Assessment Cardiac System
Transcript of Assessment Cardiac System

ASSESSMENT ASSESSMENT CARDIAC SYSTEMCARDIAC SYSTEM
By: Esperancita A. Ferrer RN By: Esperancita A. Ferrer RN MDMD

HEALTH HISTORY ANDHEALTH HISTORY ANDCLINICAL CLINICAL
MANIFESTATIONSMANIFESTATIONS

HEALTH HISTORYHEALTH HISTORY
Include subjective informationInclude subjective information Biographic and demographic dataBiographic and demographic data
– age, gender, and ethnic origin Current healthCurrent health
– Height, current weight, and usual weight
CHIEF COMPLAINTIs the reason why the patient came to the hospital. It should be recorded in quotation marks exactly as stated. ( e.g. “Shortness of breath for 1 week”)

Cardiac Signs and Symptoms:
Chest pain or discomfortChest pain or discomfort (angina pectoris, MI, VHD)
Shortness of breath or dyspneaShortness of breath or dyspnea (MI,LVF, HF)
Edema and weight gainEdema and weight gain (RVF, HF) PalpitationsPalpitations (dysrhythmias resulting from
myocardial ischemia, VHD, ventricular aneurysm, stress, electrolyte imbalance)
FatigueFatigue (earliest symptom associated with several CVS disorder)
Dizziness and syncope or loss of Dizziness and syncope or loss of consciousnessconsciousness (postural hypotension, dysrhythmias, vasovagal effect, cerebrovascular disorders)

Points to remember Points to remember when assessing when assessing
patients with cardiac patients with cardiac symptomssymptoms

Women present with atypical symptoms
Elderly people and those with diabetes may not have pain with angina or MI because of neuropathies. Fatigue and shortness of breath predominant symptoms.
Patient may have more than one clinical condition occurring simultaneously.
Patient with a history of CAD, the chest discomfort should be assumed to be secondary to ischemia

HISTORY OF PRESENT HISTORY OF PRESENT ILLNESSILLNESS OnsetOnset CharacterCharacter SeveritySeverity LocationLocation DurationDuration Frequency of signs and symptomsFrequency of signs and symptoms Associated complaintsAssociated complaints Precipitating, aggravating, and relieving Precipitating, aggravating, and relieving
factorsfactors Progression, remission, and Progression, remission, and
exacerbationexacerbation

Note:Note:
When taking HPI be guided with When taking HPI be guided with the questions in the questions in Table 26-3 • Asking Questions to Evaluate Cardiac Problems

Past Health HistoryPast Health History– Risk factorsRisk factors– Major illness and surgical history Major illness and surgical history – Allergies Allergies – Medications Medications – Dietary habitsDietary habits– Childhood and infectious diseasesChildhood and infectious diseases– Past illnessesPast illnesses
Family HistoryFamily History– Genetic abnormalities associated Genetic abnormalities associated
with cardiovascular disorders. E.g. with cardiovascular disorders. E.g. Familial HypercholesterolemiaFamilial Hypercholesterolemia

Psychosocial HistoryPsychosocial History– StatusStatus– Number of childrenNumber of children– Occupation Occupation – Hobbies Hobbies – Self-perception and self-concept– Coping and stress tolerance

Evaluate the following:
1. Effectiveness of the heart as a Effectiveness of the heart as a pumppumpIf there is presence of the following:– Reduced pulse pressure– Cardiac enlargement– Murmurs– Gallop rhythms
Cardiac insufficiencyCardiac insufficiency

2. Filling volumes and pressuresFilling volumes and pressuresare estimated by:– degree of jugular vein distention– presence or absence of congestion in the
lungs– peripheral edema– postural changes in BP
3. Cardiac outputCardiac outputreflected by:- cognition- heart rate
- pulse pressure – color
- texture of the skin - urine output

4. Compensatory mechanismsCompensatory mechanismshelp maintain cardiac output- increased filling volumes
- elevated heart rate

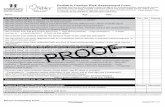
PHYSICAL ASSESSMENT

(1) general appearance(2) cognition(3) skin(4) BP (5) arterial pulses (6) jugular venous pulsations and
pressures(7) heart (8) extremities (9) lungs(10) abdomen

General Appearance and Cognition Level of distress Level of consciousness Thought processes

Inspection of the SkinCommon findings associated with CVS
disease: PallorPallor (a decrease in the color of the skin)
– lack of oxyhemoglobin. – best observed around the fingernails, lips,
and oral mucosa.– In patients with dark skin, nurse observes the
palms of the hands and soles of the feet. Peripheral cyanosisPeripheral cyanosis (bluish tinge)
– Suggests a decreased flow rate of blood to a particular area
– Observed in the nails, skin of the nose, lips, earlobes, and extremities

Central cyanosisCentral cyanosis – Venous blood passes through the
pulmonary circulation without being oxygenated
– Observed in the tongue and buccal mucosa
– Indication of: pulmonary edema and congenital heart disease
Xanthelasma Xanthelasma ((yellowish, slightly raised plaques in the Skin) – observed nasal portion of one or both
eyelids – Indicate hypercholesterolemia

Reduced skin turgorReduced skin turgor – occurs with dehydration and aging
Cold and clammyCold and clammy– In acute MI, diaphoresis is common.
EcchymosisEcchymosis (bruise)– Patients receiving anticoagulant
therapy should be carefully observed for unexplained ecchymosis.
– Excessive bruising indicates prolonged clotting times (PTT & PT)

Blood Pressure
Systemic arterial BP is the pressure exerted on the walls of the arteries during ventricular systole and diastole.
Expressed as the ratio of the systolic pressure over the diastolic pressure

Seventh Joint National Seventh Joint National Committee ClassificationCommittee Classification
Hypertension Hypertension Systolic (mmHg)Systolic (mmHg) Diastolic Diastolic (mmHg)(mmHg)
CategoryCategory
NormalNormal <120<120 and <80and <80
Prehypertension Prehypertension 120 – 139120 – 139 or 80 – 89or 80 – 89
HypertensionHypertension
Stage 1 (mild)Stage 1 (mild) 140 – 159 140 – 159 or 90 – 99 or 90 – 99
Stage 2 Stage 2
(moderate-(moderate-
severe) severe) >160 >160 or > 100 or > 100

PULSE PRESSUREPULSE PRESSUREDifference between the systolic & diastolic pressureNormal:30 to 40 mm Hg
When is Pulse Pressure increased or decreased?When is Pulse Pressure increased or decreased?
Increased Pulse Increased Pulse PressurePressure
1. 1. ↑ SV↑ SV (anxiety, exercise, bradycardia)2. ↓ SVR↓ SVR (fever)3. ↓↓ distensibility of distensibility of the arteriesthe arteries (atherosclerosis, aging, HPN)
Decreased Pulse Decreased Pulse PressurePressure1. ↓ SV & ↓ SV & ejection ejection velocityvelocity (shock, HF, hypovolemia, mitral regurgitation)2. obstruction to blood obstruction to blood flow during systoleflow during systole (mitral or aortic stenosis)
Pulse pressure of <30 Pulse pressure of <30 mmHg indicatesmmHg indicates↓ CO↓ CO

POSTURAL BLOOD PRESSURE CHANGESPOSTURAL BLOOD PRESSURE CHANGESPostural (orthostatic) hypotension- There is a postural decrease from the supine to standing position of at least 20 mmHg in systolic or 10 mmHg in diastolic BP sustained for at least 3 min- S/Sx:S/Sx: dizziness, lightheadedness, or syncope.
Most common cause:1. Due to an Autonomic Dysfunction. 2. Due to a reduced volume of blood in the
circulatory system (e.g., intravascular volume depletion, dehydration)
3. Due to inadequate vasoconstrictor mechanism

Arterial Pulses
Factors to be evaluated:1. Rate2. Rhythm3. Quality4. Configuration of the pulse wave5. Quality of the arterial vessel

PULSE RATEPULSE RATENormal 60-100bpmIn healthy young athletes 50 bpm
PULSE RHYTHMPULSE RHYTHMRegular or irregularSinus arrhythmia in young individuals is normal. ↑PR in inhalation ↓PR in exhalation
Note:Note: In initial cardiac examination: HR
should be counted by auscultating the apical pulse for a full minute while simultaneously palpating the radial pulse

PULSE QUALITYPULSE QUALITYassessed bilaterally
Scales can be used to rate the strength of the pulse:Scales can be used to rate the strength of the pulse:0 pulse not palpablenot palpable or absent+1 weak, threadythready pulse; difficult to palpate;
obliterated with pressure+2 diminisheddiminished pulse; cannot be obliterated+3 easy to palpate, fullfull pulse; cannot be
obliterated+4 strong, boundingbounding pulse; may be
abnormal



PULSE CONFIGURATIONPULSE CONFIGURATION Best appreciated by palpating the carotid carotid
artery.artery.In conditions such as:1. Aortic stenosisAortic stenosis: pulse pressure is narrow, and the pulse feels feeble2. Aortic insufficiencyAortic insufficiency: rise of the pulse wave is abrupt and strong, and its fall is precipitous—a “collapsing” or “water hammer”“collapsing” or “water hammer” pulse.
EFFECT OF VESSEL QUALITY ON PULSEEFFECT OF VESSEL QUALITY ON PULSE Assessment of the quality of the vessel by
palpating along the radial artery and comparing it with normal vessels.
Arteries in the extremities are often palpated simultaneously

Jugular Venous Pulsations
An estimate of right-sided heart function. This provides a means of estimating central venous central venous pressurepressure (CVPCVP)
CVPCVP reflects right atrial or right ventricular end-right atrial or right ventricular end-diastolic pressurediastolic pressure (the pressure immediately preceding the contraction of the right ventricle).
Normally:Normally: Jugular veins are distended when supine once HOB is elevated to 30 degrees it disappears
Abnormal:Abnormal: Jugular veins distended when patient’s head elevated 45 degrees to 90 degrees. An indication of right-sided HFright-sided HF

HEART

Inspection & Palpation In adult heart lies behind & to the In adult heart lies behind & to the left of the left of the
sternumsternum. A small portion of the right atrium . A small portion of the right atrium extends to the right of the sternum. extends to the right of the sternum.
The heart lies in a rotated position within the chest cavity, the right ventricleright ventricle lies anteriorlyanteriorly (just beneath the sternum) and the left left ventricleventricle is situated posteriorlyposteriorly.
BASEBASE- Both atria; lies toward the back- Both atria; lies toward the back
APEX-APEX- ventricles; points anteriorly ventricles; points anteriorly Apex of left ventricle touches the wall or 5Apex of left ventricle touches the wall or 5thth
ICS LMCL, (below left nipple). This area is ICS LMCL, (below left nipple). This area is called PMIcalled PMI

PrecordiumPrecordium
The area on the anterior chest The area on the anterior chest overlying the heartoverlying the heart

Correct position for examination Correct position for examination of the precordiumof the precordium



What to observe for?What to observe for? LIFT or HEAVELIFT or HEAVE appears to lift the hand from
the chest wall during palpation A broad or A broad or forceful apical impulse.forceful apical impulse.
Enlargement of LV-Enlargement of LV- heave lateral to the heave lateral to the apexapex
Enlargement of RV-Enlargement of RV- heave at or near heave at or near sternumsternum
THRILL THRILL abnormal, turbulent blood flow within the heart may be palpated with the palm of the hand as a purring sensation.

Chest Percussion Purpose: To Purpose: To detect enlargementdetect enlargement of the
heart to either the left or right Only the left border of the heart can
be detected by percussion. It extends from the sternum to the
MCL in the 3rd to 5th ICS.

MitralMitral AorticAortic-- --
Cardiac Auscultation

TricuspidTricuspid PulmonicPulmonic

ATRIOVENTRICULAR VALVES: AVVATRIOVENTRICULAR VALVES: AVVSeparate atrium & ventriclesSeparate atrium & ventriclesTricuspid Valve & Mitral ValveTricuspid Valve & Mitral Valve
SEMILUNAR VALVES: SLVSEMILUNAR VALVES: SLVThe valve between right ventricle & pulmonary The valve between right ventricle & pulmonary
artery- Pulmonic Valveartery- Pulmonic ValveThe valve between left ventricle & the aorta- The valve between left ventricle & the aorta-
Aortic ValveAortic Valve
SYSTOLESYSTOLE AVV closeAVV close DIASTOLEDIASTOLE AVV AVV openopen
SLVSLV openopen SLV SLV closecloseS1S1 S2 S2lublub dub dub

Heart SoundsHeart SoundsS1—First Heart Sound.S1—First Heart Sound.
– Closure of the mitral and tricuspid valves
– is heard best at the apex of the heart (apical area)
S2—Second Heart Sound.S2—Second Heart Sound.– Closing of the aortic
and pulmonic valves– heard loudest at the
base of the heart.
S1 & S2 are Normal S1 & S2 are Normal Heart SoundsHeart Sounds

S3-Third Heart SoundS3-Third Heart Sound– Gallop sounds– occur early in diastole during rapid ventricular
filling– Normal in children and young adults– Abnormal finding in CHFCHF– heard best with the patient lying on the left side
S4-Fourth Heart SoundS4-Fourth Heart Sound– Gallop sounds heard during atrial contraction– heard when the ventricle is enlarged or
hypertrophied and therefore resistant to filling– Abnormal finding in HPN, Aortic valve Stenosis, CADHPN, Aortic valve Stenosis, CAD
Note:Note: Gallop sounds are low-frequency sounds heard only
with the bellbell of the stethoscope placed very lightly against the chest.
They are heard best at the apex

Snaps and Clicks.Snaps and Clicks.– SNAP: StenosisStenosis of the mitral valvemitral valve resulting from RHD
gives rise to a unusual high-pitched sound heard best along the left sternal border.
– EJECTION CLICK: StenosisStenosis of the aortic valveaortic valve gives rise to a short, high-pitched sound immediately after S1
MurmursMurmurs – are created by the turbulent flow of blood.
Caused by: 1. narrowed valve2. a malfunctioning valve that allows regurgitant blood
flow3. congenital defect of the ventricular wall4. a defect between the aorta and the pulmonary artery5. an increased flow of blood through a normal structure

Friction Rub.Friction Rub.– a harsh, grating sound that can be heard
in both systole and diastole.– Seen in PericarditisPericarditis.– heard best using the diaphragmdiaphragm of the
stethoscope, with the patient sitting up and leaning forward.

Inspection of the Extremities Observe for skin and vascular changes:
1. ↓↓ capillary refill time capillary refill time2. Vascular changes:Vascular changes: ↓ in quality or loss
of pulse, discomfort or pain, paresthesia, numbness, ↓ in temperature, pallor, & loss of movement.
3. HematomaHematoma-localized collection of clotted blood in the tissue

4. Peripheral edemaPeripheral edema is fluid accumulation in dependent areas of the body.Seen in HF or DVT or Chronic Venous HF or DVT or Chronic Venous InsufficiencyInsufficiency
5. 5. Clubbing of the fingers and toesClubbing of the fingers and toes implies chronic Hgb desaturation. Seen in congenital heart diseasecongenital heart disease.
6. Lower extremity ulcersLower extremity ulcers are observed in patients with arterial or venous arterial or venous insufficiency.insufficiency.

LUNGSFindings frequently exhibited by cardiac patients include the following:1. 1. TachypneaTachypnea
– Rapid, shallow breathing. Seen in HFHF
2. 2. Cheyne-Stokes respirationsCheyne-Stokes respirations – rapid respirations alternating with apnea.
Seen in LVFLVF
3. 3. Hemoptysis Hemoptysis – Pink, frothy sputum is indicative of acute acute
pulmonary edemapulmonary edema.

4. 4. Dry, hacking coughDry, hacking cough– irritation of small airways is common in
patients with pulmonary congestion from pulmonary congestion from HFHF.
5. 5. CracklesCrackles– discrete, noncontinuous sounds that result
from delayed reopening of deflated airways
– Heard in HFHF
6. 6. WheezesWheezes– Compression of the small airways by
interstitial pulmonary edemapulmonary edema

ABDOMENWhat to assess for?What to assess for?1. Hepatojugular reflux:Hepatojugular reflux: Procedure: pressing firmly over the RUQ of the
abdomen for 30 to 60 seconds and noting a rise of 1 cm or more in jugular venous pressure.
Liver engorgementLiver engorgement occurs because of decreased venous return secondary to RVF.
2. Bladder distention:2. Bladder distention: Procedure: Procedure: palpate for an oval mass and percuss
for dullness Urine output is an important indicator of cardiac
function, especially when urine output is reduced.
This may indicate inadequate renal perfusion

AEF 01-23-09














![Cardiac Assessment _ Algorithms [Compatibility Mode]](https://static.fdocuments.net/doc/165x107/577cc8a01a28aba711a3215a/cardiac-assessment-algorithms-compatibility-mode.jpg)



