired Resistance
Cardiotoxicity. Dilative cardiomyopathy and congestive heart
failure are cumulative adverse effects that appear (usually) after 1 year.
To prevent these severe reactions, a maximum cumulative dose of 600
mg/m2 has been established.
Less severe side effects include nausea, vomiting, diarrhoea, loss of
appetite, hair loss and skin damage.
-
Mechanism of Action of Doxorubicin
Doxorubicin is a Topoisomerase II poison/inhibitor
DNA exists in cells as a supercoiled double helix which must unwind during
transcription and replication.
Topoisomerse enzymes catalyse changes in DNA topology.
Doxorubicin inhibits Topoisomerase II-catalysed DNA relaxation
Doxorubicin binds strongly to duplex DNA by intercalation selectively at C-G sequences.
generation of DNA DSBs inhibiton of religation of cleaved duplex
Halted DNA synthesis
Cell Death
Doxorubicin leads to generation of Reactive Oxygen Species (ROS) which damage DNA
Formation of DNA adducts and crosslinks
Inhibition of DNA and RNA synthesis
-
Podophyllotoxin isolated from Podophyllum
peltatum Mayapple 1880
Potent antitumour activity with severe side effects
no clinical use
Podophyllotoxin - Etoposide
Research led to
synthesis of
Podophyllotoxin
analogues Etposide,
Teniposide
-
Mechanism of Action
Podophyllotoxin: Binds tubulin and inhibits mitotic spindle assembly
Etoposide and Teniposide poison the Topoisomerase II-DNA complex.
(forming a ternary complex) and prevent re-ligation of DNA
DNA Double Strand Breaks
Cell Death
Etoposide Clinical Applications
Main indications are for testicular and lung cancers
Non Hodgkin`s, Hodgkin`s lymphoma, AML, ALL, CML, mycosis
fungoides, Wilms`, neuroblastoma, Kaposi`s, gestational trophoblastic
tumours, ovarian germ cell tumours,brain and refractory breast cancer.
Dose related and limiting myelosuppression. Bone marrow recovery
usually complete (3 weeks).
-
Camptothecin
Pentacyclic antitumour antibiotic isolated
1966 from alkaloid extracts of Camptotheca acuminata.
Remarkable activity against murine
leukaemia models (NCI)
Mechanism of Action
Camptothecin binds and stabilises DNA-Topisomerase I complex,
inhibiting religation of cleaved DNA strands, blocking DNA
synthesis.
In the 1990s, water soluble camptothecin analogues were
synthesised, demonstrating Topo I inhibition and potent antitumour
activity: Topotecan and Irinotecan have reached the clinic.
-
Irinotecan
Approved in Japan in 1994
lung,
cervical
ovarian cancers
Subsequently in Europe and US for
treatment of Colorectal cancers.
Side effects: diarrhoea, neutropaenia
Novel camptothecin analogues under clinical evaluation including
liposome-encapsulated camptothecins.
-
So far
DNA alkylators Platinum agents
Antimetabolites Antitumour antibiotics
Tubulin inhibitors Topisomerase inhibitors
-
Cytotoxic Chemotherapy targets rapidly dividing cells
DNA alkylators Platinum agents
Antimetabolites Antitumour antibiotics
Tubulin inhibitors Topisomerase inhibitors
-
Cytotoxic Chemotherapy targets rapidly dividing cells
Dose limiting toxicity: GI, haematological, renal, cutaneous toxicities:
Cells which divide rapidly under normal circumstances vulnerable
Bone marrow - myelosuppression
Digestive tract - mucositis
Hair follicles - alopecia
Lack of clinical efficacy
Drug resistance
inherent, acquired
.
Cytotoxic Chemotherapy: Limitations
-
Clinical mechanisms of resistance
Decreased drug uptake
down regulation of Cu transporting pump decreased intracellular Cisplatin concentrations and reduced Cisplatin toxicity
Enhanced drug efflux
In 1976, the MultiDrug Resistance protein-1 (MDR-1; P-
glycoprotein (P-gp); ABCB1) was
described.
P-gp pumps out of the cell a large number of broadly active
cytotoxic chemotherapeutic agents.
Cells overexpressing Pgp possess a
multidrug resistant phenotype.
-
Enhanced drug efflux
ATP binding casette (ABC) protein pumps commonly overexpressed in resistant
tumours, capable of transporting anticancer agents with distinct mechanisms
of action.
ABCB1 (P-gp); MRP-1 (multiple drug resistance protein-1; ABCC1); BCRP
(breast cancer resistance protein, ABCG2); MRP-5.
-
Clinical mechanism of resistance
Decreased drug uptake
Enhanced drug efflux (P-gp)
Altered target expression
upregulated transcription and overexpression of DHFR in response to Methorexate treatment
DNA repair MGMT removes and repairs alkylated DNA bases (Temozolomide)
Failure to activate (pro)drug (cytochrome P-450)
Metabolic drug inactivation
Mutations / altered activity of drug target
(decreased topoisomerase II-etoposide binding affinity;
Tubulin mutations)
-
Combination Chemotherapy
Treatment with a number of agents / regimes
simultaneously / sequentially with DISTINCT
mechanisms of action:
To eradicate tumour cells - heterogenous disease
Prevent emergence of acquired resistance
Limit toxicities / spare normal cells
-
Acute Lymphoblastic Leukaemia
80% childhood leukaemia
85% successful treatment
Combination treatment comprises:
Intrathecal MTX - antifolate antimetabolite
Vincristine vinca alkaloid
Daunorubicin antitumour antibiotic
Steroids enhance chemotherapy efficacy, wellbeing, combat tiredness,
anti-sickness, improve apetite, balance body salts, water
L-Asparaginase - an enzyme that destroys asparagine external to the
cell. Normal cells are able to make all the asparagine they need
internally whereas tumour cells become depleted rapidly and die.
Radiotherapy
-
Combination Therapy Breast Cancer
Surgery, Radiotherapy, Chemotherapy.
Cyclophosphamide alkylating agent
Epirubicin, Doxorubicin antibiotic, DNA intercalator
5FU antipyrimidine
Methotrexate antifolate
Mitoxantrone topoisomerase II inhibitor
Taxol antimicrotubule
Gemcitabine antipyrimidine
Tamoxifen (Hormone therapy; Herceptin, targeted, biological therapy.
-
Understand the mechanisms of action of major clinically used cytotoxic anticancer drugs.
Appreciate the side effects associated with chemotherapeutic agents and their cause.
A knowledge of mechanisms of acquired/inherent resistance to chemotherapeutic agents
Appreciate rationale underpinning combination therapy.
Summary Slide
-
Objectives: Target-directed therapy
Be aware of general treatment strategies.
Understand the mechanisms of action of major clinically used anticancer drugs.
Rationale behind target-directed therapy.
Knowledge of example molecularly targeted therapies and mechanisms of action.
A knowledge of mechanisms of acquired resistance to targeted agents, and appreciate rationale underpinning combination therapy.
Appreciate the side effects associated with chemotherapeutic
agents and their cause.
-
Cytotoxic Chemotherapy
Targets rapidly dividing cells (DNA)
DNA alkylators (S; cyclophosphamide; temozolomide)
Antimetabolites (G1; 5-FU, methotrexate)
Topisomerase inhibitors (etoposide)
Antitumour antibiotics (S; bleomycin, doxorubicin)
Tubulin inhibitors (G2/M; vincristine, taxol)
Limitations
Dose limiting side effects:
GI, haematological, renal, cutaneous toxicities
Drug resistance
Lack of clinical efficacy
-
Aim
To develop targeted agents that are tumour specific with decreased
toxicity profiles than chemotherapeutic agents.
Target-directed drug discovery
Advances in cancer cell and molecular biology have led to identification
of carcinogenic oncogenes and elucidation of cancer signalling networks
Patient / tumour
selection
development of
target-directed agents
-
Key Signalling Cascades in tumourigenesis
-
Workman, P. and Kaye, S.B. (2002) Translating basic cancer research into new
cancer therapeutics. Trends. Mol. Med. 8(4), S1-S9.
Workman, P. (2005) Genomics and the second golden era of cancer drug development. Molecular
Biosystems 1(1), 17-26.
Target-directed drug discovery
identification of a validated biological target (normally a protein)
a molecule hunt, typically involving a high-throughput screening
hit-to-lead development to identify (a) lead compound(s)
lead development (involving in vivo testing and optimisation of ADMET properties)
[Absorption, Distribution, Metabolism, Excretion, Toxicity].
clinical trials with appropriate pharmacodynamic (PD) endpoints
-
Tyrosine kinases (TKs) encoded by proto-oncogenes - are
important mediators of signalling cascades:
Key roles in growth, differentiation, metabolism and apoptosis
TK activity is tightly regulated in normal cells
Role of TKs in pathophysiology of cancer:
Mutation(s), overexpression of TKs (carcinogenic oncogenes)
lead to malignant growth.
Block constitutive activation of TKs in cancer cells:
Selective Small Molecule and
Monoclonal Antibody Inhibitors:
Tyrosine Kinases - Roles and significance in Cancer.
-
HER2
} EGFR
bcr/abl
Small molecule RTK Antibody
Gleevec bcr/abl
Vemurafenib BRAF
HER2 Herceptin
Iressa EGFR Erbitux
Tarceva
Sunitinib VEGFR Avastin
Tyrosine Kinase inhibitors examples
Targeted treatment for:
CML Melanoma Breast Prostate NSCLC CRC
-
q 34
q 11 bcr
c-abl proto-oncogene
145 kDA
Chr 9 22 9q+ Ph1
t (9;22)
Pathogenesis of Chronic Myelogenous Leukaemia
bcr-abl 210 kDa
tyrosine kinase activity
constitutively active
9q+ Ph1
-
The Gleevec Story:
Bcr-Abl a Good Target
A distinct chromosomal translocation the Philadelphia chromosome
Bcr-Abl gene formed by juxtaposition of c-Abl oncogene on chromosome 9 with the Bcr oncogene on chromosome 22
Resulting oncoprotein with elevated tyrosine kinase activity seen in 95% of patients with chronic myelogenous leukaemia (CML)
A distinct drug target clearly differing in activity between normal and leukaemic cells
-
Gleevec: Chemical Optimisation
Initial compound identified in high-throughput screen
Promising lead-like properties high potential for chemical diversity
Lead eventually to Gleevec (SAR studies aided by molecular modelling)
Gleevec binds in ATP pocket, induces apoptosis in CML cells and causes dose-dependent inhibition of tumour growth in xenograft mouse models
N
N N
H
N
Protein kinase Cinhibitor
N
N N
H
N
Me
N
H
O
N
N
STI571 (Gleevec)
(Glivec; Imatinib)
-
Gleevec: Mechanism of Action
Initial compound identified in high-throughput screen
Promising lead-like properties high potential for chemical diversity
Lead eventually to Gleevec (SAR studies aided by molecular modelling)
Gleevec binds in ATP pocket, induces apoptosis in CML cells and causes dose-dependent inhibition of tumour growth in xenograft mouse models
-
The Gleevec Story: Clinical Activity
Outstanding clinical activity in CML patients, particularly in chronic phase of disease (95% response in Phase II human trials)
Much lower response (29%) and high relapse rate in later stages of disease (blast crisis)
Other tyrosine kinase receptor targets of Gleevec include c-kit in GastroIntestinal Stromal Tumours (GIST), and Platelet Derived
Growth Factor (PDGF) receptor (variety of tumours)
Drug resistance in late stage disease mutations in ATP binding pocket
Novel agents - active in Gleevec-resistant disease:
( Nilotinib, Dasatinib. Weisberg et al, Nature Reviews cancer 7 p345 2007)
-
Point mutation: B-RAF
- a single base is altered
at position 1799 thymine is replaced by adenine
- an altered codon
- different amino acid
Valine (V) is replaced by glutamate (E) at codon 600
protein function
Constitutive activation
V600E mutation
drives pathogenesis
of > 60% Metastatic
Melanoma
-
VEMURAFENIB
V600E mutated BRAF inhibition
August 2011: FDA approves Zelboraf (vemurafenib) and companion
diagnostic test for BRAF mutation-positive metastatic
melanoma, a deadly form of skin cancer.
-
VEMURAFENIB
V600E mutated BRAF inhibition
Mechanisms of resistance to vemurafenib
Cancer cells may overexpress a cell surface protein PDGFRB creating an alternate survival pathway.
NRAS mutation, reactivating the normal BRAF survival pathway
-
Vemurafenib vs Dacarbazine in metastatic melanoma patients
Chapman et al NEJM 2011
-
75% invasive breast cancers are classified ER+;
65% are ER+ and PR+
Treatment strategies for ER+ breast cancer:
Inhibition of oestrogen synthesis
Oestrogen receptor blockade
Growth of ER+ breast tumours is stimulated by oestrogen.
Breast Cancer UK statistics:
In 2008 12,000 women and 70 men died from breast cancer
-
Targeting Oestrogen synthesis in ER+ Breast Cancer
Aromatase inhibitors
X X
-
Oestrogen receptor blockade
Tamoxifen, Raloxifene
-
Anastrazole
(Arimidex)
Tamoxifen
Treatment strategies for ER+ breast cancer:
Inhibition of oestrogen synthesis Oestrogen receptor blockade
-
In 25-30% metastatic breast cancer patients the human
epidermal growth factor receptor 2 - HER2 protein is
overexpressed through amplification of the HER2 gene.
HER2 signaling, particularly
activation of downstream effector
pathways including the
Ras/Raf/MAPK and PI3K/Akt
pathways, has been implicated in
the pathogenesis of breast
cancer.
HER2+ overexpression is
associated with a poorer
prognosis than HER2- tumours.
These cancers are less
responsive to conventional
chemotherapy and hormonal
therapy.
-
Herceptin a humanised monoclonal antibody
specifically blocks HER2 on the surface of breast
cancer cells and turns off the permanently on signal for cell division.
GFR
Ras PI3K
Raf AKT
Mek mTOR
Proliferation
apoptosis resistance
invasion, angiogenesis
protein translation
PTEN
-
Herceptin increases the survival
time of women with advanced
breast cancer.
-
Androgen-dependent prostate cancer:
Inhibition of androgen synthesis:
Critical role of CYP 17 in androgen synthesis
Inhibition of CYP17 hydroxylase and lyase activities by Abiraterone
-
Treatment for Androgen-dependent prostate cancer:
Abiraterone
Inhibition of prostate cancer cell proliferation
-
Targeted therapy for the treatment of Non Small
Cell Lung Cancer
Background
NSCLC most common form of lung cancer leading cause of cancer mortality Too advanced to be operable in ~50% patients First-line platinum agents give only modest increase in
survival
Limited efficacy and side effects of cytotoxic chemotherapy need for new therapies
Aim
To achieve cancer specific effects by targeting aberrant molecular pathways underlying tumour
growth to improve efficacy and minimise side effects
-
Activation of EGFR is involved in NSCLC growth and progression:
Inhibition of apoptosis Proliferation Angiogenesis Metastasis
Lancet Oncology 2006; 7:499
-
Aberrant signalling important in development and
progression of NSCLC
EGFR expressed in up to 93% and overexpressed in ~45% of NSCLCs Level of EGFR expression correlates with poor prognosis and reduced
survival
good target
-
Lancet Oncology 2006; 7:499
Targeting EGFR
Monoclonal antibodies directed against extracellular ligand binding domain e.g. cetuximab (Erbitux) prevent ligand binding
Small molecule selective inhibitors of intracellular TK domain e.g. gefitinib (Iressa; erlotinib (Tarceva) block autophosphorylation
Downstream
Signal
Transduction
Inhibited
-
EGFR Inhibitors: IressaTM and TarcevaTM
Gefitinib Erlotinib
N
N
N
F
Cl
O
MeO
N
OH
ZD1839 (Iressa)
N
N
N
O
O
H
OSI-774 (Tarceva)
O
O
Synthetic small molecule receptor tyrosine kinase inhibitor
Compete with ATP binding to intracellular TK domain of EGFR
Inhibit receptor autophosphorylation
Block downstream signal transduction
Orally available
-
Tarceva: place in therapy
Approved November 2004 for 2nd line tx of advanced NSCLC
Antitumour activity and symptom relief (improved quality of life) in
patients where standard chemotx
has failed; mild adverse effects
(skin rash, diarrhoea)
Erlotinib Placebo
End Points n = 488 n = 243 P value
Progression-free survival (months)
2.2 1.8 < 0.001
Overall survival (months)
6.7 4.7 < 0.001
1-year survival (%) 31 22
-
NSCLC responders vs. non-responders to EGFRi
Somatic mutations in the TK domain of EGFR correlates with subset of
patients who are exquisitely sensitive:
Women; never smokers; east Asian descent; adenocarcinoma;
bronchoalveolar carcinoma.
Tarceva
-
Efficacy of Gefitinib vs C/P in East Asian Patients
with NSCLC
Objective Response Rate (ORR) Gefitinib C/P P-value
Intent-to-treat population
(n = 609; 608) 43.0% 32.2%
-
Personalised Medicine Reduces Ineffective
Treatment in Colon Cancer
-
KRAS mutation testing in metastatic colorectal cancer
World J Gastroenterol. 2012 October 7; 18(37): 51715180.
Published online 2012 October 7. doi: 10.3748/wjg.v18.i37.5171
PMCID: PMC3468848
kras Testing
Do Not Treat
Treat with Erbitux
Treat with Erbitux
Treatment
Success
-
In situ carcinoma: undetectable microscopic mass of tumour cells
Tumour cells secrete molecules
(e.g. vascular endothelial growth
factor, VEGF)
Signalling activates genes/ protein
synthesis in normal host tissue
encouraging growth of new blood
vessels to the tumour
Judah Folkman 1933-2008 Founder anti-angiogenic therapy
One of the Hallmarks of Cancer: sustained Angiogenesis
promotes: Growth of primary tumour Metastasis
-
Hypoxia, transforming (oncogenic,
tumour suppressor) mutation:
HER2,ras, P53, PTEN, PI3K/AKT, NO, bFGF, Il-8, EGF, IGF-1, PDGF, COX-2, H2O2
VEGF
synthesis/release
P
P
P
P
Binding of VEGF to
VEGFR
VEGFR activation
Survival, proliferation,
migration
ANGIOGENESIS
Role of VEGF in Angiogenesis / Tumourigenesis
Potent mitogen for vascular
endothelial cells
Mediates the secretion and activation of enzymes which
degrade the extracellular matrix
e.g. matrix metalloproteinases,
collagenase
Survival factor for endothelial cells through inhibition of
apoptosis
Modulates endothelial cell migration
to sites of angiogenesis
Vascular maintenance
Lymphangiogenesis
VEGF
-
VEGF a good target ?
Key promoter of metastasis and central role in tumour growth
VEGF expression is increased in the majority of cancers examined to date
Overexpression correlates with risk of recurrence and poor prognosis
Drugs targeting VEGF activity at endothelial cells do not need to penetrate tumours
Drug resistance less likely than with traditional chemotherapeutics: greater genetic stability of endothelial cell compared to cancer cell
-
Targeting VEGF(R)
VEGF/VEGFR blockade by
monoclonal antibodies
Inhibition of receptor
signalling by small molecule
tyrosine kinase inhibitors
VEGF
Kinase
inhibitors Anti-VEGFR-1/2
VEGF receptor
Aptamer
Anti-VEGF
SiRNA
decoy receptor
Ribozyme targeting
VEGFR mRNA
-
How to target VEGF
BEVACIZUMAB Avastin;
Humanised neutralising IgG
monoclonal antibody directed
against VEGF
Binds all VEGF isoforms with
high affinity and blocks their
binding to the receptors.
VEGF
Kinase
inhibitors Anti-VEGFR-1/2
VEGF receptor
Aptamer
Anti-VEGF
SiRNA
decoy receptor
Ribozyme targeting
VEGFR mRNA
-
Place in therapy of Bevacizumab (Avastin)
Metastatic colorectal cancer (mCRC)
The addition of bevacizumab to 5-FU and irinotecan regime
increased survival time by ~ 5
months (30%) (20.3 months
versus 15.6 months; p < 0.001)
Approved (2004) in combination with first-line 5-FU-based
chemotherapy regimens
Bevacizumab plus chemotherapy improved survival in metastatic non-small cell
lung cancer in a randomized clinical trial*
-
Atkins et al. Nature Reviews Drug Discovery 5, 279280 (April 2006) | doi:10.1038/nrd2012
Small molecule inhibitor of VEGFR: Sunitinib
-
Results of Phase III trial of Sunitinib in glivec refractory GIST patients.
(G Demetri 2006).
Time to tumour progression
-
Sunitinib (Sutent) small molecule inhibitor of
VEGFR
Orally available small-molecule inhibitor of VEGFR 1, 2 and 3, PDGFR , , c-kit and flt-3 rich and diverse pharmacology
Phase II trials completed in cytokine-refractory metastatic renal cell cancer
Unusually high rate of objective tumour responses detected - 40%;
stable disease - 27%
Acquired resistance: rapid enhanced migratory and invasive capacity
-
Targeted therapies for solid tumours?
Gleevec success in CML where a single genetic alteration underpins disease pathogenesis (bcr-abl)
Common solid tumours do not have one defined genetic alteration driving the neoplastic process
Clinically heterogeneous disease
Acquired resistance: Target mutation (bcr-abl),
Elevated target expression (BRAF V600E)
Activation / upregulation of alternative signalling pathways (EGFR MET),
Acquired oncogenic mutations in complementary signal networks (EGFR Ras)
Enhanced cancer cell migration / invasion capacity
-
Mutation/loss of
FAP gene
APC
DNA
methylation
KRas
mutation
Loss of
P53
Acquisition of
multiple genetic
mutations
Solid Tumourigenesis
-
Targeting Solid Tumours
Combination of
molecularly-targeted agents with cytotoxic /
radiotherapy
Erbitux (cetuximab)
targets EGFR with
Irinotecan advanced colorectal cancer
Herceptin (Trastuzumab) targets HER2 protein with
paclitaxel HER2+ metastatic breast cancer
Avastin targets VEGF with paclitaxel or
carboplatin in NSCLC
Dual / multiple TK inhibitors
Zactima Sunitinib Sorafenib
Lapatinib: EGFR / HER2 GSK
small molecule Herceptin refractory breast, lung cancer
Capecitabine 5FU prodrug
-
The Phase III registration trial: Combination
with chemotherapy
Use of chemotherapy plus a monoclonal antibody against HER2 for
metastatic breast cancer that overexpresses HER2
Few studies of metastatic breast cancer demonstrated a
survival advantage of this magnitude.
Slamon DJ et al. N Engl J Med 2001; 344:783-792.
Prior anthracyclines
Herceptin + paclitaxel (n=92)
Paclitaxel (n=96)
-
Significant improvement in progression-free
survival (primary endpoint)
-
Summaryso far
The Molecular Mechanisms underpinning tumourigenesis are
Numerous,
Complex,
Not fully understood
Target aberrant proteins
Small molecules
Antibodies
Resistance
Combine cytotoxic and molecular targeted agents
to defeat cancer
-
Combination Therapy: Lung Cancer
-
Combination Therapy: Lung Cancer
Small cell lung cancer - chemotherapy (responds well; also radiotherapy)
Non small cell lung cancer (NSCLC)
- surgery, radiotherapy,
Biological therapy: EGFR inhibitors
Chemotherapy:
Cisplatin / carboplatin -
Etoposide -
Doxorubicin -
Topotecan -
Vincristine -
Gemcitabine -
-
Combination Therapy: Lung Cancer
Small cell lung cancer - chemotherapy (responds well; also radiotherapy)
Non small cell lung cancer (NSCLC)
- surgery, radiotherapy,
Biological therapy: EGFR inhibitors - Tarceva, Iressa
Chemotherapy:
Cisplatin / carboplatin - cross links DNA
Etoposide - Topo II inhibitor
Doxorubicin - DNA intercalator (heart complications)
Topotecan - Topo I inhibitor (camptothecin derivative)
Vincristine - antimicrotubule agent
Gemcitabine - antipyrimidine
-
Combination Therapy:
Colorectal (Bowel) Cancer
-
Combination Therapy:
Colorectal (Bowel) Cancer
Surgery (8/10)
Radiotherapy
Chemotherapy
5-fluorouracil (5-FU) -
Oxaliplatin -
Irinotecan -
Biological therapy
Erbitux; Iressa -
-
Combination Therapy:
Colorectal (Bowel) Cancer
Surgery (8/10)
Radiotherapy
Chemotherapy
5-fluorouracil (5-FU) - antipyrimidine
Oxaliplatin - platinum DNA crosslinker
Irinotecan - topoisomerase 1 inhibitor
Biological therapy
Erbitux, Iressa - EGFR inhibitors