Association of COVID-19 infection with pregnancy outcomes ......The ultrasound results and fetal...
Transcript of Association of COVID-19 infection with pregnancy outcomes ......The ultrasound results and fetal...

Journal Pre-proof
Association of COVID-19 infection with pregnancy outcomes in healthcare workersand general women
Suliman Khan, Li Jun, Nawsherwan, Rabeea Siddique, Yanyan Li, Guang Han,Mengzhou Xue, Ghulam Nabi, Jianbo Liu
PII: S1198-743X(20)30180-4
DOI: https://doi.org/10.1016/j.cmi.2020.03.034
Reference: CMI 1996
To appear in: Clinical Microbiology and Infection
Received Date: 25 February 2020
Revised Date: 18 March 2020
Accepted Date: 27 March 2020
Please cite this article as: Khan S, Jun L, Nawsherwan Siddique R, Li Y, Han G, Xue M, Nabi G, Liu J,Association of COVID-19 infection with pregnancy outcomes in healthcare workers and general women,Clinical Microbiology and Infection, https://doi.org/10.1016/j.cmi.2020.03.034.
This is a PDF file of an article that has undergone enhancements after acceptance, such as the additionof a cover page and metadata, and formatting for readability, but it is not yet the definitive version ofrecord. This version will undergo additional copyediting, typesetting and review before it is publishedin its final form, but we are providing this version to give early visibility of the article. Please note that,during the production process, errors may be discovered which could affect the content, and all legaldisclaimers that apply to the journal pertain.
© 2020 European Society of Clinical Microbiology and Infectious Diseases. Published by Elsevier Ltd. Allrights reserved.

1
Association of COVID-19 infection with pregnancy outcomes in healthcare workers and 1
general women 2
Suliman Khan1, Li Jun2, Nawsherwan3, Rabeea Siddique1, Yanyan Li4, Guang Han5, Mengzhou 3
Xue1, Ghulam Nabi6, Jianbo Liu7 4
1Department of Cerebrovascular Diseases, The Second Affiliated Hospital of Zhengzhou 5
University, Zhengzhou, China. 6
2Department of Obstetrics, Renmin hospital of Wuhan University, Wuhan, China. 7
3Department of Nutrition and Food Hygiene, School of Health Sciences, Wuhan University, 8
Wuhan 430071, Hubei, China. 9
4Department of Radiology, Wuhan health maternal and infant hospital. Wuhan 430000, Hubei 10
Province, China. 11
5Department of Radiation Oncology, Hubei Cancer Hospital, Tongji Medical College, Huazhong 12
University of Science and Technology, Wuhan, China. 13
6Key Laboratory of Animal Physiology, Biochemistry and Molecular Biology of Hebei Province, 14
College of Life Sciences, Hebei Normal University, Shijiazhuang 050024, China. 15
7Department of respiratory diseases, The Second Affiliated Hospital of Zhengzhou University, 16
Zhengzhou, China. 17
Correspondence: S.K ([email protected]), G.H ([email protected]), M.X 18
([email protected]) G.N ([email protected]), and J.L ([email protected]) 19
Contributed equally: S.K, L.J, N. and R.S 20
21
22
23
24
To the editor 25

2
Viral pneumonia is thought to be the most common non-obstetric infectious disease 1
during pregnancy, which is associated with maternal and neonatal morbidity and mortality 2
during pregnancy [1]. Atypical pneumonia known as coronavirus disease (COVID-19) caused by 3
severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is highly infectious and is 4
currently spreading rapidly around the globe [2]. Before leading to the global emergency, SARS-5
CoV-2 emerged in Wuhan, Hubei Province, China during December 2019 [3,4]. Several studies 6
focusing on infected patients from the general population have been reported, however, limited 7
information is available in the aspects of pregnancy outcomes of COVID-19 infected women. 8
Until now, Chen et al [5] reported the maternal-neonatal outcomes and vertical transmission 9
potential of COVID-19 pneumonia in pregnant women in the third trimester of pregnancy with 10
an infection history of a maximum of 7 days. However, more studies are needed in the aspects of 11
maternal and neonatal outcomes of pregnant women. This case series study was conducted to 12
assess the impact of COVID-19 infection on adverse pregnancy outcomes. In this study, the 13
duration from onset of infection to the delivery was 1-26 days. Both healthcare workers and 14
general infected women were included in the study. 15
We conducted a case series study on pregnant women (n =17) infected with COVID-19 16
admitted to Hubei general hospital (Renmin Hospital) from Jan 25 to Feb 15, 2020. COVID-19 17
pneumonia was diagnosed according to the New Coronavirus Pneumonia Prevention and Control 18
Program of 5th and 6th editions. All the seventeen pregnant women were found positive for 19
COVID-19 using either quantitative RT-PCR (qRT-PCR) and/or CT scan imaging or both. To 20
assess the neonatal infection with COVID-19, cord blood and neonatal throat swab samples were 21
collected immediately after delivery in the operating room and were tested by using quantitative 22
RT-PCR. All the patients delivered babies by C-section, and the detailed information collected 23
are presented in tables 1-4. We conducted a comprehensive literature search for the current 24
outbreak of COVID-19 infection in pregnant women and a thorough search for the impact of 25
SARS-CoV pregnancy outcomes. 26
The age range of the patients was 24–34 years and the range of gestational weeks at 27
admission was 35 weeks to 41 weeks. Moreover, the range of gestational weeks at delivery was 28
35 weeks and 5 days to 41weeks. respectively. In twelve individuals, the nucleic acid test from 29
the throat swab was positive for COVID-19 while only in five individuals both the CT scan and 30

3
nucleic acid test indicated COVID-19. We observed fever in three individuals and complications 1
in five. Other common symptoms were cough (n = 6), diarrhea (n = 3), nasal congestion (n = 2), 2
shortness of breath (n = 2), and sputum production (n = 1). Patients were receiving antibiotics 3
(n=17), hormones (n =8), and antivirals together with Chinese medicine (n= 15). A total of 17 4
neonates including three preterm neonates with birthweight ranging from 2300 g to 3750 g and 5
birth length from 45 cm to 52 cm (49.2 cm) were delivered through C-section. There was no fetal 6
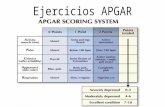
or neonatal death. The ultrasound results and fetal heart rate were normal for all the neonates 7
while the Apgar score for 16 neonates was in the range of 9-10. Only two neonates (case 6 and 8
case 14) after birth were suspected for COVID-19 while five neonates were reported with 9
neonatal pneumonia. Moreover, three cases were found with preterm delivery (Table 1 and Table 10
2). 11
Based on our findings in these seventeen patients, we suggest that COVID-19 infection 12
may lead to the occurrence of neonatal pneumonia and preterm delivery. However, we cannot 13
rule out the possibility that these complications can be linked to other biological processes or 14
intrauterine infections [6,7]. We collected all the samples in operation theatre with care to avoid 15
the chance of contamination. Thus, according to our knowledge, the collected samples were not 16
contaminated. The focus of this study was to investigate the vertical transmission potential of 17
COVID-19 infection. Two of the neonates (Table 2) were found suspected for COVID-19 18
infection, indicating the possibility for vertical transmission of COVID-19 infection. However, 19
we could not find convincing evidence to confirm the vertical transmission potential of COVID-20
19 infection. 21
Out of the seventeen neonates, we observed neonatal pneumonia in five neonates. 22
Similarly, in fifteen neonates, COVID-19 was not detected in the throat swab. The swab samples 23
tested within 24 hours after the delivery, were positive in only two neonates (case 6 and case 14). 24
However, intrauterine tissue samples such as placenta, cord blood or amniotic fluid were not 25
tested to confirm if the COVID-19 infection in the neonate was the result of intrauterine 26
transmission. Of note Chen et al. (2020) [5] for COVID-19 (n=9) and Wong et al. (2004) [8] for 27
the severe acute respiratory syndrome (SARS) (n=12) have not reported intrauterine vertical 28
transmission. 29

4
In summary, we found two neonates suspected for COVID-19 infection and five neonates 1
with neonatal pneumonia, suggesting the possibility that adverse pregnancy outcomes may be 2
linked to COVID-19 infection. 3
Acknowledgment: The authors acknowledge the Postdoctoral grant from The Second Affiliated 4
Hospital of Zhengzhou University (for S.K), and operating grant support from the National 5
Natural Science Foundation of China (grants no: 81870942, 81471174 and 81520108011), 6
National Key Research and Development Program of China (grant no: 2018YFC1312200), and 7
Innovation Scientists and Technicians Troop Constructions Projects of Henan Province of China 8
(for M.X). 9
Ethical statement: The work described has been carried out in accordance with The Code of 10
Ethics of the World Medical Association and informed consent was obtained from the patients 11
and parents of the babies. 12
Conflict of interest: The authors declare that there is no conflict of interest. 13
14
References 15
[1] Schwartz DA, Graham AL. Potential Maternal and Infant Outcomes from (Wuhan) 16
Coronavirus 2019-nCoV Infecting Pregnant Women: Lessons from SARS, MERS, and 17
Other Human Coronavirus Infections. Viruses 2020;12:1–16. doi:10.3390/v12020194. 18
[2] Khan S, Siddique R, Ali A, Xue M, Nabi G. Novel coronavirus, poor quarantine, and the 19
risk of pandemic. J Hosp Infect 2020. doi:10.1016/j.jhin.2020.02.002. 20
[3] Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 21
Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, 22
China. JAMA 2020. doi:10.1001/jama.2020.1585. 23
[4] Khan S, Nabi G, Han G, Siddique R, Lian S, Shi H, et al. Novel coronavirus: how the 24
things are in Wuhan. Clin Microbiol Infect 2020. doi:10.1016/j.cmi.2020.02.005. 25
[5] Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and 26
intrauterine vertical transmission potential of COVID-19 infection in nine pregnant 27

5
women: a retrospective review of medical records. Lancet 2020;6736:1–7. 1
doi:10.1016/S0140-6736(20)30360-3. 2
[6] Atay GA, Arsan S, Atasay B, Ensari A, Aysev D. The possible role of intrauterine 3
infections in unexplained second trimester abortions and macerated stillbirths: A study 4
from a single center. J Perinatol 2004;24:679–85. doi:10.1038/sj.jp.7211167. 5
[7] Kacerovsky M, Pliskova L, Bolehovska R, Gerychova R, Janku P, Matlak P, et al. 6
Lactobacilli-dominated cervical microbiota in women with preterm prelabor rupture of 7
membranes. Pediatr Res 2019:1–9. doi:10.1038/s41390-019-0692-1. 8
[8] Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and 9
perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet 10
Gynecol 2004;191:292–7. doi:10.1016/j.ajog.2003.11.019. 11

6
Table 1: Clinical details of pregnant women infected with COVID-19
Parameter Average (% and/or range) Comments Pregnant women occupation Health workers 3/17 (17.6%) Nurses and nephrologists were included in this study Non-health workers 14/17 (82.4) Pregnant women who were not related to medical profession General information Age (Years) 29.29 (24-34) Date of hospital admission Jan 25 to Feb 15 All the women were admitted from 25th January to 15th February.
Gestational age on admission (weeks+days) 37.82 (35-41) Majority of the women had gestational age 38-40 weeks Gestational age on delivery (weeks+days) 38.1 (35+5-41) Majority of the women had gestational age 38-40 weeks Number of days from onset of pneumonia until birth
4.2 (1-26) Only two women had 10 or more days of fetuses’ exposure to COVID-19 infection
Source of COVID-19 infection Contact with family infected member 2/17 (12%) Only two individuals were infected with COVID-19 before admission
Contact with infected patient 15/17 (88%) Majority of individuals including healthcare workers contracted infection inside the hospital
Mode of delivery and complications C-section 17/17 (100%) All the women had C-section, however, some of the women had
premature rupture of fetal membrane thus, underwent emergency C-section
Complications 5/17 (29%) Only five pregnant women had complications that caused preterm delivery
Signs and symptoms Maximum body temperature 38.5 °C
The minimum body temperature was 36.2 °C, where the majority of patient had a body temperature approximately 37 °C. Majority of the patients did not develop fever until the delivery, while sputum, shortness of breath and nasal congestion were rare. Comparatively, more
Fever 3/17 (18%) Cough 6/17 (35%) Diarrhea 3/17 (18%) Shortness of breath 2/17 (12%)

7
Nasal congestion 2/17 (12%) individuals had cough.
Sputum 1/17 (6%) Infected with COVID-19 17/17 (100%) Treatment/ Therapy Antiviral 16/17 (94%) Antiviral drugs oseltamivir or arbidol or both were given orally, while
Ribavirin was given intravenously according to the severity of symptoms. Antibiotics 17/17 (100%) Cefoperazone sulbactam sodium, Ceftazidime, Azithromycin, and
Moxifloxacin hydrochloride were given to the patients who needed it. Hormones 8/17 (47%) Chinese medicine 15/17 (88%) All those receiving Chinese medicine received Lianhua Qingwen.
Laboratory characteristics
Confirmatory (quantitative RT-PCR) test 12/17 (70.5%) Overall 12 women were confirmed only with qPCR testing for nucleic acid form pharynx swab samples.
Confirmatory (quantitative RT-PCR) test + Chest CT scan
5/17 (29.5%) 5 out of 17 patients were confirmed both with qPCR testing for nucleic acid from pharynx swab samples and chest CT scanning
Low or normal leukocyte count (<9·5 × 10⁹ cells per L)
9/17 (52.9% and5.03-19.97) The increased leukocyte count was observed in 8 patients. This increase may or may not be linked to COVID-19 infection.
Lymphocyte count (× 10⁹ cells per L) 4/17 (23.5% and 0.63-2.37) 4 out of 17 patients were found with lymphopenia, which could be linked with COVID-19 infection
Elevated ALT (>45 U/L) 2/17 (11.7% and 9-46) Two out of 17 patients were found with elevated AST and/or ALT. however, the majority of the patients had normal ALT and AST levels. Elevated AST (>35 U/L) 2/17 (11.7% and 12-39)
Table 2: Clinical details of pregnant women infected with COVID-19 Parameter Average (Percent and/or range) Comments
Birth weight (g) 3104.375 (2300-3750) Birth weight for the majority of neonates was normal. However, 3/17
neonates had weight lower than 2700g
Birth length (cm) 49.176 (45-52) Birth length was found normal for all of the neonates.

8
Apgar score 9-10 16/17 (94.1% ) Only one of the neonates had lower Apgar score 7-9 at 1 min and 5
min.
Fetal heart rate (Normal) 17/17 (100%)
All the neonates born with a normal heart rate and normal
cardiopulmonary function
Ultrasound results (Normal) 17/17 (100%)
Preterm delivery 3/17 (18%) Preterm delivery was not common, while the risk factors for the three
reported preterm cases were unidentified
Neonatal death 0/17 (0%) No neonatal death and stillbirth occurred among the delivered babies.
Although no neonate was confirmed with COVID-19, two neonates
were suspected of being infected. 1 of the suspected neonates
developed neonatal pneumonia. However, based on lack of evidence
we could not confirm if the virus was transferred from mother to the
suspected neonates
Still birth 0/17 (0%)
Infected with COVID-19 0/17 (0%)
Neonatal pneumonia 5/17 (29%)

Table 1: Clinical details of pregnant women infected with COVID-19
Parameter Average (% and/or range) Comments Pregnant women occupation Health workers 3/17 (17.6%) Nurses and nephrologists were included in this study Non-health workers 14/17 (82.4) Pregnant women who were not related to medical profession General information Age (Years) 29.29 (24-34) Date of hospital admission Jan 25 to Feb 15 All the women were admitted from 25th January to 15th February.
Gestational age on admission (weeks+days) 37.82 (35-41) Majority of the women had gestational age 38-40 weeks Gestational age on delivery (weeks+days) 38.1 (35+5-41) Majority of the women had gestational age 38-40 weeks Number of days from onset of pneumonia until birth
4.2 (1-26) Only two women had 10 or more days of fetuses’ exposure to COVID-19 infection
Source of COVID-19 infection Contact with family infected member 2/17 (12%) Only two individuals were infected with COVID-19 before admission
Contact with infected patient 15/17 (88%) Majority of individuals including healthcare workers contracted infection inside the hospital
Mode of delivery and complications C-section 17/17 (100%) All the women had C-section, however, some of the women had
premature rupture of fetal membrane thus, underwent emergency C-section
Complications 5/17 (29%) Only five pregnant women had complications that caused preterm delivery
Signs and symptoms Maximum body temperature 38.5 °C
The minimum body temperature was 36.2 °C, where the majority of patient had a body temperature approximately 37 °C. Majority of the patients did not develop fever until the delivery, while sputum, shortness of breath and nasal congestion were rare. Comparatively, more
Fever 3/17 (18%) Cough 6/17 (35%) Diarrhea 3/17 (18%) Shortness of breath 2/17 (12%)

Nasal congestion 2/17 (12%) individuals had cough.
Sputum 1/17 (6%) Infected with COVID-19 17/17 (100%) Treatment/ Therapy Antiviral 16/17 (94%) Antiviral drugs oseltamivir or arbidol or both were given orally, while
Ribavirin was given intravenously according to the severity of symptoms. Antibiotics 17/17 (100%) Cefoperazone sulbactam sodium, Ceftazidime, Azithromycin, and
Moxifloxacin hydrochloride were given to the patients who needed it. Hormones 8/17 (47%) Chinese medicine 15/17 (88%) All those receiving Chinese medicine received Lianhua Qingwen.
Laboratory characteristics
Confirmatory (quantitative RT-PCR) test 12/17 (70.5%) Overall 12 women were confirmed only with qPCR testing for nucleic acid form pharynx swab samples.
Confirmatory (quantitative RT-PCR) test + Chest CT scan
5/17 (29.5%) 5 out of 17 patients were confirmed both with qPCR testing for nucleic acid from pharynx swab samples and chest CT scanning
Low or normal leukocyte count (<9·5 × 10⁹ cells per L)
9/17 (52.9% and5.03-19.97) The increased leukocyte count was observed in 8 patients. This increase may or may not be linked to COVID-19 infection.
Lymphocyte count (× 10⁹ cells per L) 4/17 (23.5% and 0.63-2.37) 4 out of 17 patients were found with lymphopenia, which could be linked with COVID-19 infection
Elevated ALT (>45 U/L) 2/17 (11.7% and 9-46) Two out of 17 patients were found with elevated AST and/or ALT. however, the majority of the patients had normal ALT and AST levels. Elevated AST (>35 U/L) 2/17 (11.7% and 12-39)

Table 2: Clinical details of pregnant women infected with COVID-19 Parameter Average (Percent and/or range) Comments
Birth weight (g) 3104.375 (2300-3750) Birth weight for the majority of neonates was normal. However, 3/17
neonates had weight lower than 2700g
Birth length (cm) 49.176 (45-52) Birth length was found normal for all of the neonates.
Apgar score 9-10 16/17 (94.1% ) Only one of the neonates had lower Apgar score 7-9 at 1 min and 5
min.
Fetal heart rate (Normal) 17/17 (100%)
All the neonates born with a normal heart rate and normal
cardiopulmonary function
Ultrasound results (Normal) 17/17 (100%)
Preterm delivery 3/17 (18%) Preterm delivery was not common, while the risk factors for the three
reported preterm cases were unidentified
Neonatal death 0/17 (0%) No neonatal death and stillbirth occurred among the delivered babies.
Although no neonate was confirmed with COVID-19, two neonates
were suspected of being infected. 1 of the suspected neonates
developed neonatal pneumonia. However, based on lack of evidence
we could not confirm if the virus was transferred from mother to the
suspected neonates
Still birth 0/17 (0%)
Infected with COVID-19 0/17 (0%)
Neonatal pneumonia 5/17 (29%)