Annurev.pathol NOD
Transcript of Annurev.pathol NOD
-
8/6/2019 Annurev.pathol NOD
1/36
NOD-Like Receptors:Role in Innate Immunityand Inflammatory Disease
Grace Chen, Michael H. Shaw, Yun-Gi Kim,and Gabriel Nunez
Departments of Pathology and Internal Medicine and the Comprehensive Cancer CenterUniversity of Michigan Medical School, Ann Arbor, Michigan 48109;email: [email protected]; [email protected]; [email protected]; [email protected]
Annu. Rev. Pathol. Mech. Dis. 2009. 4:36598
First published online as a Review in Advance onOctober 17, 2008
The Annual Review of Pathology: Mechanisms ofDisease is online at pathmechdis.annualreviews.org
This articles doi:10.1146/annurev.pathol.4.110807.092239
Copyright c 2009 by Annual Reviews.All rights reserved
1553-4006/09/0228-0365$20.00
Key Words
caspase-1, Crohns disease, IL-1, NOD2, NLRP3
Abstract
The NOD-like receptors (NLRs)are a specialized group of intracellulareceptorsthatrepresentakeycomponentofthehostinnateimmunesys
tem. Since the discovery of the first NLR almost 10 years ago, the studof this special class of microbial sensors has burgeoned; consequently,
better understanding of the mechanism by which these receptors recog
nize microbes and other danger signals and of how they activate inflammatory signaling pathways has emerged. Moreover, in addition to theiprimary role in host defense against invading pathogens, their ability t
regulate nuclear factorkappa B (NF-B) signaling, interleukin-1-bet(IL-1) production, and cell death indicates that they are crucial to th
pathogenesis of a variety of inflammatory human diseases.
365
-
8/6/2019 Annurev.pathol NOD
2/36
PAMPs: pathogen-associated molecularpatterns
PRRs: pathogenrecognition receptors
LPS:lipopolysaccharide
PGN: peptidoglycan
TLRs: Toll-likereceptors
INTRODUCTION
Essential to human survival is the ability toeradicate pathogenic microorganisms. To en-
sure the efficient detection and removal ofharmful microbes, two effector mechanisms
have evolved: the innate and adaptive im-mune systems. The adaptive immune response
is characterized by a delayed response involv-ing gene rearrangements for the clonal se-lection and expansion of T cell and B cell
lymphocytes with antigen-specific receptors.This process results in the generation of a di-
verse, yet specific repertoire of immune effec-tors that also contribute to immunologic mem-
ory. The innate immune system, however, israpidly activated and does not require the so-
matic gene rearrangements that form the cor-nerstone of adaptive immunity. It represents
one of the first lines of defense against microor-ganisms, whereby conserved microbial struc-
tures known as pathogen-associated molecularpatterns (PAMPs) are recognized by germline-
encoded innate immune receptors, also known
as pathogen recognition receptors (PRRs). Ex-amples of PAMPs include lipopolysaccharides
(LPS), peptidoglycan (PGN), flagellin, and mi-crobial nucleic acids. Recognition of these
PAMPs by PRRs results in the activation ofsignaling pathways, which promotes an inflam-
matory, antimicrobial response. Emerging datahave also demonstrated a link between the in-
nate PRRs and the activation of the adaptiveimmune response that can act in concert in de-
fense against invasive organisms (1). Moreover,it has also become apparent that these recep-
tors are involved in sensing not only invading
pathogens, but also endogenous nonmicrobialdanger or stress signals, both of which re-
sult in the activation of inflammatory signal-ing pathways such as nuclear factorkappa B
(NF-B) and mitogen-activatedproteinkinases(MAPKs). This upstream link to complexeffec-
tor pathways highlights the importance of theseimmune receptors in both microbial defense
and the pathogenesis of noninfectious, inflam-matory diseases when signaling becomes dys-
regulated.
Three major classes of PRRs have b
identified: (a) the Toll-like receptors (TLR which are transmembrane proteins with
extramembranous domain involved in land recognition on either the extracellu
surface or within endosomes and a cytopl
mic domain involved in signal transducti(b) the NOD-like receptors (NLRs), which
intracellular, cytoplasmic sensors; and (c) tretinoid acidinducible gene1 (RIG-1)-l
receptors (RLRs), which are cytosolic helicathat primarily sense viruses. Historically,
TLRs were first recognized for their rolehost defense, but the importance of NLRs
complementing the functions of the TLRs become increasingly clear. The high evoluti
ary conservation of the NLRs attests to theirficacy and vitality in host defense. Homologs
the NLRs (e.g., R genes) have been discove
throughout the plant and animal kingdomincluding phylogenetically primitive organis
such as the zebrafish (2) and the sea urchwhich has at least 203 identified putative NL
(3).
DEFINING FEATURES OF THENOD-LIKE RECEPTOR FAMILY
In humans, the NLR family is composed of
proteins ( Table 1), and there are at least NLR genes in mice. Although primarily
pressed in immune cells, including both lyphocytes and antigen-presenting cells (APC
such as macrophages and dendritic cells, NL
can also be expressed in nonimmune cells, cluding epithelial and mesothelial cells. T
family of proteins is defined by a triptite structure consisting of (a) a variable
terminal protein-protein interaction domadefined by the caspase recruitment dom
(CARD), pyrin domain (PYD), acidic transtivating domain, or baculovirus inhibitor
peat (BIR); (b) a central nucleotide-bindoligomerization (NOD) domain, which me
ates self-oligomerization that occurs during tivation (4); and (c) a C-terminal leucine-r
repeat (LRR) that detects PAMPs.
366 Chen et al.
-
8/6/2019 Annurev.pathol NOD
3/36
Table 1 NOD-like receptor (NLR) family members
HGNC-approved symbol
Human Mouse Other names and aliases Domain organization NLR family
CIITA Cllta NLRA; MHC2TA; C2TA
Nlra; MHC2TA; C2TA NLRA
NAIP NLRB1; BIRC1; CLR5.1
Naip1 Birc1a
Naip2 Birc1b Naip3 Birc1c
NLRB Naip4 Birc1d
Naip5 Birc1e
Naip6 Birc1f
Naip7 Birc1g
NOD1 NLRC1; CARD4; CLR7.1NLRC
Nod1 Nlrc1; Card4
NOD2 NLRC2; CARD15; CD;
BLAU; IBD1; PSORAS1;
CLR16.3
NLRC
Nod2 Nlrc2; Card15
NLRC3 NOD3; CLR16.2
NLRC Nlrc3 CLR16.2
NLRC4 CARD12; CLAN; CLR2.1;
IPAF NLRC
Nlrc4 Card12; CLAN; Ipaf
NLRC5 NOD27; CLR16.1NLRC
NIrc5
NLRP1 NALP1; DEFCAP; NAC;
CARD7; CLR17.1
Nlrp1a NALP1
NLRPNlrp1b
Nlrp1c NLRP2 NALP2; PYPAF2; NBS1;
PAN1; CLR19.9 NLRP
Nlrp2 Pypaf2; Nbs1; Pan1
NLRP3 CIAS1; PYPAF1; Cryopyrin;
NALP3; CLR1.1 NLRP
Nlrp3 Cias1; Pypaf1; Cryopyrin;
Nalp3; Mmig1
NLRP4 NALP4; PYPAF4; PAN2;
RNH2; CLR19.5
Nlrp4a Nalp4a; Nalp-eta; Nalp9D
Nlrp4b Nalp4b; Nalp-gamma; Nalp9ENLRP Nlrp4c Nalp4c; Nalp-alpha; Rnh2
Nlrp4d Nalp4d; Nalp-beta
Nlrp4e Nalp4e; Nalp-epsilon
Nlrp4f Nalp4f; Nalp-kappa; Nalp9F
Nlrp4g Nalp4g
(Continued
www.annualreviews.org NLRs: Role in Immunity and Disease 367
-
8/6/2019 Annurev.pathol NOD
4/36
Table 1 (Continued)
HGNC-approved symbol
Human Mouse Other names and aliases Domain organization NLR famil
NLRP5 NALP5; PYPAF8; MATER;
PAN11; CLR19.8 NLRP
Nlrp5 Mater; Op1
NLRP6 NALP6; PYPAF5; PANS;
CLR11.4NLRP
Nlrp6 NLRP7 NALP7; PYPAF3; NOD12;
PAN7; CLR19.4 NLRP
NLRP8 NALP8; PAN4; NOD16;
CLR19.2 NLRP
NLRP9 NALP9; NOD6; PAN12;
CLR19.1
Nlrp9a Nalp9a; Nalp-thetaNLRP Nlrp9b Nalp9b; Nalp-delta
Nlrp9c Nalp9c; Nalp-zeta
NLRP10 NALP10; PAN5; NOD8;
PYNOD; CLR11.1 NLRP
Nlrp10 Nalp10; Pynod NLRP11 NALP11; PYPAF6; NOD17;
PAN10; CLR19.6 NLRP
NLRP12 NALP12; PYPAF7; Monarch1;
RNO2; PAN6; CLR19.3 NLRP
Nlrp12 Nalp12
NLRP13 NALP13; NOD14; PAN13;
CLR19.7 NLRP
NLRP14 NALP14; NOD5; PAN8;
CLR11.2 NLRP
Nlrp14 Nalp14; Nalp-iota; GC-LRR
NLRX1 NOD9; CLR11.3
NLRX
The N-terminal domain of the NLRsis critical for downstream signaling. CARDdomains were originally associated with pro-
teins involved in apoptosis and inflammationsuch as many of the caspases, including caspase-
1; however, CARDs have also been shownto mediate caspase-independent interactions.
The structure of PYD is homologous to tof CARD and promotes homophilic intactions with other PYD-containing prote
that are important for downstream signalevents. Both CARD and PYD are members
the death domainfold superfamily, membof which are involved in both apoptosis a
368 Chen et al.
-
8/6/2019 Annurev.pathol NOD
5/36
inflammation. Finally, the BIR-containing pro-
teins can be classified into two major groups,
inhibitor of apoptosis proteins (IAPs) and neu-ronal apoptosis inhibitor proteins (NAIPs),
both of which are NLR family members. Be-cause of the variety in domain structures for
each NLR, the nomenclature of the differentNLRs has been inconsistent and confusing. Re-
cently, in order to promote uniformity in thenomenclature of the various NLRs, a new sys-
tem approved by the Human Genome Orga-nization Gene Nomenclature Committee was
established (5). This new annotation systemrecognizes the evolutionarily conserved NOD
and LRR domains that are the central defin-
ing features of these PRRs, but it further sub-divides the NLR family into four subfamilies
(indicated by letters A through C and P) basedon the type of N-terminal effector domain
(Table 1). An additional subfamily, NLRX, hasno strong homology to the N-terminal domain
of any of the other four subsets and currentlyconsists of only one member, NLRX1 (Nod9),
which appears to be unique in its localization tothe mitochondria (6, 7).
NOD-LIKE RECEPTORSIGNALING: DIVERSE ANDCOMPLEX PATHWAYS WITH
MULTIPLE LEVELSOF REGULATION
In general, the primary function of PRRs is theactivation of inflammatory signaling pathways.
In some respects, NLR signaling is very sim-ilar to that of the TLRs, with shared down-
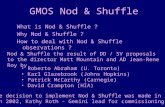
stream targets (Figure 1). For example, uponrecognition of their respective PAMPs, the pri-
marily membrane-bound TLRs recruit adaptorproteins such as MyD88 and TRIF, which acti-
vate the MAPK and NF-B signaling pathways,
resulting in the induction of proinflammatoryand antimicrobial mediators such as interleukin
(IL)-6, tumor necrosis factor alpha (TNF-),and IL-1 (for a review, see Reference 8). Sim-
ilarly, stimulation of the intracellular NLRs ac-tivates downstream signaling pathways for the
production of proinflammatory mediators to
defend the host against infection. However, the
end targets of NLR signaling are not the samefor all NLRs. Three major activation targets of
NLR signaling after PAMP recognition have
been identified: (a) NF-B, (b) MAPKs, and(c) caspase-1 (Figure 1).
Nuclear FactorKappaB/Mitogen-ActivatedProtein Kinase Signaling
The earliest-identified and best-characterized
NLRs are NOD1 and NOD2, which are pro-totypical of NLR activation of both the NF-
B and MAPK pathways (912). Upon recog-
nition of their respective agonists, both NOD1and NOD2 self-oligomerize to recruit and ac-
tivate the adaptor protein RICK (also knownas RIP2), which is essential for the activation
of both NF-B and the MAPKs (4, 10, 1316). RICK is a serine-threonine kinase that be-
comes polyubiquitinated upon interaction withNOD1 or NOD2 through homotypic CARD-
CARD interactions (17). This RICK K63linked ubiquitination step is essential for re-
cruitment of the kinase TAK1, which activatesthe NF-B-activating complex and is inhibited
by the deubiquitinase A20 (17). RICK itself
recruits and promotes the K63-linked polyu-biquitination of the I-kappa-B kinase gamma
(IK) regulator subunit of the IK complex,or NF-B essential modulator (NEMO), which
can also facilitate recruitment of TAK1 in aubiquitin-dependent manner (18). The colo-
calization of NEMO and TAK1 promotes thesubsequent phosphorylation of the IK sub-
unit of IK by TAK1 and results in the phos-phorylation and degradation of IB, a criti-
cal step that allows the cytoplasmic release andnuclear translocation of NF-B (19). NF-B
subsequently activates transcription of inflam-
matory cytokines and chemokines such asTNF-, IL-6, IL-8, and membrane cofactor
protein 1, which are important for stimulationand recruitment of additional effector cells dur-
ing host defense.As has been demonstrated for both NOD1
and NOD2 signaling, ubiquitination plays a
www.annualreviews.org NLRs: Role in Immunity and Disease 369
-
8/6/2019 Annurev.pathol NOD
6/36
a
b
c
Lipoprotein
Flagellin
Viral
dsRNAT
RIF
Endosome
TLR1
or
TLR6
TLR5
TLRs
TLR2
TLR
4
LPS
MyD88
Imiquimod
IRA
K1
IRAK4
TRAF6
TAK1T
AB1
TAB2/3
NEMO
TLR3
TLR7
TLR9
CpGDNA
MKKs
Nucleus
ERK
JNK
IKK
IKK
NF-B
NF-B
R1
r R6
TLR5
7
TLR9
C
TLRs NNN
FNF-FBBB
NF-B
TAK1
TAK1
iE-DAP
MDP
NOD1
N
OD2
RICK
CA
RD9
RICK
CARD9
NLR
inflammasome
Ub
Ub
TAB1 T
AB2/3
TAB1
TAB2/3
NEMO
MKKs
MKKs
p38
JNK
ERK
p3
8
JNK
ERK
IKK
IKK
Pro-IL-1
IL-1
Figure1
Toll-likereceptor(TLR)andNod-likereceptor(NLR)signalingpathways.(a)Extracellularpathogen-associatedmolecularpatterns(PAMPs)
arerecognizedbyTLRsat
theplasmamembranean
dendosomes,whichsignalthroughtheadaptorsMyD88andToll/interleukin-1receptordomain-containingadapter-inducinginterferonbeta
(TRIF),aswellasthroughinterleukin-1receptorassociatedkin
ase(IRAK)proteinsandtumornecrosi
sfactorreceptorassociatedfactor6(TRAF6).(b)TheNLR
proteinsNOD1andNO
D2senseintracellularD--glutyamyl-meso-DAP(iE-DAP)andmuramyldipeptide(MDP),respectively,
leadingtor
ecruitmentoftheadaptor
proteinsRICKandcaspaserecruitmentdomain9(CARD9).Su
bsequently,bothTLRsandNOD1/NO
D2signalingpathwaysrecruitTAK1,whichmediatesthe
activationofnuclearfactorkappaB(NF-B)andmitogen-activ
atedproteinkinases(MAPKs),resultinginthetranscriptionalupregulationof
proinflammatorygenes.
(c)ActivationofNLRsb
ymicrobialorendogenousmoleculesinthecytosolresultsintheformationof
caspase-1-activatinginflammasomes.Activationofcaspase-1
inducesprocessingoftheinterleukin-1-beta(IL-1)precursorandsecretionofthematurecytokine.Abbreviations:ERK,extracellularsignal
regulatedproteinkinase;
IKK,
I-kappa-Bkinase;JNK,c-JunN-terminalkinase;MKK,M
APkinasekinase;NEMO,
NF-Bessentialmodulator.
370 Chen et al.
-
8/6/2019 Annurev.pathol NOD
7/36
key role in activation of downstream signaling.
For NOD2-mediated activation of NF-B in
particular, the E3 ligase tumor necrosis factorreceptorassociated factor 6 (TRAF6) was sug-
gested to be importantbut dispensableforNOD1 signaling, whereas TRAF2 and TRAF5
were essential (17, 20). The significance of thedifferential utilization of E3 ligases for ubiqui-
tination is not clear, but this ligase may provideadditional points of regulation during the in-
duction of inflammatory cytokine production.NOD2 is also additionally regulated by Erbin,
which interacts with NOD2 and is capable ofdownregulating NOD2-dependent activation
of NF-B. However, whether Erbin also reg-
ulates signaling of other NLRs remains to bedetermined (21).
Stimulation of NOD1 and NOD2 also re-sults in the activation of MAPKs, including
the p38, extracellular signalregulated proteinkinase (ERK), and c-Jun N-terminal kinase
( JNK) pathways (Figure 1) (15). In contrastto NF-B, the molecular events that occur for
activation of these pathways are not as well de-fined, but they involve similar upstream signal-
ing molecules such as RICK and TAK1 (15,22, 23). Recent evidence also suggests that the
adaptor protein CARD9 may be particularly
important in NOD2- and RICK-mediated ac-tivation of MAPK pathways and less so for
NF-B (24).Importantly, there are NLR members that,
instead of promoting NF-B activation, mayhave a primarily negative regulatory role. These
members include NLRP12 (25, 26), NLRC3 inT cells (27), and NLRP2 in macrophages (28).
As the studies identifying these members wereall performed in vitro and typically involved
overexpression of proteins or the use of tumorcell lines, the physiologic roles of these NLRs
in vivo remain to be determined.
Biological Responses to NOD-1and NOD-2 Signaling
A consequence of NOD1- and NOD2-mediated activation of NF-B and MAPK is
the upregulatedtranscription and productionof
MDP: muramyldipeptide
inflammatory mediators, including cytokines,
chemoattractants, adhesive molecules, and in-
ducible molecules (e.g., iNOS, Cox-2). ForNOD1 specifically, which is expressed in ep-
ithelial and mesothelial cells, its stimulation caninduce chemokine production and recruitment
of effector immune cells, including neutrophilsin vivo (29, 30). Equally important is the upreg-
ulation of antimicrobial peptide productionespecially in epithelial cells, which may be NF-B dependent, by both NOD1 and NOD2 sig-naling. Disruption of this function may con-
tribute to the pathogenesis of inflammatorydiseases in the bowel (3136). NOD1 signal-
ing is also important in the coordination of an
adaptive immune response by both T and Bcells through synergistic antigen presentation
with TLRs (1). Similarly, a role for NOD2 inmounting adaptive responses is implicated by
the observation that the NOD2 agonist, mu-ramyl dipeptide (MDP), can act as an effective
adjuvant for antigen-specific T cell responsesand antibody production (37, 38).
Aside from the induction of proinflamma-tory mediators, NOD1 and NOD2 have also
been shown to induce apoptosisin in vitro over-expression systems; in fact, these proteins were
originally identified by their structural homol-
ogy to Apaf-1 and CED-4, known regulatorsof apoptosis (13, 14). The specific pathways in-
volved in the induction of apoptosis are not en-tirely clear, but for NOD1 this process involves
both caspase-8 and caspase-9 and requiresRICK. Note, however, that these studies were
all performed in vitro and that functional rele-vanceremainstobeinvestigatedinvivo(13,23).
Interleukin-1 Productionand the Inflammasome
In addition to NF-B and MAPKs, the third
important pathway activated by NLR signalinginvolves ASC (adaptor protein apoptosis speck
protein with caspase recruitment) to activatecaspase-1 (Figure 1). NLRs that participate in
caspase-1 activation include NLRP1, NLRP3,and NLRC4. Caspase-1 activation is required
for the cleavage of pro-IL-1 and pro-IL-18
www.annualreviews.org NLRs: Role in Immunity and Disease 371
-
8/6/2019 Annurev.pathol NOD
8/36
into their mature, biologically active forms. Re-
cruitment of ASC by these NLRs is believed to
occur through homophilic PYD-PYD interac-tions. Via its CARD domain, ASC, in turn, in-
teracts with caspase-1. These protein-proteininteraction domains promote oligomerization,
recruitment,andapproximationofeffectorpro-teins essential for activationof caspase-1 (4, 39).
Indeed, a hallmark of this caspase-1-dependentpathway is the assembly of large macromolec-
ular complexes through CARD-CARD andPYD-PYD protein-protein interactions that
function to form a scaffold for procaspase-1 recruitment and activation. This molecu-
lar platform, of which NLR family members
are the cornerstone, has been termed the in-flammasome (40) as an analogy to the apopto-
some, an activator of caspase-9 duringapoptosis(41).
Currently there are three well-described in-flammasomes named after the NLR involved:
NLRP1, NLRP3, and NLRC4. Common tothese inflammasomes is the role of ASC as the
adaptor protein that bridges these NLRs tocaspase-1 (40, 42). The NLRP1 inflammasome
was the first to be characterized and is the onlyinflammasome that has been reconstituted in
vitro with purified proteins (40, 43). The ex-
istence of the NLRP3 and NLRC4 inflamma-somes, the activities of which are dictated by
the specific PRRs recognized by the NLRs, hasbeen implicated primarily by the ability of both
NLRP3 and NLRC4 to activate caspase-1 in anASC-dependent manner (4450).
OtherNLRmembersthatcanassociatewithprocaspase-1 and promote IL-1 production
such as NLRP2have only been demonstratedin vitro, but whether the latter is a bona fide in-
flammasome that functions to activate caspase-1 during host defense in vivo remains to be
determined (28). NAIP with its BIR domain,rather than its CARD or PYD domain, has also
been shown to be capable of activating caspase-
1 at least for the murine isoform Naip5; how-ever, the relevance of its ability to interact with
caspase-1 and whether it acts alone or togetherwith NLRC4 remain controversial. We discuss
this issue in more detail below.
Another important consequence of caspa
1 activation is the induction of a newly rognized process of programmed cell de
termed pyroptosis, which is distinct from aptosis and necrosis. Pyroptosis is typically
duced in macrophages infected with cert
intracellular bacteria such as Salmonella andassociated with a proinflammatory response
volving caspase-1-mediated IL-1 and IL-production (51). This response causes rapid f
mation of plasma membrane pores, cellular sis, and release of intracellular inflammato
contents to fuel additional inflammatory snaling pathways (52). Caspase-1 activation a
the release of IL-1 and IL-18 have bshown to be particularly important in h
defense against such pathogens as Shig(53), Legionella (48), Francisella (54), Liria (55), Yersinia (56), and Bacillus anthr
(52). How the different inflammasomes enlisted to defend against specific pathoge
or stimuli is described in the followsections.
NOD-LIKE RECEPTORSRECOGNIZE SPECIFICBACTERIAL ANDENDOGENOUS MOLECULES
Although numerous studies have delineated
importance of individual NLRs against specpathogens, a direct interaction between a p
tative ligand and its corresponding NLR hnot been demonstrated for most of the NL
Therefore, the possibility that the interactibetween NLR and PRR is indirect and invol
an intermediary host factor or activity cannbe precluded. In this section, we describe w
is known about the sensing of pathogens by various NLRs (Table 2).
NOD1
Originally, LPS preparations were demostrated to activate both NOD1 and NO
through RICK, but this was recently shownbe due to contamination of LPS preparatio
with PGN moieties (10, 15, 57). Both NO
372 Chen et al.
-
8/6/2019 Annurev.pathol NOD
9/36
Table 2 NOD-like receptor (NLR) agonists and downstream signaling pathwaysa
Receptor Agonist Bacteria Signaling pathway
Nod1 GM-tripeptide Helicobacter pylori NF-B
meso-lanthionine, meso-DAP Shigella flexneri MAPK
-d-Glu-DAP(iEDAP) Listeria monocytogenes
Campylobacter jejuni
d-lactyl-l-Ala--Glu-meso-DAP-Gly (FK156) Enteropathogenic Escherichia coli
heptanolyl--Glu-meso-DAP-Ala (FK565) Chlamydia pneumoniae
Pseudomonas aeruginosa
Bacillusspp.
Nod2 MDP Streptococcus pneumoniae NF-B
MurNAc-l-Ala-g-d-Glu-l-Lys (M-TRILys) Listeria monocytogenes MAPK
Mycobacterium tuberculosis
Salmonella Typhimurium
Staphylococcus aureus
Shigella flexneri
Nlrc4 flagellin (Salmonella, Legionella, Pseudomonas) Salmonella Typhimurium caspase-1
unknown (Shigella) Legionella pneumoniae
Pseudomonas aeruginosa
Shigella flexneri
Listeria monocytogenesb
Naip unknown Legionella pneumophila caspase-1
Pseudomonas aeruginosa
Salmonella
Listeria
Nlrp1b anthrax lethal toxin Bacillus anthracis caspase-1
Nlrp3 bacterial RNA Staphylococcus aureus caspase-1
viral RNA and DNA Listeria monocytogenesb
uric acid crystals
LPS
LTA
MDPsilica
asbestos
aAbbreviations: LPS, lipopolysaccharide; MAPK, mitogen-activated protein kinase; MDP, muramyl dipeptide; NF-B, nuclear factorkappa B.bBoth Nlrc4 and Nlrp3 may play redundant roles in caspase-1 activation in response to this pathogen, as both have been shown to contribute to IL-1
production in vitro.
and NOD2 recognize PGN moieties found
in the bacterial cell that are secreted bybacteria (5861). PGN provides structure and
rigidity to bacteria and is found in virtually
all bacteria, although the amount, location,and specific composition may vary (62).PGN consists of sugar chains of alternating
N-acetylglucosamine (GlcNAc) and N-acetyl
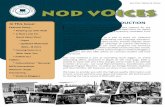
muramic acid (MurNAc), which are cross-linked by short peptide chains (Figure 2).
These peptide chains contain unique aminoacids that are differentially found in gram-
negative and gram-positive bacteria and that
are also differentially recognized by NOD1 andNOD2. Specifically, NOD1 can sense PGN
moieties containing meso-diaminopimelic
acid, an amino acid that is found predomi-nantly in gram-negative bacteria but also insome gram-positive bacteria such as Listeriamonocytogenes and Bacillus spp. The minimalstructure recognized by NOD1 is the dipeptide
D--glutyamyl-meso-diaminolimelic acid (iE-
DAP) (59, 60). Studies defining synthetic iE-DAP derivatives that stimulate NOD1 revealed
www.annualreviews.org NLRs: Role in Immunity and Disease 373
-
8/6/2019 Annurev.pathol NOD
10/36
Plasma membrane
PGN
Lipoteichoic acid
Polysaccharide
Cytosol
Cytosol
LPS Porin
Lipopeptide
Plasma membrane
PGN
Outer membrane
L-alanine
D-glutamic acid
Mesodiaminopimelic acid
D-alanine
Tetra-peptidechain (amino acids)
MDP(Nod2 ligand)
iE-DAP
(Nod1 ligand)Pep
tidoglycan(PGN)
Glycan chain
Gram-negativ
ebacteria
Gram-positivebacteria
NAGNAM NAG NAM
NAG NAMNAG NAM
374 Chen et al.
-
8/6/2019 Annurev.pathol NOD
11/36
that the attachment of hydrophobic acyl
residues enhanced stimulation of NOD1 up to
severalhundredfold(63).Astheseresiduescon-tained fatty acid chains similar to those found
in the phospholipids that make up the hostcell membrane, it is possible that the increased
NOD1-stimulatory activity is due to an in-creased interaction with the cellmembrane that
facilitates translocation into the intracellularcompartment of the host cell (63). The
lipophilicity of the NOD1 ligand appears im-portant for recognition by NOD1, butprecisely
how NOD1 interacts with these lipophilicmolecules and whether this actively contributes
to its transfer and recognition into the host cell
remain to be determined.In vitro studies have demonstrated that
many bacteria have NOD1-stimulatory activ-ity, with the strongest activity associated with
the genus Bacillus (58). Moreover, the pres-ence of bacteria has not always been necessary
for NOD1 stimulation, as water-soluble ex-tracts from food and soil as well as supernatant
from overnight bacterial cultures are capable ofstimulating NOD1 (58). This suggests that
physical contact with live bacteria is not nec-essary and that NOD1 agonists can be pro-
duced and released by bacteria. Consistent
with this observation, Shigella mutants that in-crease release of PGN fragments upregulated
NOD1-dependent NF-B activation in vitro(64). In addition, where and how NOD1 in-
teracts with bacteria are not clear. Localiza-tion of bacteria to the intracellular compart-
ment has been shown to not necessarily berequired for NOD1 stimulation, as the Liste-ria streptolysin O mutant, which is requiredfor Listeria to escape from the phagosome into
the cytosol, is still capable of activating NF-B
in a NOD1-dependent manner (58). Localiza-tion studies of NOD1 through overexpression
have shown that NOD1 becomes membrane
bound, at least during infection with Shigellaflexneri at sites of bacterial entry. However,
whether this occurs in vivo remains to be de-termined, as endogenous NOD1 localization
during infection has been difficult to visualize(65).
Despite the identification of the PGN moi-ety sensed by NOD1, the role of NOD1 dur-
ing in vivo infection remains unclear, with thepartial exception ofHelicobacter pylori, a bacte-
rial organism associated with the developmentof gastritis and duodenal ulcers. Specifically,
Nod1-deficient mice have shown increased sus-ceptibility to H. pylori infection, with an as-
sociated impairment of -defensin-4 produc-
tion (34, 66). In vitro studies, on the otherhand, have shownNOD1-dependent activation
by other pathogenic bacteria such as L. mono-cytogenes (15), S. flexneri (9), Campylobacter je-
juni(36, 67), enteroinvasive Escherichia coli(68),
Chlamydophila pneumonia (69), and Pseudomonasaeruginosa (70). However, these findings werebased on in vitro studies only and may not nec-
essarily reflect requirements in vivo. For exam-ple, NOD1 was originally implicated in pro-
tection against Chlamydia trachomatis infectionin vitro, where Nod1-deficient mouse embry-
onic fibroblasts (MEFs) exhibited decreased cy-
tokine production after C. trachomatisinfection;however, Nod1-deficient mice did not have
increased bacterial load or clinical symptoms,suggesting either that NOD1 is not directly in-
volved or that other redundant signaling path-ways can compensate (71).
Figure 2
Generation of NOD1 and NOD2 ligands from bacterial peptidoglycan (PGN). In this simplified diagram,the bacterial cell wall and PGN structure from Escherichia coliare depicted. Parallel PGN strands composedof the alternating amino sugars N-acetylglucosamine (NAG) and N-acetyl muramic acid (NAM) are cross-linked to each other by stem peptides. Notice that E. coliPGN lacks bridging amino acids linking stempeptides and that cross-linking occurs via a direct link between a meso-diaminolimelic acid (meso-DAP)residue and the d-alanine residue in position four from a peptide anchored on the parallel glycan strand.Minimal motifs required for NOD1 and NOD2 (dashed boxes) recognition are also shown. Abbreviations:iE-DAP, d--glutyamyl-meso-DAP; LPS, lipopolysaccharide; MDP, muramyl dipeptide.
www.annualreviews.org NLRs: Role in Immunity and Disease 375
-
8/6/2019 Annurev.pathol NOD
12/36
NOD2
Separate studies have also demonstrated thatNOD2 can detect pathogenic bacteria. In
contrast to NOD1, which appears to beprimarily involved in sensing gram-negative
bacterial pathogens, NOD2 senses the spe-cific MDP motif that is found in a broader
range of bacteria, with some overlap withthose recognized by NOD1 (Figure 1). These
bacteria include Streptococcus pneumoniae (72),
L. monocytogenes(33, 73), Mycobacterium tuber-culosis (74), Salmonella (75), and Staphylococcus
aureus (76). Again, most of these studies wereperformed in vitro; therefore, the in vivo rel-
evance of these findings remains to be deter-mined. One exception, however, is L. monocyto-
genes, in which increased bacterial burdens wereobserved in Nod2-deficient mice when infected
orally rather than intravenously or intraperi-toneally (33). This immunity is associated with
decreased production of-defensins in Panethcells (33). In addition, both Nod1 and Nod2
have been shown to be important for bacterialrecognition and host defense against L. mono-cytogenesafter exposure of macrophages or an-
imals to LPS or E. coliin vivo (77). These ob-servations suggest that the intracellular sensors
NOD1 and NOD2 play a critical role in hostdefense when TLRsignaling is reduced, such as
within the intestine due to low expression levelsof TLRs (78, 79) or after induction of toleriza-
tion by exposure to TLR ligands.
NLRC4
As mentioned above, a subset of NLRs partic-ipate in the formation of inflammasomes that
ultimately leads to activation of caspase-1 and
maturation of IL-1. To date, these NLRs in-clude NLRC4, NLRP1, and NLRP3. Studies
have shown that the NLRC4 inflammasomecan activate caspase-1 in response to infection
by S. Typhimurium, an activity not shared bythe NLRP3 inflammasome (49, 50). Salmonella
infection can lead to gastroenteritis as well as totyphoid fever, which canbe associated with high
morbidity and mortality. What is recognized
by NLRC4 is flagellin, as flagellin-defici
Salmonella mutants elicit substantially redulevels of caspase-1 activation (49). Similarly,
tosolic detection ofL. monocytogenesby Ipaf
quires flagellin (80). A direct interaction btween flagellin and NLRC4 has not yet be
demonstrated, however, and therefore recogtion is likely indirect. TLR5, a member of t
TLR family, also senses flagellin; howeverhas been shown that the cytoplasmic delivery
flagellin requires NLRC4 but not TLR5, cosistent withits cellular location.As an additio
consequence of caspase-1 activation, caspa1 can lead to early macrophage cell death,
NLRC4-dependent process in the host defeagainst Salmonella (47).
In vivo, NLRC4 has also demonstrated
tivity against Legionella pneumophila, an intcellular pathogen that causes Legionnaires d
ease, which can be deadly. The pathogenesisLegionella requires successful entry and repli
tion inside host macrophages and is dependon the formation of a specialized vacuole th
blocks the fusion of the phagosome to the lysome, a process dependent on an intact fun
tional type IV secretion system (TFSS). Athecasewith Salmonella, Legionella also conta
flagellin, and NLRC4-dependent caspase-1 tivation requires the presence of intact flage
and its intracellular delivery (48, 81). As a
sult of NLRC4-induced caspase-1 activatiLegionella growth is restricted by promoti
the fusion of the Legionella-containing phagsome to thelysosome fordegradation(48).H
caspase-1 activation controls phagosome muration in response to Legionella infection
not known, but it may involve interactioncaspase-1 with host proteins involved in pha
some formation and transport or direct targing ofLegionella virulence factors required
lysosomal evasion.In vitro, NLRC4 is important in respond
to Shigella, an intestinal pathogen that cau
dysentery and, as mentioned above, can aelicit NOD1-dependent MAPK activation a
secretion of IL-8 (9). Like Legionella, Shigcan escape from within membrane vacuo
and enter the cytosol. Interestingly, Shig
376 Chen et al.
-
8/6/2019 Annurev.pathol NOD
13/36
does not express flagellin genes, yet it can ac-
tivate caspase-1 macrophages and induce py-
ropoptosis in an NLRC4-dependent process(82). This suggests that NLRC4 also rec-
ognizes an as-yet-unidentified PAMP or sig-nal associated with Shigella. Shigella also in-
duces autophagy, which is facilitatedin NLRC4but not in ASC-deficient macrophages, sug-
gesting that NLRC4 provides an additionalhost-defense measure independent of ASC and
IL-1 production by inhibiting autophagy (amembrane-trafficking system in which cyto-
plasmic components are sequestered for de-livery to lysosomes, where cytoplasmic ma-
terial is degraded). This downregulation of
autophagy is specific to Shigella-induced au-tophagy, as autophagy from serum starvation or
rapamycin treatment does not require NLRC4or caspase-1 (82). The reason for the inhibi-
tion of autophagy by NLRC4 is not clear, but ithas been proposed that this inhibition allows
the induction of pyroptosis, which may bet-ter promote an effective inflammatory response
(82).
NAIP
One of the mouse homologs of human NAIP,
Naip5, is also important in the host defenseagainst Legionella. This finding arose from
observations that different mouse strainsshow varying permissiveness to intracellular
replication of Legionella and that this permis-siveness is genetically controlled (83, 84). The
genetic locus responsible for the increasedsusceptibility to Legionella infection in the A/J
mouse strain in particular has been determinedto be Naip5 (85). Naip5 promotes the fusion
of the Legionella-containing phagosomes tothe lysosome, thereby preventing intracellu-
lar replication (86). Studies in vitro have also
suggested that Naip5 activation requires the in-tracellular delivery of flagellin, which results in
caspase-1 activation and in promotion of earlycell death, thereby controlling intracellular
replication ofLegionella (81, 87, 88). However,these studies used large numbers of Legionellabacteria, which can lead to nonspecific early
cell death of macrophages; they also used
an indirect, nonspecific method of detectingcaspase-1 activation. In a separate study using
low bacterial load and caspase-1-specific anti-
bodies, Legionella-induced caspase-1 activationand IL-1 production occurred independently
of Naip5 but required Nlrc4 as well as flagellin(89). Naip5, however, was still required for in-
hibition ofLegionella replication intracellularly,irrespective of Nlrc4 signaling; this suggests
a caspase-1-independent pathway regulatedby Naip5 that restricts Legionella replication
and acts in concert with Nlrc4 signaling(89). The PAMP involved in this process has
yet to be determined, as it does not requireflagellin. In addition, Naip5like Nlrc4has
been suggested to regulate autophagy: A/J
mice that harbor mutant Naip5 exhibitedslower rates of autophagy induction after
Legionella infection of macrophages comparedwith Legionella-resistant C57BL/6 that have
intact Naip5 (90). This observation furtherdemonstrates the complexity of intracellular
Legionella replication by different NLRs, and itremains an active area of investigation.
Based on in vitro studies using A/J mice thatare considered Naip5 deficient compared with
C57BL/6, which have intact Naip5 and are re-sistant toLegionella replication, Naip5 also con-
tributes to IL-1 production by bone marrow
derived macrophages after infection withP. aeruginosa, an opportunistic bacteria that can
cause pneumonia and sepsis (91). The decreasein IL-1 production in A/J mice, although
statistically significant, may reflect inherentlydifferent genetic susceptibility differences be-
tween the two mouse strains that are indepen-dent of Naip5; therefore, this decrease may
be physiologically irrelevant in vivo. There-fore, additional studies examining a true
Naip5-knockout strain should provide addi-tional insight into and confirmation of these
findings.
NLRP1
Recently discovered mutations in the Nlrp1
(Nalp1b) gene in various mouse strains have
www.annualreviews.org NLRs: Role in Immunity and Disease 377
-
8/6/2019 Annurev.pathol NOD
14/36
been found to influence the susceptibility of
mice to Bacillus anthracislethal toxin (LT) (92),
the major virulence factor in the pathogen-esis of anthrax. This was the first demon-
stration of an NLR that responds to avirulence factor, as opposed to a specific bacte-
rial component. LT results in the formation ofpores allowing lethal factor, a protease, to enter
cells, resulting in proteolytic cleavage of hostsubstrates and subsequent cell death. Suscepti-
bility to LT-induced macrophage lysis/necrosisand death requires caspase-1 activation and is
associated with Nalp1b polymorphisms. Five ofthese polymorphisms have been identified, ex-
plaining the variability in susceptibility to LT-
induced cell death in different mouse strains(92). Caspase-1 activation by LT results in
pyroptosis similar to that seen in NLRC4-mediated cell death induced by Salmonella
infection (52).The human NLRP1 inflammasome, recon-
stituted with purified proteins including ASC,NLRP1, andprocaspase-1, hasalso beenshown
to respond to MDP and to induce the matura-tion of IL-1. Because only purified proteins
were used in this cell-free system (40), it is pos-sible that, in this case, a direct interaction be-
tween the inflammasome and MDP occurred
under physiological conditions.
NLRP3
NLRP3 is an NLR that also participates ininflammasome formation through the recruit-
ment of ASC and subsequent activation ofcaspase-1 and secretion of IL-1 and IL-18.
NLRP3 detects PAMPs such as LPS, MDP, andbacterial and viral RNA, including the double-
stranded RNA analog poly I:C (4446) as wellas the imidazoquinoline antiviral compounds
R837 and R848 (93). Consistently, NLRP3
has been found to respond to infection withthe Sendai and influenza viruses, resulting in
caspase-1 activation (44). Subsequently, it wasshown that NLRP3 can detect viral DNA (94).
In vitro, NLRP3 has also been demonstrated tobe required for caspase-1 activation/IL-1 se-
cretion in response to the bacterial pathogens
S. aureusand L. monocytogenes(46). However
the case ofL. monocytogenes, the role of NLRhas been controversial, as there are oppos
data to suggest that caspase-1 activation byL
teria can occur independently of NLRP3 (102). This discrepancy may be explained
redundant contributions by both NLRP3 aNLRC4 in caspase-1 activation in response
Listeria (80).Characteristic of NLRP3, however, is its
pability to respond to a broad repertoire of onists that are not necessarily microbial in o
gin, but rather are endogenous signals. NLRhas been suggested to respond to changes
cellular ion concentrations, particularly potsium, that are produced, for example, by
marine toxin maitotoxin and the K+/H+
tiport ionophore nigericin (46). NLRP3 actition is also observed with uric acid crystals (
and reactive oxygen species that are generain response to, for example, asbestos and sil
(7).Significant insight into the mechanism
which NLRP3 recognizes its various ligacame from the observation that the addition
ATP to macrophages prestimulated with bterial molecules such as LPS can significan
enhance caspase-1 activation and IL-1 p
duction. Identifying the role of ATP in NLRactivation has been controversial, as high no
physiological concentrations of ATP are tycally required for enhanced IL-1 producti
An important function of ATP is the stimlation of the P2X7 receptor, which, in tu
results in the opening of a pore mediatedthe hemichannel protein pannexin-1 (96, 9
Therefore, a consequence of ATP additionthe ability of bacterial products to enter the
tosol through the pore and to subsequently tivate NLRP3 and caspase-1. Indeed, with
addition of ATP, several bacterial product
including LPS, PGN, and lipoteichoic acas well as heat-killed bacteriacan activ
caspase-1inanNLRP3-dependent(butaTLand RICK-independent) manner (44, 45,
98). Moreover, the requirement for ATP canbypassed when other methods of cytosolic
livery are implemented; such methods inclu
378 Chen et al.
-
8/6/2019 Annurev.pathol NOD
15/36
the use of pore-forming bacterial toxins (e.g.,
streptolysin O) or the lipophilic DOTAP deliv-
ery system (98, 99). However, not all bacterialpathogens that can invade the cytosol require
NLRP3 for caspase-1 activation as Salmonellaand Francisellawhich are capable of deliver-
ing bacterial products into the cytosol throughtype III secretion systems (TTSS) or through
pore-forming molecules without ATPcanactivate caspase-1 independently of NLRP3
(98). Thus, NLRP3 recognition of PAMPs ap-pears to be linked to pannexin-1-dependent
pore formation. MDP, a NOD2 agonist, hasalso been shown to activate NLRP3 (100) so
as to activate caspase-1. This activation is in-
dependent of NOD2 and involves the internal-ization of MDP into acidified vesicles that are
released into the cytosol upon addition of ATPin a pannexin-1-dependent manner (101).
An increasingly recognized consequence ofactivation of the P2X7 receptor and pannexin-
1 by ATP is the alteration in potassiumconcentrations in the cell (i.e., intracellular
potassium depletion), which has been sug-gested to be important for NLRP3 but not
for NLRC4 signaling (102, 103). Treatmentof macrophages with the pore-forming tox-
ins nigericin and maitotoxin is also associ-
ated with intracellular potassium depletionand results in NLRP3-induced activation
of caspase-1 (46). Therefore, in additionto facilitating entry of NRLP3-responsive
PAMPs, pore-forming toxins also promotechanges in intracellular potassium concen-
trations that may be required for NLRP3activation. However, the concentration of
potassium itself may not regulate caspase-1 ac-tivation, as changes in potassium concentration
in the cell are associated with other ionic fluxesor cellular events that may be critically involved
in NLRP3 signaling. Moreover, in the absence
of PAMP prestimulation, ATP does not acti-vate caspase-1, even though it alone can trigger
potent efflux of intracellular potassium (102).Thus, the true significance of potassium con-
centration changes associated with NLR sig-naling remains to be fully elucidated. However,
one can interpret changes in cellular potassium
concentrations associated with pore formation,
uric acid release, and ATP generation as surro-gate indicators of cellular stress or injury; there-
fore, NLRP3 andperhaps other NLRs mayalso
function to recognize and respond to endoge-nous danger signals besides microbial infection
(95, 104).
MECHANISMS OFINTRACELLULAR DELIVERYOF MICROBIAL PRODUCTSFOR DETECTION BY
NOD-LIKE RECEPTORS
A defining feature of the NLRs is their in-
tracellular localization. With the exception ofNLXR1, which has been shown to be im-
portant within the mitochondria (6, 7), andCIITA, which resides in part in the nucleus,
all NLRs characterized to date are locatedwithin the cytoplasm. This raises the question
of how these receptors recognize pathogens,or how pathogens are delivered into the intra-
cellular compartment. Based on their cytoso-lic localization, NLRs may respond primarily
to (a) bacteria that escape extracellular detec-tion by the TLRs and invade directly into the
cell, (b) bacterial components that are deliv-
ered into the cytosol through secretion sys-tems or through pore-forming molecules, or
(c)bacterialproductsthatareuptakenbytheim-mune cell through phagocytosis or pinocytosis
(Figure 3). Consistent with the first possibil-ity, NOD1 activation depends upon the intra-
cellular localization of directly invasive bacteriasuch as S. flexneri(9, 64, 105) and S. pneumoniae(72). Also, only live and not paraformaldehyde-fixed C. jejunielicit NOD1-dependent NF-B
activation (36).Bacteria with active secretion systems pro-
vide an additional mechanism for intracellu-
lar entry that is important for NLR recog-nition. Two secretion systems, type III and
type IV, are involved in the injection of viru-lence proteins into the host cell to stimulate
NLR signaling. These secretion systems arefound in gram-negative bacteria and are en-
coded within regions of the bacterial genome
www.annualreviews.org NLRs: Role in Immunity and Disease 379
-
8/6/2019 Annurev.pathol NOD
16/36
P2X7R
ATPPannexin-1a
-BNF
NLRinflammasome
Pore-formingtoxin
Pro-IL-1
Nucleus
IL-1
Caspase-1
Phagosome
Bacteria type III or IVsecretion system
P2X7R
PAMPs
Figure 3
Modes of intracellular entry of microbes for Nod-like receptor (NLR)activation. Microbes and microbial molecules enter the cytosol viapore-forming toxins, type III or IV secretion systems, or ATP-mediatedactivation of the pannexin-1 pore. Sensing of microbial molecules in the cytosolby several NLRs results in the formation of inflammasomes. The mechanismwhereby NLRs recognize microbial molecules appears indirect and remainspoorly understood. Activation of caspase-1 induces processing of the
interleukin-1-beta (IL-1) precursor and secretion of the mature cytokine.Abbreviation: PAMPs, pathogen-associated molecular patterns.
known as pathogenicity islands. These secre-tion systems allow NLR detection by non-
phagocytosing cells such as epithelial cells. ForTTSS, the mechanism by which gram-negative
bacteria invade the cell is well illustrated by
Salmonella (106). Two important features of
Salmonella pathogenesis are (a) the bacterias
ability to invade nonphagocytic cells such asintestinal epithelial cells and (b) their ability
to survive as well as replicate within phago-cytes. Both of these features depend upon
intact TTSS. TTSS consists of a complexassembly of proteins that form transporter ap-
paratuses; these contain approximately 20 pro-tein subunits for the trafficking of bacterial
proteins involved in bacterial virulence. As
scribed above, the delivery of flagellin to tcytosol for NLRC4 inflammasome activat
has been proposed to occur via TTSS, a
Salmonella mutants with nonfunctional TTare unable to activate NLRC4 in macropha
(50).InthecaseofLegionella, TFSSis essential
the survival of the pathogen within the phagsome. In a not-fully-understood mechanis
Legionellaonce phagocytosed by the APsuch as the macrophagereplicates within
phagosome and avoids fusion with the lysome through secretion of virulence prote
by the TFSS, which causes pore formati
Legionella is recognized by NLRC4 most lik
as a result of translocation of bacterial liga
(flagellin) through the TFSS into the cyto(107). As with Legionella, delivery of PG
derived molecules into the cytosol by H. pyforNOD1signalingrequiresanintactTFSS
sociated with the cag pathogenicity island, a
H. pyloristrains that lackcaghave reduced lev
of NF-B activation (66).Bacterial secretion systems also ena
pathogens to form pores to escape phasomes after phagocytosis, as well as
transport bacterial products. For example, pore-forming toxin listeriolysin produced
Listeria permits the delivery of PGN tha
recognizable by NOD1 and NOD2 (12, 108). Other bacteria that secrete pore-form
toxins, such as S. pneumoniae, which produpneumolysin, and B. anthraciswith anthroly
O, can also allow internalization of PGN frments for recognition by NLRs, especially
nonphagocytosing cells such as epithelial c(109).
With certain bacteria, activation of NLcan occur with heat-killed bacteria alone, su
gesting that neither an active secretion stem nor direct invasion is required for reco
nition. In these cases, dead bacteria are lik
directly uptaken into the cell by phagocyto(73). For example, inhibition of macropha
phagocytosis of heat-killed S. aureusresulteddecreased inflammatory cytokine producti
which was partly dependent on both NO
380 Chen et al.
-
8/6/2019 Annurev.pathol NOD
17/36
and NOD2 (76). The entry of MDP has also
been proposed to occur in intestinal epithe-
lial cells through a host-dependent rather thanbacterial-dependent mechanism, in which the
active peptide transporter hPepT1 transportsMDP in vitro (110).
NOD-LIKE RECEPTORSIGNALING SYNERGIZES ANDCOMPLEMENTS TOLL-LIKERECEPTOR SIGNALING
There is great overlap and an apparent redun-dancy in the natureof thepathogensrecognized
by the various NLRs and TLRs, and many of
the receptors converge to common pathways(e.g., NF-B and IL-1 activation). An obvi-
ous reason for the existence of multiple recep-tors channeling into common end targets is
the potentiation of the inflammatory responseto infection. This is consistent with the syn-
ergy observed with TLR and NLR signalingin response to PGN (74, 111, 112) and be-
tween TLR and NOD2 agonists (33). In addi-tion, a segregation of function between NLRs
and TLRs is naturally imposed by their cellu-lar localization, such that NLRs may acquire
greater importance in the detection of intracel-
lularly located bacteria. Regardless, NLRs andTLRs also play nonredundant roles, as is re-
flected in the observations of TLR- and NLR-specific transcriptomes associated with Listeria
infection andof synergistic activation of NF-B(113).
Additional evidence for complementaryroles of NLRs and TLRs in the inflamma-
tory response has been demonstrated with IL-1 secretion (see Figure 4a). The release
of IL-1 involves two distinct steps: (a) in-duction of pro-IL-1, which is NF-B de-
pendent, and (b) cleavage of pro-IL-1 by
caspase-1 to the mature, active IL-1. The firststep requires TLR activation of NF-B (98);
however, activation of caspase-1 occurs inde-pendently of TLRs and requires the inflam-
masome (98). This two-part pathway, differen-tially regulated by TLRs and NLRs, may serve
as a safeguard against excessive production of
IL-1, which can cause pathology (see In-flammatory Diseases Associated with Excessive
Interleukin-1 Production, below). Similarly,
multiple NLRs or TLRs may recognize simi-lar stimuli but regulate different aspects of the
same process. Using the same example of reg-ulation of IL-1 production, caspase-1 activa-
tion by MDP stimulation requires NLRP3 andATP but not NOD2; however, the induction
of IL-1 messenger RNA, on the other hand,requires NOD2 but not NLRP3 (101). There-
fore, similar to therequirement for TLRsignal-ing to promote pro-IL-1 production through
NF-B,inthecaseofIL-1 induction by MDP,NOD2 mediates the transcription of pro-IL-
1byNF-B, whereas NLRP3 mediates IL-1
processing through caspase-1 activation. Also,as described above, studies have suggested that
Legionella recognition by both NLRC4 andNaip5 can result in alternate activities to re-
strict intracellular replication ofLegionella andthat recognition of flagellin in either Legionella
or Salmonella by TLR5 and NLRC4 can resultin the activation of separate pathways, NF-B
and caspase-1 activation, respectively (4850,89, 114). Thus, the multiplicity of receptors in-
volved in the recognition of the same ligandallows not only multiple levels of control to
prevent excessive production of cytokines (e.g.,IL-1) that can harm the host, but it also pro-
motes a concerted response against infection
through the activation of separate, but coop-erative pathways.
In addition to having a synergistic effect with TLR signaling, NLRs may provide the
host with a backup defense mechanism thatmay be required under conditions when TLR
signaling has been tolerized (Figure 4b). Awell-recognized phenomenon associated with
TLR signaling is the induction of tolerance: After an initial LPS exposure to, for exam-
ple, macrophages, cytokine responses are sup-pressed upon secondary exposure to LPS.
Possible physiologic explanations for this phe-
nomenon are (a) to prevent excessive cytokineproduction by bacterial stimuli, which can lead
www.annualreviews.org NLRs: Role in Immunity and Disease 381
-
8/6/2019 Annurev.pathol NOD
18/36
TLRs
NF-B
Pro-IL-1 IL-1
Caspase-1
NLRinflammasome
TLRs
Invasion ofintracellular bacteria
TLR activation
Reduced TLR signaling (tolerance)(prevent overproduction of proinflammatory cytokine)
+Enhanced NLR signaling
Prepare to fight invasive pathogen
a b
Figure 4
The cooperative interplay between Toll-like receptors (TLRs) and Nod-like receptors (NLRs) in response to intracellular bacteria.(a) Stimulation of TLRs or NOD1/NOD2 induces the production of pro-interleukin-1-beta (pro-IL-1) through the activation ofnuclear factorkappa B (NF-B) signaling, leading to transcription of the IL-1 gene. In contrast, the presence of microbial molecuin the cytosol is sensed by the NLRs, resulting in inflammasome formation and caspase-1 activation. Activated caspase-1 cleavespro-IL-1 and results in secretion of mature IL-1. (b) Intracellular bacteria such as Listeria are recognized by TLRs, leading to TLactivation and production of proinflammatory and antimicrobial molecules. Persistent TLR stimulation leads to TLR tolerization anto reduced TLR signaling. Cytosolic invasion of the bacteria activates NLRs (e.g., NOD1/NOD2 and inflammasome-inducing NLR
resulting in enhanced NLR signaling and in production of antimicrobial molecules.
to the clinical syndrome of sepsis and to mul-tiorgan failure in the host, and (b) to stymie
an excessive immune response against com-mensal bacteria, which can lead to patholog-
ical inflammation. Although theoretically this
is a good safeguard mechanism, a potenrisk in the development of hyporesponsiven
with serial LPS challenge in APCs is an creased susceptibility to bacterial superinf
tion (115). Because TLR-induced tolerizat
382 Chen et al.
-
8/6/2019 Annurev.pathol NOD
19/36
is limited to TLR agonists that act in the
same pathway, NLRs may play a protective role
against bacterial infection in the TLR-tolerizedstate (Figure 4b) (77). Indeed, it has recently
been shown that cross-tolerization does not oc-cur with the combination of the NLR ago-
nist MDP and the TLR agonist LPS, as pres-timulation with either LPS or MDP does not
abrogate cytokine responses to MDP or LPS,respectively (77). Rather, enhancement in NF-B and MAPK activation as well as in cytokineproduction occurred after stimulation of MDP
in macrophages made refractory to TLR lig-ands, and vice versa (77).
A functional consequence of this phe-
nomenon is the heightened importance ofNOD1 and NOD2 response to intracellular
bacterial infection in macrophages tolerizedto previous exposure with TLR agonists (77).
Consistently, it was demonstrated that afterprevious exposure to E. colior LPS, response to
subsequent infection with Listeria was greatlycompromised in the absence of NOD1 and
NOD2 signaling both in vitro and in vivo (77).Similarly, in the case of Salmonella infection,
TLR-tolerant macrophages were still capableofIL-1productionthrough NLRC4signaling
(49). Thus, NLR signaling can potentiate TLR
signaling and can provide additional protectionto the host against bacterial invasion. One im-
plicationfor this model is that immune cells canremain sensitive to infection by pathogenic bac-
teria through NLR signaling in cells that havebecome tolerized to TLR ligands, such as com-
mensal bacteria in the gut.Note, however, that several groups (116
118) have also shownboth in humans andin micethat cross-tolerization still does oc-
cur with stimulation of immune cells by NLRagonists followed by TLR agonists. This dis-
crepancy may be due in part to differences inexperimental methods, including the timing of
pretreatment (early versus late second expo-
sure) or cell type (macrophages versus den-dritic cells), and it suggests that the regulation
of tolerization and synergy between NLR andTLRs may be specific to both context and cell
type.
IBD: inflammatorybowel disease
UC: ulcerative colit
CD: Crohns diseas
DYSREGULATED NOD-LIKERECEPTOR SIGNALING ISINVOLVED IN THEPATHOGENESIS OF MULTIPLEHUMAN DISEASES
The physiologic significance of the variousNLRs lies primarily in their roles in host de-
fense against microbial infection. However, itis becoming increasingly clear that NLRs alsofunction in organ homeostasis, which is un-
derscored by the fact that many inflammatoryand noninflammatory disease processes can
be attributed to dysregulated NLR signaling(Figure 5). The following subsections de-
scribe certain defined NLR roles in humandiseases.
Inflammatory Bowel Disease
The role of NLRs in intestinal homeostasis was
highlighted by the observations of mutationsin NOD2 that are associated with the devel-
opment of inflammatory bowel disease (IBD).IBD encompasses two different diseases, ulcer-
ative colitis (UC) and Crohns disease (CD);these diseases cause inflammation of the intes-
tine, leading to the common clinical presenta-
tion of abdominal pain, bloody diarrhea, andweight loss. Despite their similar clinical symp-
toms, UC and CD have distinguishing clinicaland histologic features. In UC, inflammation is
limited to the mucosal layer of the colon, mostcommonly therectum. In CD,however, inflam-
mation is transmural and can involve any part ofthe gastrointestinal tract. Because of the trans-
mural inflammation in CD, complications nottypically seen in UC can occur; these include
bowel-wall perforation and fistula formation.CD also differs from UC with regard to the af-
fected areas of the bowel: CD most commonly
involves the lower part of the small intestine,the terminal ileum.
The underlying pathogenesis of IBD is un-clear, but studies suggest that both environ-
mental and genetic factors contribute to theetiology of CD. Genetic linkage analyses of
affected families have identified eight genetic
www.annualreviews.org NLRs: Role in Immunity and Disease 383
-
8/6/2019 Annurev.pathol NOD
20/36
Blau syndrome/early-onsetsarcoidosis
NOD2(skin, eyes, joints)
Cryopyrinopathies
(MWS, FCAS, NOMID)NLRP3
(skin, eyes, joints)
Asthma
NOD1
(lungs)
Barelymphocyte
syndrome
CTIIA(lymphocytes)
Inflammatory bowel disease
NOD2, NOD1?(intestine)
Sarcoidosis
NOD1(lungs)
Vitiligo
NLRP1(skin)
Gain-of-functionmutations
Loss-of-functionmutations
Figure 5
Genetic variation in Nod-like receptors (NLRs) is associated with development of human disease.Gain-of-function point mutations within the NOD domains ofNLRP3 and NOD2 cause autoinflammatodisorders: The former cause Muckle-Wells syndrome (MWS), familial cold autoinflammatory syndrome
(FCAS), and neonatal-onset multisystem inflammatory disease (NOMID), and the latter cause Blausyndrome/early-onset sarcoidosis. Consistently, the latter diseases are inherited in a Mendelian-dominantfashion. In contrast, loss-of-function mutations ofNOD1, NOD2, and CTIIA are associated with thedevelopment of asthma, adult sarcoidosis, bare lymphocyte syndrome, and Crohns disease. Genetic variatin NLRP1 is associated with vitiligo. The type of functional alteration of the disease-associated NLRP1alleles remains to be determined.
loci(IBD1IBD8) containingCD-susceptibility
genes (119). The risk allele for IBD1 has beenidentified as NOD2 by genetic and functional
studies (120, 121). Although multiple variantsof NOD2 have been found to be associated
with CD, approximately 40% of CD patientsof North American or Western European de-
scent carry at least one of the three major
disease-associated variants: G908R, R702W,and a frame-shift deletion mutation at L1007
(L1007fsinsC). Patients homozygous for thesemutations have a 20- to 40-fold increased risk
for disease development, whereas heterozyg
subjects have only a two- to fourfold increarisk (120, 121). These CD-associated NO
variants exhibit reduced capacity to activNF-B following MDP stimulation (61), co
sistent with the finding that these mutationsnear or within the LRR domain of NOD2. T
impaired sensing of PGN and/or MDP sugests that these CD-associated mutations res
in a loss-of-function phenotype. Furthermo
monocytes isolated from CD patients harbing the L1007fsins mutation exhibit reduc
384 Chen et al.
-
8/6/2019 Annurev.pathol NOD
21/36
3
34
4
Reduced NOD2-dependentexpression of bactericidal-defensins in Paneth cells
Impaired recognition andclearance of bacteria byintestinal phagocytes
Dysregulation of TLR2-mediatedinflammation in intestinalmacrophages and/or dendritic cells
Enhanced production of IL-1
Macrophage
Nod2
IL-1
Nod2
Proinflammatorycytokines
TLR2
4
innflflaaammmmmmaammmmaaaccrrooopphphh
EEnEnnnhhhaaanncncced
11LL
-defensins
Paneth cellsNod2
4 ILIh
1-1L-L4 LIL
222R2R2TLRRRTLR
Dendritic cell
1
1
2
2
Figure 6
Proposed models for the role of NOD2 in Crohns disease. Shown are four nonexclusive models of the contribution of mutant NODalleles to Crohns disease. In the first two models, impaired NOD2 function is associated with either increased invasion of intestinalbacteria by deficient production of-defensins (1) or reduced clearance of bacteria by intestinal phagocytes, leading to inappropriateactivation of NOD2-independent pathogen-recognition receptor (PRR)-signaling pathways (2). In the third model, NOD2 acts as abrake of commensal bacteriadriven inflammation, and the presence of deficient NOD2 alleles results in enhanced Toll-like receptor(TLR)-induced activation (3). In the fourth model, which is based on a mouse Nod2-knockin model, Crohns diseaseassociated NODmutations function as gain-of-function alleles, resulting in inappropriate interleukin-1-beta (IL-1) production (4).
production of proinflammatory cytokines such
as TNF-, IL-6, and IL-8, as well as the anti-inflammatory cytokine IL-10 (122, 123). How-
ever, the loss of NF-B inducibility by the CD-associated NOD2 variants is inconsistent with
the occurrence of increased NF-B-dependentinflammation observed in clinical samples iso-
lated from CD patients. In order to reconcilethese observations and provide a mechanistic
explanation, two broad hypotheses regardingthe role of NOD2 in the pathogenesis of CD
have been advanced (Figure 6). The first hy-pothesisisthatmutationsinNOD2resultinde-
ficiencies in epithelial-barrier function and/orin immune cells required for limiting bacterial
invasion or clearance, which subsequently leads
to increased inflammation at intestinal sites.The second contends that primary dysregula-
tion of the mucosal immune system leads to ex-
cessive activation of proinflammatory signalingpathways.
Evidence for a role for NOD2 in regulatingepithelial-barrier function comes from trans-
fection experiments demonstrating that wild-type (but not mutant) NOD2 can restrict pro-
liferation of Salmonella in intestinal epithelialcells (75). The ability of NOD2 to restrict in-
vasive bacterial growth may be related to itsability to activate NF-B-dependent produc-
tion of the -defensins by Paneth cells, whichare specialized epithelial cells located in the
crypts of the ileal mucosa. Consistent with this
www.annualreviews.org NLRs: Role in Immunity and Disease 385
-
8/6/2019 Annurev.pathol NOD
22/36
hypothesis is the observation that NOD2 is ex-
pressedconstitutively in Paneth cells (124, 125).
In addition, CD patients with mutant NOD2have reduced expression of two -defensins
in the ileal mucosa, human -defensin-5 and-defensin-6 (31). Furthermore, mice genet-
ically deficient for Nod2 displayed impairedprotection against oral, but not intravenous or
intraperitoneal, administration of L. monocyto-
genes. The increased susceptibility of Nod2-
deficient mice was correlated with diminishedexpression of Panethcellderived antimicrobial
peptides, Defcr4 and Defcr-rs10 (33). Thus,impaired production of-defensins in Paneth
cells due to NOD2 mutations, which results
in a compromise in barrier function, might bea plausible link between NOD2 and suscepti-
bility to CD. However, the observation of de-creased -defensins should be interpreted with
caution, as this may merely reflect Paneth cellloss from inflamed, damaged epithelium (126).
Another possibility is that NOD2 mutationsresult in impaired clearance of locally inva-
sive bacteria due to defective recognition byintestinal phagocytes. This alternative loss-of-
function hypothesis is consistent with observa-tions of impaired production of antimicrobial
molecules and of IL-1, induced by MDP in
monocytes, expressing CD-associated NOD2mutations (61, 123). The defective removal of
intestinal bacteria may drive inflammation viaactivation of NOD2-independent PRRs, in-
cluding NOD1 and TLRs.The second hypothesis regarding the patho-
genesis of CD contends that the disease re-sults from inappropriate hyperresponsiveness
to commensal bacteria in the normal intestinemicroflora (127). This hyperreactive hypoth-
esis is supported by evidence demonstratingthat (a) NOD2 functions as a negative regu-
lator of IL-12 production mediated by PGNthroughTLR2and(b)intheabsenceofNOD2-
mediated regulation, PGN elicits a heightened
NF-B-dependent IL-12 or IL-23 responseby intestinal APCs, thereby promoting an ex-
uberant adaptive Th1 or Th17 type of im-mune response often observed in CD patients
(128, 129). In this model, it is assumed that in
normal intestine, APCs are constantly expo
to commensal bacteriaderived PGN withany overt immune response. It is then pos
lated that in normal individuals, NOD2 futions as a brake, dampening any potential
nate immune response to PGN. In contr
PGN-mediated immune responses in indivuals with NOD2 mutations are refractory
NOD2 modulation, thus resulting in high lels of IL-12/IL-23 andcreating an environm
capable of generating a pathological Th1/Thimmune response. Consistent with the ideat
dysregulated IL-12 promotes colitis, treatmof CD patients with antibody against IL-12
been shown to be effective (130). Alternativedata derived from the analysis of knockin m
expressing Nod2, which mimics L1007fsinsuggest that macrophages from these knoc
mice had increased levels of IL-1 product
(131). In addition to increased cytokine prodtion, theseknockin mice were shown to be m
susceptible to dextran sodium sulfateinduccolitis, suggesting that the frame-shiftmutat
associated with CD is a gain-of-function mtation. However, unlike the published knoc
Nod2 mouse model, monocytes from healtor CD patients homozygous for NOD2 mu
tions exhibit loss-of-function phenotypes (123). Thus, the relevance of the knoc
Nod2 mouse model remains uncertain.The hpotheses presented here may not be mutua
exclusive; further, they suggest that NOD2 m
contribute to CD development via multimechanisms.
Due to the similarity in signaling and struture between NOD1 and NOD2, research
are interested in determining whether NOis also associated with susceptibility to IB
Studies have been conflicting and may be poulation dependent; however, two studies h
demonstrated an association of NOD1 wIBD (132, 133). The first study to identify an
sociation between NOD1 polymorphisms aIBD involved two independent cohorts co
prising over 1000 IBD patients in England
these patients the common deletion allelea complex polymorphism (ND1+326561) w
significantly associated with IBD and wit
386 Chen et al.
-
8/6/2019 Annurev.pathol NOD
23/36
-
8/6/2019 Annurev.pathol NOD
24/36
-
8/6/2019 Annurev.pathol NOD
25/36
such as BS, researchers have attempted
to determine whether NOD2 variants are
also associated with disease susceptibility forsarcoid. However, unlike with NOD1, no
correlation between NOD2 mutations and sar-coid has been observed (162164). Interest-
ingly, however, NOD2 has been associated with juvenile-onset sarcoid (EOS). This disease is
distinct from adult sarcoidosis in that it usuallyis seen in individuals younger than four years
with the clinical triad of skin, joint, and eyeinvolvementsimilar to that seen in BS, but
lacking pulmonary findings. In a small studyof 10 Japanese patients diagnosed with EOS,
nine had heterozygous missense mutations in
the NOD domain of NOD2, totaling six dif-ferent variants (165). Only one variant was
identical to that reported with Blau syndrome,while the remaining five were novel. Regard-
less, EOS-associated NOD2 variants, like theirBS-associated NOD2 counterparts, exhibited
increased basal NF-B activity compared towild type that was further enhanced with the
addition of MDP in a reporter assay in vitro(165).
Allergic diseases. Allergies are associated
with hyperreactivity to antigens; they are char-acterized by increased immunoglobin E re-
sponse and are therefore inflammatory innature. Certain NOD1 genetic variants are
associated with an increased risk of develop-ing asthma and atopic eczema, and therefore
NOD1 may play a role in the modulation of amucosal allergic response (166, 167). Because
asthma results from gene-environment inter-actions, its association with NOD1 may impli-
cate bacterial signaling through NOD1 in thepathogenesis of asthma. This would be consis-
tent with the prevailing hygiene hypothesis
of asthma risk: Studies have demonstrated thatindividuals with reduced exposure to bacteria
during childhood have an increased risk of de-veloping asthma (168170). Moreover, NOD1
polymorphisms can also modify the protectiveeffect of early exposure to allergens (171), pro-
vidingadditional evidence for a possible role for
NOD1 in modulating the response to environ-
mental bacteria and development of asthma.
Cancer. Recent studies have suggested thatTLR signaling plays an important role in car-
cinogenesis, especially within the gastrointesti-
nal tract (172, 173). A role for NLRs has not yetbeen investigated; however, a tumor-suppressor
function in NOD1 has been suggested in breastcancer xenograft models (174). This phenotype
was attributed to a functional role for NOD1in regulating apoptosis, in which retrovirally
infected MCF-7 cells with defective NOD1expression were more sensitive to TNF--
induced apoptosis in vitro in the presence ofcyclohexamide, which facilitates apoptosis by
inhibiting expression of antiapoptotic factors.In vivo, this mutant cell line also showed in-
creased growth potential as xenografts; this po-
tential was not associated with decreased apop-tosis, but rather with a lack of responsiveness
to estrogen-induced proliferation, suggestingan additional role for NOD1 in regulating es-
trogen receptor expression. However, sponta-neous growth of tumors has not been observed
in Nod1-deficient mice, and whether NOD1influences tumor growth in other organs that
are not necessarilyhormone responsive remainsto be determined.
CONCLUSIONS ANDPERSPECTIVES
The identification and initial characterization
of NLR proteins have yielded new insights intothe host recognition system involved in micro-
bial detection and host-defense mechanisms.The involvement of NLRs in the pathogenesis
of several genetic diseases indicates that theseproteins play an important role in the regula-
tion of immune and inflammatory responses.
There is conclusive evidence that several NLRssense conserved microbial molecules to activate
discrete signaling pathways including NF-B,MAPK, and caspase-1 activation. There is also
clear evidence for interplay between NLRs andTLRs in the regulation of the inflammatory re-
sponse against microbes.
www.annualreviews.org NLRs: Role in Immunity and Disease 389
-
8/6/2019 Annurev.pathol NOD
26/36
-
8/6/2019 Annurev.pathol NOD
27/36
-
8/6/2019 Annurev.pathol NOD
28/36
-
8/6/2019 Annurev.pathol NOD
29/36
44. Kanneganti TD, Body-Malapel M, Amer A, Park JH, Whitfield J, et al. 2006. Critical role for
Cryopyrin/Nalp3 in activation of caspase-1 in response to viral infection and double-stranded RNA.
J. Biol. Chem. 281:3656068
45. Sutterwala FS, Ogura Y, Szczepanik M, Lara-Tejero M, Lichtenberger GS, et al. 2006. Critical role
for NALP3/CIAS1/Cryopyrin in innate and adaptive immunity through its regulation of caspase-1.
Immunity 24:31727
46. Mariathasan S, Weiss DS, Newton K, McBride J, ORourke K, et al. 2006. Cryopyrin activates the
inflammasome in response to toxins and ATP. Nature 440:22832
47. Mariathasan S, Newton K, Monack DM, Vucic D, French DM, et al. 2004. Differential activation of theinflammasome by caspase-1 adaptors ASC and Ipaf. Nature 430:21318
48. Amer A, Franchi L, Kanneganti TD, Body-Malapel M, Ozoren N, et al. 2006. Regulation ofLegionella
phagosome maturation and infection through flagellin and host Ipaf. J. Biol. Chem. 281:3521723
49. Franchi L, Amer A, Body-MalapelM, Kanneganti TD,Ozoren N, et al.2006. Cytosolic flagellin requires
Ipaf for activation of caspase-1 and interleukin 1 in salmonella-infected macrophages. Nat. Immunol.
7:57682
50. Miao EA, Alpuche-Aranda CM, Dors M, Clark AE, Bader MW, et al. 2006. Cytoplasmic flagellin
activates caspase-1 and secretion of interleukin 1 via Ipaf. Nat. Immunol. 7:56975
51. Fink SL, Cookson BT. 2007. Pyroptosis and host cell death responses during Salmonella infection. Cell
Microbiol. 9:256270
52. Fink SL, Bergsbaken T, Cookson BT. 2008. Anthrax lethal toxin and Salmonella elicit the common cell
death pathway of caspase-1-dependent pyroptosis via distinct mechanisms. Proc. Natl. Acad. Sci. USA105:431217
53. Sansonetti PJ, Phalipon A, Arondel J, Thirumalai K, Banerjee S, et al. 2000. Caspase-1 activation of
IL-1 and IL-18 are essential for Shigella flexneriinduced inflammation. Immunity 12:58190
54. Mariathasan S, Weiss DS, Dixit VM, Monack DM. 2005. Innate immunity against Francisella tularensis
is dependent on the ASC/caspase-1 axis. J. Exp. Med. 202:104349
55. Tsuji NM, Tsutsui H, Seki E, Kuida K, Okamura H, et al. 2004. Roles of caspase-1 in Listeria infection
in mice. Int. Immunol. 16:33543
56. Bergsbaken T, Cookson BT. 2007. Macrophage activation redirects Yersinia-infected host cell death
from apoptosis to caspase-1-dependent pyroptosis. PLoS Pathog. 3:e161
57. Inohara N, Ogura Y, Chen FF, Muto A, Nunez G. 2001. Human Nod1 confers responsiveness to
bacterial lipopolysaccharides. J. Biol. Chem. 276:255154
58. Hasegawa M, Yang K, Hashimoto M, Park JH, Kim YG, et al. 2006. Differential release and distributionof Nod1 and Nod2 immunostimulatory molecules among bacterial species and environments. J. Biol.
Chem. 281:2905463
59. Girardin SE, Boneca IG, Carneiro LA, Antignac A, Jehanno M, et al. 2003. Nod1 detects a unique
muropeptide from gram-negative bacterial peptidoglycan. Science 300:158487
60. Chamaillard M, Hashimoto M, Horie Y, Masumoto J, Qiu S, et al. 2003. An essential role for NOD1 in
host recognition of bacterial peptidoglycan containing diaminopimelic acid. Nat. Immunol. 4:7027
61. Inohara N, Ogura Y, Fontalba A, Gutierrez O, Pons F, et al. 2003. Host recognition of bacterial muramyl
dipeptide mediated through NOD2. Implications for Crohns disease. J. Biol. Chem. 278:550912
62. McDonald C, Inohara N, Nunez G. 2005. Peptidoglycan signaling in innateimmunityand inflammatory
disease. J. Biol. Chem. 280:2017780
63. Hasegawa M, Kawasaki A, Yang K, Fujimoto Y, Masumoto J, et al. 2007. A role of lipophilic
peptidoglycanrelated molecules in induction of Nod1-mediated immune responses. J. Biol. Chem.282:1175764
64. Nigro G, Fazio LL, Martino MC, Rossi G, Tattoli I, et al. 2008. Muramylpeptide shedding modulates
cell sensing ofShigella flexneri. Cell Microbiol. 10:68295
65. Kufer TA, Kremmer E, Adam AC, Philpott DJ, Sansonetti PJ. 2008. The pattern-recognition molecule
Nod1 is localized at the plasma membrane at sites of bacterial interaction. Cell Microbiol. 10:47786
66. Viala J, Chaput C, Boneca IG, Cardona A, Girardin SE, et al. 2004. Nod1 responds to peptidoglycan
delivered by the Helicobacter pyloricag pathogenicity island. Nat. Immunol. 5:116674
www.annualreviews.org NLRs: Role in Immunity and Disease 393
-
8/6/2019 Annurev.pathol NOD
30/36
67. Zilbauer M, Dorrell N, Boughan PK, Harris A, Wren BW, et al. 2005. Intestinal innate immun
to Campylobacter jejuni results in induction of bactericidal human -defensins 2 and 3. Infect. Imm
73:728189
68. Kim JG, Lee SJ, Kagnoff MF. 2004. Nod1 is an essential signal transducer in intestinal epithelial c
infected with bacteria that avoid recognition by toll-like receptors. Infect. Immun. 72:148795
69. Opitz B, Forster S, Hocke AC, Maass M, Schmeck B, et al. 2005. Nod1-mediated endothelial c
activation byChlamydophila pneumoniae. Circ. Res. 96:31926
70. Travassos LH, Carneiro LA, Girardin SE, Boneca IG, Lemos R, et al. 2005. Nod1 participates in
innate immune response to Pseudomonas aeruginosa. J. Biol. Chem. 280:367141871. Welter-Stahl L, Ojcius DM, Viala J, Girardin S, Liu W, et al. 2006. Stimulation of the cytosolic recep
for peptidoglycan, Nod1, by infection with Chlamydia trachomatisor Chlamydia muridarum. Cell Micro
8:104757
72. Opitz B, Puschel A, Schmeck B, Hocke AC, Rosseau S, et al. 2004. Nucleotide-binding oligomerizat
domain proteins are innate immune receptors for internalized Streptococcus pneumoniae. J. Biol. Ch
279:3642632
73. Herskovits AA, Auerbuch V, Portnoy DA. 2007. Bacterial ligands generated in a phagosome are targ
of the cytosolic innate immune system. PLoS Pathog. 3:e51
74. Ferwerda G, Girardin SE, Kullberg BJ, Le Bourhis L, de Jong DJ, et al. 2005. NOD2 and toll-l
receptors are nonredundant recognition systems ofMycobacterium tuberculosis. PLoS Pathog. 1:2798
75. Hisamatsu T, Suzuki M, Reinecker HC, Nadeau WJ, McCormick BA, et al. 2003. CARD15/NO
functions as an antibacterial factor in human intestinal epithelial cells. Gastroenterology 124:99310076. Kapetanovic R, Nahori MA, Balloy V, Fitting C, Philpott DJ, et al. 2007. Contribution of phagocyt
and intracellular sensing for cytokine production byStaphylococcus aureusactivated macrophages. Inf
Immun. 75:83037
77. Kim YG, Park JH, Shaw MH, Franchi L, Inohara N, et al. 2008. The cytosolic sensors Nod1 a
Nod2 are critical for bacterial recognition and host defense after exposure to Toll-like receptor ligan
Immunity 28:24657
78. Abreu MT, Thomas LS, Arnold ET, Lukasek K, Michelsen KS, et al. 2003. TLR signaling at t
intestinal epithelial interface. J. Endotoxin Res. 9:32230
79. Melmed G, Thomas LS, Lee N, Tesfay SY, Lukasek K, et al. 2003. Human intestinal epithelial cells
broadly unresponsive to Toll-like receptor 2dependent bacterial ligands: implications for host-micro
interactions in the gut. J. Immunol. 170:140615
80. Warren SE, Mao DP, Rodriguez AE, Miao EA, Aderem A. 2008. Multiple Nod-like receptors activcaspase-1 during Listeria monocytogenesinfection. J. Immunol. 180:755864
81. Molofsky AB, Byrne BG, Whitfield NN, Madigan CA, Fuse ET, et al. 2006. Cytosolic recognition
flagellin by mouse macrophages restricts Legionella pneumophila infection. J. Exp. Med. 203:109310
82. Suzuki T, Franchi L, Toma C, Ashida H, Ogawa M, et al. 2007. Differential regulation of caspas
activation, pyroptosis, and autophagy via Ipaf and ASC in Shigella-infected macrophages. PLoS Pat
3:e111
83. Yamamoto Y, Klein TW, Friedman H. 1991. Legionella pneumophila growth in macrophages from s
ceptible mice is genetically controlled. Proc. Soc. Exp. Biol. Med. 196:4059
84. Yamamoto Y, Klein TW, Friedman H. 1992. Genetic control of macrophage susceptibility to infect
byLegionella pneumophila. FEMS Microbiol. Immunol. 4:13745
85. Fortier A, Min-Oo G, Forbes J, Lam-Yuk-Tseung S, Gros P. 2005. Single gene effects in mouse mod
of host/pathogen interactions. J. Leukoc. Biol. 77:8687786. Fortier A, de Chastellier C, Balor S, Gros P. 2007. Birc1e/Naip5 rapidly antagonizes modulation
phagosome maturation byLegionella pneumophila. Cell Microbiol. 9:91023
87. Zamboni DS,Kobayashi KS,Kohlsdorf T, Ogura Y, Long EM, et al. 2006. TheBirc1ecytosolic patte
recognition receptor contributes to the detection and control of Legionella pneumophila infection. N
Immunol. 7:31825
88. Ren T, Zamboni DS, Roy CR, Dietrich WF, Vance RE. 2006. Flagellin-deficient Legionella muta
evade caspase-1- and Naip5-mediated macrophage immunity. PLoS Pathog. 2:e18
394 Chen et al.
-
8/6/2019 Annurev.pathol NOD
31/36
89. Lamkanfi M, Amer A, Kanneganti TD, Munoz-Planillo R, Chen G, et al. 2007. The Nod-like receptor
family member Naip5/Birc1e restricts Legionella pneumophila growth independently of caspase-1 activa-
tion. J. Immunol. 178:802227
90. Amer AO, Swanson MS. 2005. Autophagy is an immediate macrophage response to Legionella pneu-
mophila. Cell Microbiol. 7:76578
91. Miao EA, Ernst RK, Dors M, Mao DP, Aderem A. 2008. Pseudomonas aeruginosa activates caspase 1
through Ipaf. Proc. Natl. Acad. Sci. USA 105:256267
92. Boyden ED, Dietrich WF. 2006. Nalp1b controls mouse macrophage susceptibility to anthrax lethal
toxin. Nat. Genet. 38:2404493. Kanneganti TD, Ozoren N, Body-Malapel M, Amer A, Park JH, et al. 2006. Bacterial RNA and small
antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature 440:23336
94. Muruve DA, Petrilli V, Zaiss AK, White LR, Clark SA, et al. 2008. The inflammasome recognizes
cytosolic microbial and host DNA and triggers an innate immune response. Nature 452:1037
95. Martinon F, Petrilli V, Mayor A, Tardivel A, Tschopp J. 2006. Gout-associated uric acid crystals activate
the NALP3 inflammasome. Nature 440:23741
96. Locovei S, Wang J, Dahl G. 2006. Activation of pannexin 1 channels by ATP through P2Y receptors
and by cytoplasmic calcium. FEBS Lett. 580:23944
97. Pelegrin P, Surprenant A. 2006. Pannexin-1 mediates large pore formation and interleukin-1 release
by the ATP-gated P2X7 receptor. EMBO J. 25:507182