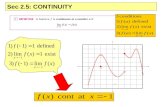
Aging Q3: Continuity of care Kimberly S. Davis, MD Physician Clinical Director, University Internal...
-
Upload
dwayne-lawrence -
Category
Documents
-
view
216 -
download
0
Transcript of Aging Q3: Continuity of care Kimberly S. Davis, MD Physician Clinical Director, University Internal...
Aging Q3: Continuity of Aging Q3: Continuity of carecare
Kimberly S. Davis, MDKimberly S. Davis, MD
Physician Clinical Director, Physician Clinical Director, University Internal MedicineUniversity Internal Medicine
AgendaAgenda
• Having a primary care physician: How Having a primary care physician: How much of a difference does it make much of a difference does it make towards patient care? Is it valuable?towards patient care? Is it valuable?
• Anatomy of Primary Care Anatomy of Primary Care • Outpatient medication reconciliationOutpatient medication reconciliation• Using Practice Partner as a tool to Using Practice Partner as a tool to
communicatecommunicate– short cuts for the usershort cuts for the user
Continuity and Coordination Continuity and Coordination of Careof Care
Continuity is ‘‘care over time by a Continuity is ‘‘care over time by a single individual or team of single individual or team of healthcare professionals’’ includinghealthcare professionals’’ including‘‘effective and timely communication ‘‘effective and timely communication of healthcare information.’’of healthcare information.’’ Institute of Medicine 1996Institute of Medicine 1996
Continuity and Coordination Continuity and Coordination of Careof Care
Continuity and coordination of care Continuity and coordination of care have several components,have several components,including aincluding a longitudinal longitudinal relationship relationship with awith a single single identifiable provider identifiable provider and and cooperationcooperation betweenbetween providersprovidersand between venues of care.and between venues of care.Meijer et al. Int J Qual Health Care 1997;9:23–33.Meijer et al. Int J Qual Health Care 1997;9:23–33.
The next few slides will show The next few slides will show some of the evidence that some of the evidence that Primary Care Primary Care isis effective---and effective---and improves quality of care and improves quality of care and outcomes as well as reduces outcomes as well as reduces cost!cost!
Evidence: Primary care Evidence: Primary care improves improves process of careprocess of care
Persons who receive primary care Persons who receive primary care are:are:
• More likely to More likely to receive the receive the recommended preventive servicesrecommended preventive services
• More likely to More likely to adhere to treatmentadhere to treatment
• More likely to More likely to be satisfiedbe satisfied with with their caretheir care
Bindman and Grumbach, J Gen Intern Med 1996;11:269. Bindman and Grumbach, J Gen Intern Med 1996;11:269. Safran et al. J Fam Pract 1998;47:213Safran et al. J Fam Pract 1998;47:213
Evidence: Primary care Evidence: Primary care improves outcomesimproves outcomes
• Breast cancer: Breast cancer: early detection is early detection is greatergreater when the supply of when the supply of primary care physicians is higherprimary care physicians is higher
• Cervical cancer: Cervical cancer: Incidence of Incidence of advanced stage presentation is advanced stage presentation is lowerlower in areas well-supplied with in areas well-supplied with family physiciansfamily physicians
• No advantage having a greater No advantage having a greater supply of specialist physicianssupply of specialist physicians
Ferrante et al. J Am Board Fam Pract 2000;13:408. Ferrante et al. J Am Board Fam Pract 2000;13:408. Campbell et al. Fam Med 2003;35:60Campbell et al. Fam Med 2003;35:60
Evidence: Primary care Evidence: Primary care improves outcomes and improves outcomes and reduces costsreduces costs
Adults with a primary care physician Adults with a primary care physician rather than a specialist as their rather than a specialist as their personal physicianpersonal physician
• 33% lower annual adjusted cost33% lower annual adjusted cost of care of care
• 19% lower adjusted mortality19% lower adjusted mortality, , controlling for age, gender, income, controlling for age, gender, income, insurance, smoking, perceived health insurance, smoking, perceived health (SF-36) and 11 major health conditions(SF-36) and 11 major health conditions
Franks and Fiscella. J Fam Pract 1998;47:103Franks and Fiscella. J Fam Pract 1998;47:103
Evidence: Primary care Evidence: Primary care improves outcomes and improves outcomes and reduces costsreduces costs
For 24 common quality indicators for For 24 common quality indicators for Medicare patients:Medicare patients:
• High quality significantly associated with High quality significantly associated with lower per capita Medicare expenditureslower per capita Medicare expenditures
• States with a greater ratio of generalist States with a greater ratio of generalist physicians to population had physicians to population had higher higher quality and lower costsquality and lower costs
• States with a greater ratio of specialist States with a greater ratio of specialist physicians to population had lower quality physicians to population had lower quality and higher costsand higher costs
Baicker and Chandra. Health Affairs Web Exclusive. April 7, 2004.Baicker and Chandra. Health Affairs Web Exclusive. April 7, 2004.
Evidence: Primary care Evidence: Primary care improves outcomes and improves outcomes and reduces costsreduces costs
• The higher the primary care to population The higher the primary care to population ratio the lower the ratio the lower the hospitalization rate for 6 hospitalization rate for 6 ambulatory sensitive conditionsambulatory sensitive conditions (asthma, (asthma, copd, chf, diabetes)copd, chf, diabetes)
• Health care costs are higher in regions with Health care costs are higher in regions with higher ratios of specialists to generalists higher ratios of specialists to generalists
Parchman and Culler. J Fam Pract 1994;39:123Parchman and Culler. J Fam Pract 1994;39:123 Welch et al. Welch et al. NEJM 1993;328:621NEJM 1993;328:621
Evidence: Primary care Evidence: Primary care reduces disparities in carereduces disparities in care
• Reduced stroke riskReduced stroke risk
• Better CAD care and reduced CAD Better CAD care and reduced CAD mortalitymortality
• Narrows effect of income and Narrows effect of income and gender differences on care gender differences on care outcomesoutcomes
Starfield, Shi, Macinko. The Milbank Quarterly, Vol. 83, Starfield, Shi, Macinko. The Milbank Quarterly, Vol. 83, No. 3, 2005 (pp. 457–502)No. 3, 2005 (pp. 457–502)
Continuity of Care ACOVE:Continuity of Care ACOVE:Quality IndicatorsQuality Indicators
• Identification of source of careIdentification of source of care• Follow up on medication in Follow up on medication in
outpatient settingoutpatient setting• Continuity of medication between Continuity of medication between
physiciansphysicians• Continuity in the ED and at Hospital Continuity in the ED and at Hospital
AdmissionAdmission• Follow up after hospital dischargeFollow up after hospital discharge
General InternistsGeneral Internists
• Average General Internist has a Average General Internist has a panel of 1500-2000 patientspanel of 1500-2000 patients
• At 20 visits a day, we do 130,000 At 20 visits a day, we do 130,000 outpatient visits in a careeroutpatient visits in a career
• We should review what we doWe should review what we do
Components of Meaningful Components of Meaningful Primary care VisitPrimary care Visit
• Pre-visitPre-visit
• VisitVisit
• Post-visit Follow-upPost-visit Follow-up
• Inter-visit care Inter-visit care
Components of primary care: Components of primary care: Pre-visitPre-visit
• How to prep for clinic visitHow to prep for clinic visit– Review notes—your last note, any notes Review notes—your last note, any notes
by other MDs in the interim, ER or by other MDs in the interim, ER or discharge summariesdischarge summaries
– Review interim labs Review interim labs – Review interim studies—ex mammo, Review interim studies—ex mammo,
stress test, colonoscopy, etcstress test, colonoscopy, etc– Review any consultsReview any consults– Set up any needed health maintenanceSet up any needed health maintenance
Components of primary care: Components of primary care: VisitVisit
• Inform pt. of their PCP and nurse – Inform pt. of their PCP and nurse – provide resources (card and photo provide resources (card and photo composite) composite)
• Review all meds (purpose, frequency, Review all meds (purpose, frequency, dose, other) with patient and give them a dose, other) with patient and give them a copy of the updated med listcopy of the updated med list
• Give patient a medication bag; Give patient a medication bag; encourage taking it with them to all encourage taking it with them to all provider visitsprovider visits
Segments of primary care: Segments of primary care: Post-visit Follow-upPost-visit Follow-up
• Assign PCP in EMR Assign PCP in EMR
• Document diagnostic test and studies Document diagnostic test and studies ordered and pending (IP) and FU on themordered and pending (IP) and FU on them
• Notify UIM PCP when seeing another Notify UIM PCP when seeing another providers patient by using the .cc code providers patient by using the .cc code (OP)(OP)
• How to look up provider codes in EMR How to look up provider codes in EMR through knowledge base.through knowledge base.
• Notify patients of test results Notify patients of test results
So…what does this mean So…what does this mean to you?to you?
What will you be What will you be doing in this part of doing in this part of
Aging Q3?Aging Q3?
Aging Q3CONTINUITY OF CARE – Outpatient Blue sheet
PCT or Nurse:YES NO
1. Have you visited the ER, been admitted to the hospital, or seen any other providers since your last visit to this clinic?
2. Did you bring your pill bottles with you today?
3. Did you bring your medication list with you today?
4. Are you taking any over-the-counter drugs, vitamins or supplements?
Continuity of CareContinuity of Care POSTER POSTERPatients 65 years and older have multiple medical problems, arePatients 65 years and older have multiple medical problems, areon multiple medications, and are seen by multiple providers. Having on multiple medications, and are seen by multiple providers. Having a primary care physician, communicating among all providers, and a primary care physician, communicating among all providers, and reconciling medications are all essential for quality patient care.reconciling medications are all essential for quality patient care.
Ask the patient…Ask the patient…
1. What are the names of 1. What are the names of the medications (including the medications (including OTC, vitamins and herbal OTC, vitamins and herbal supplements) you are supplements) you are currently taking?currently taking?
2. How do you take your 2. How do you take your medications and how medications and how much have you been much have you been taking?taking?
3. Do you understand 3. Do you understand what the medication is what the medication is for?for?
4. Where do you get your 4. Where do you get your prescriptions filled?prescriptions filled?
MD action…MD action…
1. Compare list to the list 1. Compare list to the list in the patient’s chart.in the patient’s chart.
2. Compare dose, 2. Compare dose, frequency, with/without frequency, with/without food..food..
3. If not, teach the 3. If not, teach the patient. Use plain, non-patient. Use plain, non-medical language; speak medical language; speak slowly; break down slowly; break down information into short information into short statements.statements.
4. Call the pharmacy if 4. Call the pharmacy if there is any discrepancy there is any discrepancy between the patient’s between the patient’s reported meds and your reported meds and your list. Rectify in the list. Rectify in the patient’s chart.patient’s chart.
5. Be sure there is a clear 5. Be sure there is a clear indication for each indication for each medication.medication.
Medication Reconciliation Steps
References: Wenger, N.S. and R.T. Young (2007) “Quality Indicators for Continuity and Coordination of Care in Vulnerable Elders.” JAGS 55:S285-292.Varkey, P. et al (2007) “Improving Medication Reconciliation in the Outpatient Setting.” Jt. Comm J on Quality & Patient Safety 33:5.
Funding provided by D.W. Reynolds Foundation
So why do Med So why do Med reconciliation?reconciliation?
• It is a Joint commission requirement It is a Joint commission requirement for both inpatient and outpatientfor both inpatient and outpatient
• Patient safety ---ADE higher in 65+ Patient safety ---ADE higher in 65+ age groupage group
• Quality CareQuality Care
Adverse Drug EventsAdverse Drug Events
• 2 year national study 1/2004-2 year national study 1/2004-12/2005, there were 21,298 ADE 12/2005, there were 21,298 ADE reported or 2 per every 1000 reported or 2 per every 1000 required ER visits.required ER visits.
• Estimate closer to 700,000Estimate closer to 700,000
• More likely in the 65+ population to More likely in the 65+ population to have ADEhave ADE
Meds initiated by ER, other specialist doctors, hospital DC reevaluate need for continuation of each medication and duplication. There must be an indication for every medication.
Ask about OTC medication and herbal supplements
Encourage patient to bring all medications to every visit.
Aging Q3CONTINUITY OF CARE – Outpatient
MD ACTION REMEMBER TO:
Update the Medication list and give a copy to the patient.
Give the patient a business card.
Tell the patient how to reach a UIM physician after hours.
Show the patient your Team Photo page and explain the practice team concept.
Give the patient a medication bag if appropriate.
Segments of primary care: Segments of primary care: Inter-visit care Inter-visit care
• Complete timely DC summary and include Complete timely DC summary and include the PCP name, H & P, and do med the PCP name, H & P, and do med reconciliationreconciliation
• Keep in mind patients medications may Keep in mind patients medications may change when admitted based on MUSC’s change when admitted based on MUSC’s Automatic Therapeutic SubstitutionAutomatic Therapeutic Substitution and and they need to be changed back to patients they need to be changed back to patients insurance formulary at the time of discharge. insurance formulary at the time of discharge.
How do you know when your How do you know when your patient is in ER or hospitalized?patient is in ER or hospitalized?
• Contracted with company, DDIContracted with company, DDI• Automated notification system when they are Automated notification system when they are
hospitalized or in ERhospitalized or in ER• You and your case manager will be notified You and your case manager will be notified
via email via email • Expectation- Visit or call patient during Expectation- Visit or call patient during
hospitalization when notified of their hospitalization when notified of their admission admission
• Case manager will ensure appropriate f/u with Case manager will ensure appropriate f/u with you and that they are getting new meds filled.you and that they are getting new meds filled.
Aging Q3 Continuity of Care ACOVE 4
Inpatient
Primary Care Clinic MD ________________________________________NAME
Was the letter on the reverse side faxed to the primary care office?
YES _____ NO _____
UIM Resident Fax #792-0448
UIM Faculty Practice Fax #876-0767
Other local MD’s Fax #s can be found on the Aging Q3 website:
http://mcintranet.musc.edu/agingq3
Yellow SheetYellow Sheet
Date _________________________________
Dear Dr. _________________________________ Fax # _______________________
Your patient, ____________________________________, DOB, ____/____/____ was admitted
to the Medical University of South Carolina, General Medicine Service, on ____/____/____ with a
diagnosis of _______________________________________.
We will be contacting you just prior to their discharge to make arrangements for follow up. In the meantime if you need to contact us, please feel free to page Dr. ________________________ at 843-792-2123 pager # _________________.
Thanks for allowing us to participate in your patient’s care.
Physicians at MUSC
Continuity of Care: UIM Note Template Primary Care Provider: (Pull-down list required)
Has the patient been to the ER, or admitted to the hospital, or seen other out-patient doctors since the last visit to this clinic? YES NO
Did the patient bring all their pill bottles with them today? YES NO
Are they taking any OTC medications, vitamins or supplements? YES NO
Did you perform medication reconciliation today? YES NO
Did you give a copy of the updated medication list to the patient? YES NO
Did you give the patient a medication bag? YES NO(Already has one)
Did you give your business card to your patient today? YES NO(NO, I am a unit resident or my patient already has one)
Practice Partner TIPsPractice Partner TIPs
• How to assign a PCP provider-pick list onlyHow to assign a PCP provider-pick list only
• How to write a new prescriptionHow to write a new prescription
• How to renew a prescriptionHow to renew a prescription
• How to print the ‘reconciled’ med listHow to print the ‘reconciled’ med list
• How to look up a provider ID in PP using How to look up a provider ID in PP using Knowledge Base?Knowledge Base?
• How to do a .CC to your partners so they How to do a .CC to your partners so they are aware of what has gone on w their are aware of what has gone on w their patients. patients.