Atrial Fibrilation... Tutorial
description
Transcript of Atrial Fibrilation... Tutorial

ATRIAL FIBRILATION
DEVIKHA PEREMEL

ATRIAL FIBRILATION
• Atrial fibrillation(AF) is a disorder of the rhythm of the heart. It results from disorganised electrical activity in the atria of the heart, which causes rapid stimulation of the ventricles, leading to an irregular pulse rate.

EPIDERMIOLOGY• Atrial fibrillation is the most common arrhythmia &
the incidence & prevalence increases with the age• The incidence:– <0.5% below 50Yrs– 2% in age 60-69– 4.6% in age 70-79– 8.8% in age 80-89
• Men were 1.5 times more likely to develop AF than women• Whites were more likely to develop AF than blacks







• If left untreated, AF can lead to various short- and long-term problems. In patients who have pre-existing heart failure, the rapid heart rate seen in AF can lead to low blood pressure, lung congestion, angina, or worsening of the heart failure.
• Untreated AF also increases the risk of stroke. This is because in AF the atria become dilated and contract ineffectively, which leads to blood clots developing in the atria. These clots can subsequently dislodge and travel to the brain and other organs, causing strokes and other organ damage.
The main risk factors for developing a stroke in patients with AF are:• Prior stroke or transient ischaemic attack• The finding of left ventricular dysfunction on echocardiogram• Age > 65• High blood pressure• Rheumatic heart disease• Diabetes mellitus• Congestive heart failure

HOW TO DIAGNOSE AF?• History & physical examination:
- Symptoms: severity, duration, constant or paroxysmal- Predisposing factors: alcohol, emotional or exercise- Disease association: CVS, DM, HTN, hyperthyroidism- Evaluate heart sound (murmur), thyroid or evidence of heart failure or AF complications (stroke).
• Electrocardiogram (ECG)• Echocardiogram - to evaluate the size of the right & left atria
and ventricles, and to asses peak right ventricle pressure• Transesophageal Echocardiography – more sensitive for
identifying thombus in the left atrium or left atrial appendage.

MANAGEMENT OF AF


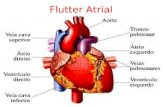
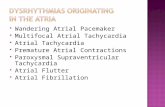
ATRIAL FLUTTER

DEFINITION
• Atrial flutter (AFL) is an abnormal heart rhythm that occurs in the atria of the heart. When it first occurs, it is usually associated with tachycardia (beats over 100 per minute)
and falls into the category of supra-ventricular tachycardias. • While this rhythm occurs most often in individuals with
cardiovascular disease (e.g. hypertension, coronary artery disease, and cardiomyopathy) and diabetes, it may occur spontaneously in people with otherwise normal hearts.
• It is typically not a stable rhythm, and frequently degenerates into atrial fibrillation(AF).
• However, it does rarely persist for months to years.

CLINICAL FEATURES
• Atrial flutter can sometimes go unnoticed.
SYMPTOMS:• Sensations of regular palpitations. Such sensations usually
last until the episode resolves, or until the heart rate is controlled.
• shortness of breath, • chest pains, • light-headedness or dizziness, • nausea and, in some patients, and• nervousness

• Prolonged fast flutter may lead to decompensation with loss of normal heart function (heart failure). This may manifest as effort intolerance (exertional breathlessness), nocturnal breathlessness, or swelling of the legs or abdomen.
SIGNS:• Pulse may be irregular or regular, but is usually rapid. • RAISED in the jugular venous pulse.• May be associated with signs of underlying causes - eg,
thyrotoxicosis, alcoholism, pericarditis, valvular dysfunction or septal heart defects.
• Heart failure, hypotension and respiratory distress may be present.

DIFFERENTIAL DIAGNOSIS
• Supraventricular tachyarrhythmias.• Atrial fibrillation.• Wolff-Parkinson-White syndrome.

INVESTIGATIONS
Electrocardiogram:• The absence of P waves, the P waves are replaced by “F” waves
of flutter, between which are no isoelectric intervals.• F waves have a frequency of 250-350 beats / minute, are
monomorphic, regular and have the appearance of “saw tooth”.• QRS complex has a normal aspect, it may have a longer duration
than usual, if there is a branch block or a ventricular preexcitation syndrome.
• In the absence of atrioventricular accessory pathways, driving trough ventricles is the most common, with block 2 / 1 ( can be met atrioventricular block 3 / 1 or 4 / 1).
• QRS complexes occur at irregular intervals, and F waves are well evidenced in the ECG.




MANAGEMENT
General treatment goals for symptomatic atrial flutter are similar to those for atrial fibrillation and include the following:• Control of the ventricular rate• Restoration of sinus rhythm• Prevention of recurrent episodes or reduction
of their frequency or duration• Prevention of thromboembolic complications• Minimization of adverse effects from therapy

• Cardioversion (DC) is currently recommended in forms of atrial flutter with hemodynamic deterioration or in combination with Wolf-Parkinson-White syndrome. After sedation, is applied an external electric shock, synchronous with low energy (20-50 joules), which can be repeated if necessary. Anticoagulant therapy should be considered in case of atrial flutter with a length greater than 48 hours.
• Decrease of ventricular rate with atrioventricular blockers: verapamil, diltiazem, digoxin, esmolol. Sometimes digoxin can converse a atrial flutter into a atrial fibrillation.
• Cardiac Ablation - High frequency (>500,000 Hz) energy flows easily up the ablation catheter because it has a very low resistance. When this energy flow encounters human tissue, the higher impedance produces resistive heat which pushes the cellular temperature above 50 degrees celsius and kills the cells. The dead tissue no longer propagates electrical signals, and the irregular rhythm patterns are disrupted. RF ablation is an effective treatment for supraventricular tachycardia (SVT) and atrioventricular nodal reentry tachycardia (AVNRT).



THANK YOU!!