Acid-Base Equilibrium Fate Bicarbonate in...
Transcript of Acid-Base Equilibrium Fate Bicarbonate in...

Influence of Steady-State Alterations inAcid-Base Equilibrium on theFate of Administered Bicarbonate in the Dog
HORACIOJ. ADROGUE,JEFFREY BRENSILVER, JORDANJ. COHEN, andNICOLAos E. MADIAS, Department of Medicine, Tufts University School ofMedicine and the Division of Nephrology, Tufts-New England MedicalCenter, Boston, Massachusetts 02111
A B S T R A C T Previous workers have shown that met-abolic acidosis increases the apparent space throughwhich administered bicarbonate is distributed. Thisfinding has been ascribed to the accompanying aci-demia and to the consequent availability of a largequantity of hydrogen ion that accumulates on nonbi-carbonate tissue buffers during the development ofacidosis. To test this hypothesis, bicarbonate space wasmeasured in dogs with a broad range of steady-stateplasma [HCO-] in association with alkalemia as wellas with acidemia. Appropriate combinations of pH andplasma [HCO-] were achieved by pretreating the an-imals to produce graded degrees of each of the fourcardinal, chronic acid-base disorders. Metabolic aci-dosis (n = 15) was produced by prolonged HCI-feed-ing; metabolic alkalosis (n = 17) by diuretics and achloride-free diet; and respiratory acidosis (n = 9) andalkalosis (n = 8) by means of an environmental cham-ber. Animals with normal acid-base status (n = 4) werealso studied. Sodium bicarbonate (5 mmol/kg) was in-fused over 10 min to the unanesthetized animals; ob-servations were carried out over 90 min. The resultsobtained from animals with metabolic acid-base dis-turbances demonstrated an inverse relationship be-tween bicarbonate space and initial plasma pH, con-
A preliminary report of this study was presented in ab-stract form at the American Society of Nephrology Meetingin 1977.
Dr. N. E. Madias is an Established Investigator of theAmerican Heart Association. Address reprint requests to Dr.Madias, Tufts-New England Medical Center, Boston, MA02111. Dr. H. J. Adrogue is currently at the Methodist Hos-pital, Houston, TX. Dr. J. Brensilver is currently at the St.Luke's Hospital Center, New York City. Dr. J. J. Cohen iscurrently at the Michael Reese Hospital and Medical Center,Chicago, IL.
Received for publication 1 I February 1982 and in revisedform 25 October 1982.
firming the previous findings of others. By contrast,the results obtained in animals with respiratory acid-base disturbances demonstrated a direct relationshipbetween bicarbonate space and initial plasma pH. Thepooled data revealed that bicarbonate space is, in fact,quite independent of the initial pH but is highly cor-related with the initial level of extracellular [HCOJ];dogs with low extracellular [HCOQ] (s10 meq/liter)whether acidemic or alkalemic, have a bicarbonatespace that is 25% larger than normal and some 50%larger than in dogs with high extracellular [HCO ](n50 meq/liter). Weconclude from these results thatthe increased bicarbonate space in metabolic acidosis(and respiratory alkalosis) does not reflect the avail-ability of more hydrogen ions for release during bi-carbonate administration, but merely evidences thewider range of titration (ApH) of nonbicarbonate buff-ers that occurs during alkali loading whenever plasma[HCO3] is low.
INTRODUCTION
The fate of administered bicarbonate is conventionallydescribed in terms of the apparent space of distributionfor this ion. Because a sizeable portion of administeredbicarbonate is dissipated by body buffers, one can en-vision the apparent space of distribution as havinganatomical and nonanatomical subdivisions; the ana-tomical portion corresponds to the extracellular vol-ume in which bicarbonate is freely dissolved, and thenonanatomical, to a purely theoretical "space" largeenough to accomodate (at the prevailing extracellularbicarbonate concentration) all of the administered bi-carbonate unaccounted for by extracellular stores.Numerous observations have established that the an-atomic and nonanatomic portions of the apparent bi-carbonate space are approximately equal in size in
J. Clin. Invest. © The American Society for Clinical Investigation, Inc. * 0021-9738/83/04/0867/17 $1.00Volume 71 April 1983 867-883
867

normal individuals, i.e., that the apparent bicarbonatespace is -40-50% of body weight as compared withan extracellular fluid volume of -20% of bodyweight (1-6).
Bicarbonate is often administered to patients withmetabolic acidosis and such use has prompted inves-tigators to examine the effect of acidosis on the ap-parent space of distribution for this ion. Although ear-lier workers had concluded that metabolic acidosis hasa negligible effect on the internal distribution of ad-ministered bicarbonate (4, 7), more recent studiesdemonstrated a significant enlargement of the bicar-bonate space under these circumstances (5, 6). Thislatter finding was ascribed to the associated acidemiaand to the consequent availability of a large quantityof hydrogen ion on nonbicarbonate (largely intracel-lular) buffers that accumulated during the develop-ment of acidosis. An alternative possibility, whichseemed equally plausible to us, is that a low level ofplasma bicarbonate concentration, per se, mandatesan enlargement of the bicarbonate space by enlargingthe range of pH over which nonbicarbonate bufferswill be titrated by a given quantity of administeredbase.
This study was designed to distinguish between thesealternatives. The apparent bicarbonate space was ex-amined in animals with widely different levels ofplasma pH but similar values for plasma bicarbonateconcentration. The results indicate that the enlarge-ment of bicarbonate space in animals with metabolicacidosis is a consequence not of acidemia but of thelow plasma bicarbonate concentration.
METHODS53 acute bicarbonate infusion studies were carried out on36 female mongrel dogs ranging in weight between 10.2 and18.2 kg. The animals were fed 30 g/kg per d of a syntheticdiet until the day of infusion. The diet contained <1.0 meqsodium/100 g, <0.1 meq potassium/100 g, and <0.5 meqchloride/100 g (8). The daily diet was supplemented with2.5 meq/kg body wt of potassium as neutral phosphate and2.5 mmol/kg body wt of sodium chloride, except as notedbelow. The diet was homogenized with twice its weight ofdistilled water before feeding. Animals that did not eat spon-taneously were tube fed; animals that vomited were excludedfrom further study. Blood samples were obtained by per-cutaneous arterial puncture; rectal temperature was mea-sured at the time of blood sampling.
Five groups of animals were prepared before the acuteinfusion with the intent of achieving a broad range of steady-state plasma bicarbonate concentrations in association withacidemia as well as with alkalemia. Accordingly, animalswith each of the four cardinal acid-base disturbances andanimals with normal acid-base status were studied.'
'In some instances, a given animal received two bicar-bonate infusions, one at each of two levels of severity of thesame acid-base disturbance.
Group 1. Chronic metabolic acidosisMetabolic acidosis (nine dogs, 15 studies) of graded se-
verity was induced by adding hydrochloric acid or L-lysine-monohydrochloride (Sigma Chemical Co., St. Louis, MO) tothe daily diet. For a given study, the same daily dose of acidwas used throughout but, to achieve a wide range of steady.state bicarbonate decrements for the group as a whole, thedaily dose of acid ranged between 2 and 8 mmol/kg bodywt. The development of a chronic steady state was insuredby feeding the acid for at least 7 d (9).
Group 2. Chronic respiratory alkalosisSustained hyperventilation (seven dogs, eight studies) was
produced by exposing the animals to an hypoxic atmospherewithin a large environmental chamber (10). The ambientoxygen concentration within the chamber was lowered from21 to 9% over a period of 2-3 d. The chamber atmospherewas maintained at a level of 9% oxygen for at least 7 d, aperiod known to be adequate for the development of achronic steady state (11).
Group 3. Chronic respiratory acidosisRespiratory acidosis (seven dogs, nine studies) was pro-
duced by exposing the animals to carbon dioxide within alarge environmental chamber (10). The animals were main-tained at a given level of inspired carbon dioxide (8 and/or11%) for at least 7 d, a period known to be adequate for thedevelopment of a chronic steady state (8). A normal atmo-spheric oxygen concentration of 21% was maintained in allstudies.
Group 4. Chronic metabolic alkalosisMetabolic alkalosis (13 dogs, 17 studies) of graded severity
was produced by administering ethacrynic acid, 50 mgorally, for 1-5 d. To obviate correction of the diuretic-in-duced alkalosis, sodium neutral-phosphate was substitutedfor the dietary sodium chloride supplement used in the othergroups. 5 d were allowed to lapse after the last dose of etha-crynic acid before evidence for a chronic steady state ofacid-base equilibrium was sought.
Group 5. Normal acid-base equilibriumFour dogs were used in the four studies performed. Four
of the animals used in group 4 were also studied under nor-mal conditions several days before the induction of meta-bolic alkalosis.
Acute experimental protocolEach animal received an acute sodium bicarbonate in-
fusion following the establishment of a chronic steady stateof acid-base equilibrium. In each instance, a chronic steadystate was judged to have been present when neither PaCO2nor plasma bicarbonate concentration varied by > ±5% fromthe mean value for at least three consecutive days before theacute infusion.
On the day of the acute experiment, each animal wasweighed and allowed to lie comfortably on a table; the dietwas witheld. An indwelling bladder catheter was placed
H. J. Adrogue, J. Brensilver, J. J. Cohen, and N. E. Madias868

under topical anesthesia (xylocaine jelly, Astra Company,Worcester, MA). Body weight was corrected for residualurine volume. 10-15 ml of an aqueous solution of sodiumradiosulfate (35S, New England Nuclear, Boston, MA) wasinjected into a peripheral vein; the dose of 35S was calculatedto deliver -0.25 ,uCi/kg body wt. Arterial blood sampleswere obtained at 30, 60, 90, and 120 min after injection formeasurement of plasma sulfate radioactivity. The 90- and120-min samples were also utilized for base-line measure-ments of electrolyte and acid-base composition.
Animals were accepted for study only if (a) the mean ofthe two control values for plasma bicarbonate concentrationdiffered by no >2 meq/liter from the value obtained on theprevious day and (b) the mean of the two control observationsfor PaCO2differed by no >3 mmHgor 10% (whichever wasgreater) from the value obtained on the previous day.
Sodium bicarbonate, 5 mmol/kg body wt, was adminis-tered intravenously as a 1-N solution over a 10-min period.Arterial blood samples (10 ml) were drawn anaerobically at30, 60, and 90 min from the midpoint of the infusion. Urinewas collected anaerobically in four consecutive periods, onebefore bicarbonate infusion and three at 30-min intervalsfollowing bicarbonate infusion; complete bladder emptyingwas achieved by manual compression over the suprapubicarea.
Analytical methodsMethods used for determining sodium, potassium, and
chloride have been reported previously (12). Total CO2 wasmeasured by autoanalyzer (Technicon Instruments Corp.,Tarrytown, NY) and the results were confirmed daily by themanometric technique of Peters and Van Slyke accordingto a protocol previously described (13). pH was measuredanaerobically at 39°C by glass electrode (13). Bicarbonateconcentration and PaCO2 were calculated from the Hen-derson-Hasselbalch equation. pH, pK', and the solubilitycoefficient of CO2 were corrected for temperature; pK' wasalso corrected for pH (14-16). Total plasma protein concen-tration was determined by refractometry (17). 35S beta-ra-dioactivity was measured in a liquid scintillation solution(ACS, Amersham Corp., Arlington Heights, IL) using a Tri-Carb scintillation spectrometer (model 3002, Packard In-strument Co., Downers Grove, IL).
Calculations and definitionsThe concentration of plasma water (in kilograms per liter)
was calculated from the plasma total protein concentration(in grams per deciliter) by the following equation: [H2OIp= 0.986 - 0.00745 [Pr]p (18). The extracellular concentra-tions of anions and cations were calculated from their con-centrations in plasma water using a correction factor of 0.95for the Donnan effect. Initial total erythrocyte volume wascalculated from the hematocrit and an assumed plasma vol-ume of 0.045 liter/kg body wt. Subsequent values for totalerythrocyte volume were corrected for the quantity of bloodremoved during the experiment.
Initial extracellular fluid (iECF) volume was estimatedfrom the radiosulfate space (19). The counts per liter ofplasma water (corrected for Donnan effect) were divided byinjected counts for each of the four blood samples obtainedbefore bicarbonate infusion. Radiosulfate space was calcu-lated from the zero-time intercept of the least squares linedrawn through the logarithms of these quotients (19).
Changes in extracellular fluid (ECF)2 volume (AECF) fol-lowing bicarbonate infusion were estimated using chloridespace arithmetic, as follows:
AECF = eECF - iECF,
eECF = (iECF X i[CIj]e + bcI)/e[Clie,where eECF = experimental ECF volume, iECF = initialECF volume (radiosulfate space), i[Cl-Lj = initial extracel-lular chloride concentration, bc1 = chloride balance, ande[Cl-e = experimental extracellular chloride concentration(18). Because no chloride was administered, the term bc1represents urinary chloride losses over the respective timeinterval. Chloride space arithmetic assumes that internalshifts of chloride do not occur.
Correcting [HCO-7, and pH for the effectsof acute changes in PaCO2Bicarbonate loading tends to elevate PaCO2 for two rea-
sons: (a) carbon dioxide is generated as some of the admin-istered bicarbonate is titrated and (b) ventilation is dam-pened by the alkalinizing effects of the administered base.Although the resulting change in PaCO2 is small (Results),to whatever extent hypercapnia does accompany bicarbon-ate loading, some portion of the measured increment in[HCO-Ip will reflect the titration of nonbicarbonate buffersby carbonic acid (21). This unwanted influence on [HCO-Lcould, in theory, have been eliminated by controlling ven-tilation, but anesthesia would have been required to do so.To avoid anesthesia, we chose instead to calculate the smalleffect of the observed change in PaCO2 and to correct themeasured value for [HCO],, accordingly. Estimates of theinfluence of acute increments in PaCO2 on [HCO.-],, werederived from experiments in which acute hypercapnia wasproduced in unanesthetized dogs with chronic steady statesof acid-base equilibrium identical to those studied here (22,23). A value of 0.18 meq/liter per mmHgincrement inPaCO2was used for normal animals, animals with metabolicacidosis, and animals with metabolic alkalosis; a value of0.26 meq/liter per mmHgincrement in PaCO2was used foranimals with respiratory alkalosis.3 In no instance did cor-recting [HCO-1. for the effects of PaCO2 require a downwardadjustment by more than 1.3 meq/liter.
For purposes of data analysis, it was necessary to havevalues for blood pH following bicarbonate infusion that wereuninfluenced either by changes in PaCO2 per se or by thatportion of the A[HCOI, related to changes in PaCO2. Ac-cordingly, postinfusion values for pH (pHc) were calculated(using the Henderson-Hasselbalch equation) from the re-spective control value for PaCO2and the corrected value forplasma bicarbonate ([HCO-]J), as defined above.
Fate of retained bicarbonateThe amount of bicarbonate retained ("retained bicarbon-
ate") at any time following the acute infusion was calculated
2 Abbreviations used in this paper: bcl, chloride balance;c, corrected value (Methods); e, before an abbreviation ex-perimental; after an abbreviation extracellular; ECF, extra-cellular fluid; i, initial.
3 Animals with respiratory acidosis did not experience achange in PaCO2during bicarbonate loading (Results), pre-sumably because ventilation was maximally stimulated bythe elevated FiCO2.
Bicarbonate Space in Chronic Acid-Base Disturbances 869

as the difference between the amount administered and theaccumulated change in urinary bicarbonate excretion. Hav-ing an independent measure of the extracellular space aswell as measurements of protein concentration and eryth-rocyte mass permitted an explicit accounting of much of theretained bicarbonate. Two major divisions and several sub-divisions of retained bicarbonate were defined as follows:
Bicarbonate freely dissolved in the ECF. (a) Bicarbonateretained within the original volume of extracellular fluid(iECF) was calculated as the product of iECF volume andthe A[HCO-1.
(b) Bicarbonate retained within the increment in extra-cellular volume produced by the acute infusion was calcu-lated as the product of AECF volume and the prevail-ing [HCO-].
Bicarbonate not freely dissolved in the ECF. (a) Bicar-bonate titrated by protons released from plasma proteins wasestimated as 0.11 times the product of A plasma pHc, plasmatotal protein concentration and plasma volume (assumed tobe constant at 4.5% body wt). The factor, 0.11, is the buffervalue of plasma proteins expressed as millimoles per gramper pH unit (24, 25).
(b) Bicarbonate retained in erythrocytes was calculatedas 0.5 times the product of A[HCO-], and total erythrocytevolume. The factor 0.5 was taken as the ratio of bicarbonateconcentration in erythrocytes to that in plasma (3, 25).
(c) Bicarbonate titrated by protons released from hemo-globin was estimated as 60 times the product of A plasmapHc and total erythrocyte volume. The factor, 60, is theproduct of the molar buffer value of hemoglobin (which istaken to be 3) and millimoles of hemoglobin per liter eryth-rocytes (which is assumed to be 20) (26).
(d) Bicarbonate entering the "intracellular compartment"was estimated as the difference between total retained bi-carbonate and the sum of the bicarbonate accounted forexplicitly by the above calculations. Consequently, this sub-division of retained bicarbonate corresponds to the aggregatecontribution of all non-extracellular repositories includingskeletal muscle, visceral organs, other soft tissues, and bone(3, 27).
The theoretical fluid volume through which retained bi-carbonate appeared to distribute ("apparent bicarbonatespace") was calculated by dividing retained bicarbonate bythe change in extracellular bicarbonate concentration(A[HCOj]J) and was expressed as a percentage of bodyweight. This conventional definition of bicarbonate spacewas modified only to the extent that A[HCO3j1 was correctedfor the simultaneous APaCO2, as discussed above.
Statistical analysisStatistical analyses were carried out by means of analysis
of variance for paired or unpaired groups of data, as ap-propriate. Regression functions were calculated accordingto conventional techniques. The terms "significant" or "sig-nificantly different" will be used, unless otherwise specified,to describe differences which have a P value of <0.01.
RESULTS
General remarks. The term "metabolic studies" isused in connection with pooled data from animals withmetabolic acidosis, metabolic alkalosis, and normalacid-base status; the term "respiratory studies" is usedin connection with pooled data from animals with re-
spiratory acidosis, respiratory alkalosis, and normalacid-base status. In some instances, data from all fivegroups are pooled for analysis.
Throughout the acute experimental protocol, all an-imals remained quiet, alert, and easy to manage. Ad-ministration of radiosulfate and sodium bicarbonateproduced no apparent ill effects.
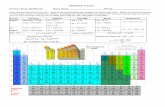
ECF volume and composition. As can be seen inTable I, mean ECF volume during control rangedfrom 23.0 to 26.4% of body wt among the five exper-imental groups. In no group did control ECF volumediffer significantly from that of any other; however,by design, the groups with chronic acid-base distur-bances featured graded degrees of severity. For thisreason, we combined in turn the data from normalswith that from each of the other groups and examinedthe least squares relationship between initial ECF vol-ume and initial extracellular bicarbonate concentra-tion. This analysis revealed a significant inverse rela-tionship for the metabolic alkalosis group (y = -0.18x+ 29.82, r = -0.447, P < 0.05), in keeping with theprogressively more severe volume depletion antici-pated in this group as a function of the severity of thediuretic-induced hyperbicarbonatemia. Analysis alsorevealed a significant direct relationship for the met-abolic acidosis group (y = 0.17x + 22.79, r = 0.469,P < 0.05), in accordance with the progressively greatercationic losses characteristic of mineral acid-inducedhypobicarbonatemia of graded severity (9). Under theconditions of these studies therefore, the mean iECFvolume expected for animals with i[HCO-L of 10, 21,or 50 meq/liter of metabolic origin was 24.5, 26.2, or20.8% of body wt, respectively. No significant rela-tionship between iECF volume and i[HCO3L was de-tected for either the respiratory acidosis or the respi-ratory alkalosis group.
Administration of sodium bicarbonate resulted inexpansion of ECF volume in all experimental groups;the degree of expansion was not significantly differentamong the groups and ranged from 60 to 129 ml at30 min. Thereafter, a progressive return of ECF vol-ume towards control was observed; in each group, thedegree of expansion at 90 min was significantly lessthan that at 30 min. Control hematocrit was signifi-cantly elevated in the group with chronic respiratoryalkalosis, in keeping with the hypoxia-induced hyper-ventilation imposed to produce this acid-base distur-bance. Hematocrit values, as well as plasma total pro-tein concentration were significantly lower in allgroups at 30 min after bicarbonate infusion; subse-quently, they tended to return towards control values.
Control plasma bicarbonate concentrations([HCOiL,), by design, covered a wide spectrum rangingfrom 8.5 to 16.5 meq/liter in animals with chronicmetabolic acidosis, from 11.9 to 15.2 meq/liter in an-
870 H. J. Adrogue', J. Brensilver, J. J. Cohen, and N. E. Madias

t- O CCD
+1
Ci Ci+1
+1
Ci N~~~~~~~CN +1 +1C]~~~ ~,,C' :+l +l
~C+1
C+ +l+1
+1+1
C] +1
C]
_cl s +l
+1
+1
+1 + +l
ClC
?- +1
+1
0 _c C- C]
c] +l +l
- C]
LC cll- Xc+ +l
+1
~~~~~~C~ ~ ~ CCA +
Biabnt Spac in
C] +l +l
- C]
s CC +l
Co C] :
X- C]t- CC *rCce CC +l
cc-~~~t cNx]+1 +l
C _ - C;C _~ ;-
Cs+l+
Bicarbonate Space in
t- c
~"+1_J_
C] ct +l
C] xC
C_ _
-r -ri
CC -
- +1
c +1
LC +1
C -
I- C]
C
CC!
* +1
C"
_ _1
l +l
CO +1
cc -C- O
C_ v
X] -r-r +l
XC -t- _
CC +lr- - C
CC +l
- +1l
+1
Incc
- +1
+1
..
t- t- C, X +l
CT, +lI - +l
_;
tz ~~~Z__
ChncAcdBs isubne
4
i-0
-0,
871
I
I
=
--: IIt-l= z
_11
-~

imals with chronic respiratory alkalosis, from 28.2 to36.4 meq/liter in animals with chronic respiratoryacidosis, from 23.0 to 42.3 meq/liter in animals withchronic metabolic alkalosis. Control plasma bicarbon-ate concentrations in animals with normal acid-baseequilibrium ranged from 18.9 to 20.4 meq/liter.
As shown in Table II, extracellular bicarbonate con-centration ([HCO1]') increased significantly in all groupsafter bicarbonate infusion. The change in [HCO],however, was not significantly different among groupsat any point of observation; mean values forA[HCO-]' varied from +9.1 to +10.5 meq/liter at 30min. Progressively smaller A[HCO-]c values were ob-served over the ensuing hour in all groups. Bicarbonateinfusion resulted in a small but significant incrementin PaCO2 in all but the respiratory acidosis group.PaCO2did not change significantly in any group overthe final hour of observation.
Plasma pHc, as did [HCO3], increased significantlyin all experimental groups following bicarbonate in-fusion.4 Values were maximally elevated at 30 min andreturned progressively towards control thereafter. Ascan be seen in Fig. 1, a significant inverse relationshipwas found between i[HCO-] and A plasma pHc at eachpoint of observation in both metabolic and respiratorystudies. When the 30-min data from all 53 studies werepooled, the hyperbolic function shown in the figureprovided an excellent fit, as assessed by covarianceanalysis. At 60 and 90 min, relationships with verysimilar slopes but lower intercepts were found (Fig.1, right hand panel).
As shown in Table II, extracellular sodium concen-tration in each group was significantly higher thancontrol at 30 min following sodium bicarbonate ad-ministration and remained elevated to the same degreein subsequent periods. Extracellular potassium con-centration, by contrast, fell significantly in all groupsby 30 min but, as with sodium concentration, remainedunchanged throughout the remainder of the study.Extracellular chloride concentration was significantlylower in all groups at 30 min after bicarbonate infusionand, in general, tended to return towards control overthe ensuing hour.
Plasma unmeasured anion concentration, defined as
4Values for pH during experimental periods were cal-culated from the corrected plasma [HCO-] and the prein-fusion PaCO2 (Methods). This calculated correction permit-ted an assessment of the effects of bicarbonate infusion, perse (i.e., without the complicating influence of unavoidablechanges in PaCO2). In each case, calculated pH values wereslightly higher than the corresponding measured values, re-flecting the fact that the observed APaCO2was proportion-ately greater than the required correction in plasmaA[HCO3]. The differences between measured and calculatedpH values ranged between 0.03 and 0.06 pH units.
the sum of plasma sodium and potassium concentra-tions minus the sum of plasma chloride and bicarbon-ate concentrations, was not significantly altered bybicarbonate infusion in any of the experimental groups.Furthermore, the small reduction in plasma proteinconcentration coupled with the rise in plasma pH thatwere observed after bicarbonate infusion left the an-ionic equivalency of plasma proteins virtually un-changed (28, 29). This observation, taken together withthe stability of the unmeasured anion concentration,serves to exclude a sizeable accumulation of organicacids following infusion of sodium bicarbonate.
Bicarbonate excretion. As can be seen in Table III,bicarbonate excretion was virtually nil during controlin all experimental groups and increased to a variableextent following bicarbonate infusion. Animals withmetabolic acidosis excreted the least amount of ad-ministered bicarbonate, whereas animals with respi-ratory acidosis excreted the most; cumulative bicar-bonate excretion at 90 min averaged 0.5% of the ad-ministered load in the metabolic acidosis group and43% of the administered load in the respiratory aci-dosis group. The corresponding values for the meta-bolic alkalosis and respiratory alkalosis groups were 35and 20%, respectively.
Fate of retained bicarbonate. Table IV depicts themean values for retained bicarbonate in the five ex-perimental groups at each point of observation. Withthe exception of the metabolic acidosis group, in whichbicarbonate excretion was negligible, the amount ofbicarbonate retained declined progressively as a func-tion of time but, in keeping with the differences inalkali excretion rates noted above, did so more rapidlythe higher the initial level of extracellular bicarbonateconcentration.
Using measurements of ECF volume, total plasmaprotein concentration and hematocrit, it was possibleto obtain a somewhat more explicit accounting of theinternal distribution of retained bicarbonate than thatprovided by the theoretic "apparent bicarbonatespace." As indicated in the Methods section, retainedbicarbonate can be thought of as existing in two majordivisions: (a) that freely dissolved in the ECF, includ-ing both the initial and the expanded portions thereofand (b) that not freely dissolved in the ECF, encom-passing the bicarbonate titrated by plasma proteins,dissolved in erythrocyte water, titrated by hemoglobin,and removed by the "intracellular" compartment (i.e.,soft tissue and bone buffers). The distribution of re-tained bicarbonate among these various subdivisionsis depicted in Table IV for each group at each pointof observation.
Marked differences were observed among the ani-mals with respect to the internal distribution of re-tained bicarbonate. A consistent and striking feature,
872 H. J. Adrogue', J. Brensilver, J. J. Cohen, and N. E. Madias

t-0 0- 0-_+1 -+1 -+1
Ci O 0s- Ct
+I - +1 +1
t4 - X 00+1 ++1 +1
r0N- 00
+1 ++1 +1
006 x0 0~,-+1 - +l - +l
N ++I c0 +1co- 00-oc
+1 C''+I +1 +l
-
+l N +I cs+l
+1 +1 +1
+1 0+1 -+1
-4 -0 t X
+1 0+I +I
04 0- CirXO
+l- - +l -+
C-
_4 0 - ?9+1 : +l - +1
+l -ro 0-
+1j +- +1
+1 C, +l - +1*>1-+- t-+
+ Ti - +I
+1 +IN
+10 01+-t1
- - - -
C, 10 C+l X +l - +
t~0
Bicarbonate Space in Chronic Acid-Base Disturbances 873
¢ sCE
s .rE
o .-EC -
o .'E
3 -E
o .'co E
, _ ,_
_ _Co .=
;v E
_ _
C: .-
_
_ ._
_
5t
-
3 E
o ._
co E
_ _
, _ ;
_ .=
s: E
-
o .=
;; E
_ _CO '-
_
V4
O arco
11
._
0
C-
e4
0
, 110._
C,
z -
0CN +1
t-0o) eqN +1
_CTN +i
O C-4t- +1
N +1
00
c0 +1
00
c0 +1
04i +1
in
CO +1
ND _0r +l
12
N 0'° +l
-O
1 +1
t +l
*: +l
0o +l
o1 +-
_ _ t-
t +1 +1
co+ +IC]O C6
q +l +1
t- t- 0
C,) Oq C 00 +1 +1
C1 +l +l
0 t0c+l +1
0 N-
I+l +1
c0+l +l
- +1 +1
tr- t-M +l +l
0t - NO?01- 00-t +l +l
0l~+1 +1
C+l +l
t- - t_
c0 +l +l
04+l +l
-q+l +l
cs+l +l
_0+1 +l
cs+I +l
.0
.s
0"-0
1 .~
1- COs
000 c
-
Q
0° +l
0 +l
0° +l
_ +l
0D-_ +l
_ +l
*9 +l
9. +°l
-O
0_ _
-t +l
t~ +1
t9 +1
+1
-i
7.-I .1
=
C ;=ab
; ;,
Z.

. 0
0
0
30 min.
I I
30 min
60 min90 min
I I
lo 20 30 40 50 10 20 30 40
Initial Extracellular [HCOS]meq /liter
50
Fi(IJRE 1 Relationship between initial extracellular bicarbonate concentration and change inplasma pH following sodium bicarbonate infusion. Experimental values for plasma pH were
calculated from the corrected plasma [HCO-] and the preinfusion PaCO2 (Methods). The left-hand panel depicts the relationship at 30 min after infusion. Filled circles denote values obtainedin dogs with metabolic acidosis and metabolic alkalosis. Open circles denote values obtainedin dogs with respiratory acidosis and respiratory alkalosis. Filled triangles denote values obtainedin dogs with normal acid-base status. The pooled data were best described by the hyperbolic
function, y = 2.38 + 0.032 (r = 0.957). The right-hand panel compares the relationship at 30x
min with those obtained at 60 min ( 2= 2+0.01,r=0.953) and 90 min y= +
0.001, r = 0.922) after the infusion. The intercepts, but not the slopes, of these relationships are
significantly different from each other. The slope of each relationship is significantly differentfrom zero.
however, was the dynamic nature of the distributionprocess. Thus, throughout the period of observation,an operational steady state was never achieved withregard either to the apparent space of distribution ofbicarbonate or to the compartmental distribution ofthe retained bicarbonate.
As shown in the left-hand panel of Fig. 2, pooleddata from all studies yielded a significant inverse cor-
relation between i[HCO-1 and the apparent space ofdistribution for bicarbonate; on the average, animalswith the lowest values for i(HCO4L (whether of respi-ratory or metabolic origin) had an '50% larger spaceof distribution at 30 min than animals with the highestvalues. As shown in the right-hand portion of Fig. 2,
the apparent space of distribution increased continu-ously during the postinfusion period but the stronginfluence exerted by the i[HCO-1C persisted throughout.Utilizing the relationships depicted in Fig. 2, one can
calculate that animals with an i[HCO41 of 10 meq/liter, whether of respiratory or of metabolic origin,will exhibit on average a bicarbonate space of '60%body wt at 30 min and 76% body wt at 90 min; at theopposite extreme, animals with an i(HCO-. of 50 meq/liter will exhibit an average bicarbonate space of -41and 53% body wt at 30 and 90 min, respectively.
Because i[HCO-l, influenced the space of distributionof bicarbonate similarly in the metabolic and in therespiratory studies, it is axiomatic that control plasma
874 H. J. Adrogue', J. Brensilver, J. J. Cohen, and N. E. Madias
0 25k
0 20-
0 '15
0.10-
0051
IL I

TABLE IIIChanges in Urinary Bicarbonate Excretion following Administration of Sodium Bicarbonate to Dogs
with Various States of Chronic Acid-Base Equilibrium
Normal Chronic metabolic acidosis Chronic metabx)lic alkalosis Chronic respirators alkalosis Chronic respiratory aci&osis(n =4) (n = 15) (n = 17) (n = 8) (n = 9)
(Con- 30 60 90 Con- .30 60 90 Con- 30 60 90 (Co- 30 6(0 90 (Con- 30 60 9()trot min min min trol mil min mill trot min mill min trot mill mill mill trot mill nin niii
Bicarbonate 0 300 194 118 0 10 2 0 6 334 223 134 0 215 124 64 4 404 249 1 :36excretion ±0 3 ±83.3 ±38.1 ±28.4 ±0 ±4.7 ±0.9 ±0.1 ±2 3 ±266 ±166 ±139 ±0 ±21.6 ±9.8 ±9.1 ±12 ±364 ±229 ±10 4
(seq/ min)
(Cumulative 16.4 25.5 31.0 0 4 0.5 03 17.8 28.0 35.0 11.4 17.( 20 0 23 8 36 4 4:3.3bicaronate ±33 ±4.4 ±5.4 ±0 2 ±0.2 ±0.2 ±1.1 ±135 ±1.9 ±1 2 ±16 ±1.9 ±14 ±2.2 ±2.3excretion.percentage ofadlministered
Valtues represent the means± 1 SE.
pH was not of overriding importance. Indeed, as in-dicated in Figs. 3 and 4, a significant negative cor-relation between the space of distribution of bicar-bonate and the initial plasma pH was observed in themetabolic studies and a significant positive correlationwas observed in the respiratory studies.
As is evident from the similarity of ECF measure-ments among the groups and the marked influence ofi[HCO-L on the apparent space of distribution for bi-carbonate, a much greater fraction of retained bicar-bonate disappeared from the extracellular fluid in an-imals with low as compared with high initial extra-cellular bicarbonate concentrations; as shown in Fig.5, when pooled data from all five groups were analyzedat each time interval, a significant inverse relationshipwas observed between i[HCOjL and the percentage ofretained bicarbonate not found freely dissolved in theECF. Based on the relationship depicted in Fig. 5, onecan calculate that animals with an i[HCO-L of 10 meq/liter, whether of respiratory or of metabolic origin,will dissipate approximately two-thirds of retainedbicarbonate outside of the ECF space by 30 min; atthe opposite extreme, in animals with an qHCO]L of50 meq/liter, only approximately one-third of the re-tained bicarbonate will have disappeared from theECF by 30 min. As is evident from Table IV, most ofthe bicarbonate not remaining freely dissolved in theECF volume was removed by the "intracellular com-partment." As was the case for the non-ECF bicar-bonate as a whole (Fig. 5), "intracellular" bufferingcontributed more to the dissipation of retained bicar-bonate in animals with hypobicarbonatemia (whetheracidemic or alkalemic) than it did in those with hy-perbicarbonatemia. In animals with an i[HCO4L of 10meq/liter, whether of respiratory or metabolic origin,-40% of the bicarbonate retained at 30 min would
be expected to enter the "intracellular" compartment.
By contrast, only -25% would be expected to do soin animals with an i[HCO-L of 50 meq/liter. Fig. 5 alsoillustrates that, as time elapses following bicarbonateinfusion, a progressively larger fraction of retainedbicarbonate disappeared from the ECF.
DISCUSSION
This study demonstrates that the internal distributionof an acute alkali load is critically dependent on theinitial level of plasma bicarbonate concentration,rather than on the prevailing pH. Hypobicarbona-temic animals, whether acidemic or alkalemic, exhib-ited a much larger apparent space of distribution foradministered bicarbonate than did hyperbicarbona-temic animals. The second major finding, scarcely em-phasized in previous studies of bicarbonate loading(2, 5, 6), is that the response to acute bicarbonate in-fusion is a highly dynamic one, characterized at alllevels of initial plasma bicarbonate concentration bya continuous and rapid disappearance of retained basefrom the extracellular compartment. As a conse-quence, the apparent space of distribution for admin-istered bicarbonate increases progressively for at leastan hour or two after infusion and, hence, cannot mean-ingfully be assigned a single value, even at a givenbicarbonate concentration.
Before elaborating on the major conclusions of thisstudy, two important methodologic differences be-tween this and previous investigations of acute bicar-bonate loading deserve comment. The first involvesthe animal preparation used. Previous workers haveutilized bilateral nephrectomy or ureteral ligation toobviate the loss of administered bicarbonate (2, 5, 6).Wechose to avoid the anesthesia and surgical traumainvolved in this approach in the belief that more mean-ingful data could be obtained from studying intact
Bicarbonate Space in Chronic Acid-Base Disturbances 875

,. C, C
* +5+ + +5+1 +1+I+1
In 0. n
S .> E e Tl - T °$+1 - +1 +°+°+-+i +1$$
0.O*- X- t- C* 0*tt- s _ CXI= -1C:1 C C6O Ci 00 Ci 00 0 00 -0 -0X+l +l +1 +1 +l +l +1 +1 +1
> :S: _ - - 11 $- O-C 1 -C-I - - t 0-> e
.1~. c o _0o oo -0o 0000jo o -0 o 0c<_+l +1 +l +5 +1 +l +1 +l +l
o. t- C,1 -C_
+ +_ +_ +_ +X +_ + +- +M 51-r Neq-r
- t+5 +5l +5+i +5+5$c T+Ti - +i +TOo _
X.CIO_ ~-- 0o C--0 C" 8-0C, N115 c 55+5 6 6o+5 + j +o +j o +_+5+5 +5 +5 +551~-
to_= +l +l +l +l +l +l +l +l +l
- C'1C'I 11>0 - I111>1 CC C, Ir C 01 ic CR
o.=°. C, o t-. _ - - -0 0 COc
+5 +5 +5 +5 +5 +5 +5 +5 +5
0 C
< t _ _- MCI 001 PC'O 1t 0 ~ O1 011>O 0t- 1-=11 155 0 t$ - $i ° 1Ti --l 11>$i o$ i $i $
+5+5 +5 +5 +5 +5 +5 +5 +5
,0 _M_8tMMXM0 CCI 1-~ X
.t X115 c t 6 N o 6 6N or o C,oN
Co Zo. +l +l +l +l +l +l +l +l +lbr . , v~ C'- 1>10 1>D * - X - _ Ct I__CC 0-
_EoNC 5 + o5 6 6 6 - + +
+l +l +i +l +1 +C +l +l +l
R_ E X, e X - ._ N v e X_o- X.5K _ x N; ._
0 & E e $ $ $ $ $ Tl $i +
3 Z eM: $~~~1 $+ +1 o +1 +1 +1 +1
£C6C5~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~+
x~~~~~~+ +1 +i >$ j>i 1 +-i1 $ -e
_ ~ ~~~~~~~~;, r ,c t- X -.
*ctI | _ ' X _ - *- 4'in - = _ |
z_:r.X _
876 H. J. Adrogue', J. Brensilver, J. J. Cohen, and N. E. Madias

0
o
.
00
* 0
0 *
toA -
.0
30 min
I I I
10 20 30 40 50 10
Initial Extrocellulormeq / liter
90min
60 min
30 min
20;[ HCOS]
30 40 50
FiCuRE 2 Relationship between initial extracellular bicarbonate concentration and apparentbicarbonate space following sodium bicarbonate infusion. The left-hand panel depicts the re-
lationship at 30 min after infusion. Filled circles denote values obtained in dogs with metabolicacid-base disturbances, open circles, values in dogs with respiratory acid-base disturbances, andfilled triangles, values in dogs with normal acid-base status. The pooled data are best described
244.3
by the hyperbolic function, y =- + 35.9 (r = 0.726). The right-hand panel compares thex
relationship at 30 min with those obtained at 60 min =- + 42.4, r = 0.570) and 90 min
9y=11+ 47.3, r = 0.417) after the infusion. The intercepts of these relationships are signif-
icantly different from each other. The slope of each relationship is significantly different fromzero.
dogs in optimal physiologic condition. The advantagesinherent in using an intact animal model in such stud-ies are self-evident. One bit of tangible evidence ofthis advantage may be found in the apparent stabilityof plasma organic acid concentration in our animalsas compared with the significant increase observed inprevious studies (2, 5). The disadvantage to studyinganimals with intact renal function was that a variableportion of the infused base was excreted during theperiod of study; as a consequence, the actual amountof retained bicarbonate upon which our estimates ofinternal distribution are based differed significantly
among the various groups. Considering all five studygroups and all three points of observation, the average
amount of retained bicarbonate ranged between 2.8and 4.9 meq/kg body wt (Table IV). Such differencesby themselves, however, do not appear to influencethe proportion of newly assimilated bicarbonate thatundergoes a particular fate in normal animals; pre-
vious investigators have found a virtually identicalpattern of internal distribution of alkali during theacute administration of as little as 2 to as much as 20mmol/kg body wt of sodium bicarbonate in intacthumans (3) and in animals with interrupted renal func-
Bicarbonate Space in Chronic Acid-Base Disturbances
80
70_
601_
501-
ko4o
V%)
t)
401_
301_
IAL
877

0
0
0
A
A
0
0
30 mini
I I I I
7.30 7.50
90 min
60 min
30 min
IA I I I I I-ye 7.30 7.50
Initial Plasma pHFI(;URE 3 Relationship between initial plasma pH and apparent bicarbonate space followingsodium bicarbonate infusion in animals with metabolic acidosis and metabolic alkalosis (filledcircles) and in animals with normal acid-base status (filled triangles). The left-hand paneldepicts the relationship at 30 min after infusion. The least squares regression line drawn throughthe data conforms to the equation y = -43.2x + 365.9 (r = -0.748). The right-hand panel com-
pares the relationship at 30 min with those obtained at 60 min (y = -43.Lx + 370.7, r = -0.602)and 90 min (y = -50.Ox + 429.2, r = -0.409) after the infusion. The intercepts of theserelationships are significantly different from each other. The slope of each relationship is sig-nificantly different from zero.
tion (2). In addition to excreting a variable fractionof the administered alkali load, our intact animals alsohad the potential for augmenting the amount of re-
tained bicarbonate by continuing to excrete urinarynet acid. On the one hand, this effect was almost cer-
tainly negligible in animals that manifested significantbicarbonaturia (i.e., all but the metabolic acidosisgroup) because net acid excretion was fully suppressed.On the other hand, to the extent that animals withpreinfusion metabolic acidosis continued to excrete netacid following alkali infusion, the apparent space ofdistribution for administered bicarbonate would beeven larger than that indicated by our calculations.
A second major methodologic difference betweenour studies and previous reports is that we correctedour data for the influence of changes in PaCO2 ratherthan attempting to obviate the mild hypercapnia that
naturally accompanies alkali infusion. To establish theincrement in bicarbonate concentration producedsolely by the direct effects of a given alkali load, some
means must be used to eliminate the "contaminating"influence of any concomitant alteration in PaCO2; thisis true because bicarbonate concentration is unavoid-ably affected by acute changes in carbonic acid con-
centration through titration of nonbicarbonate buffers(21). Previous investigators have attempted to preventchanges in PaCO2through the use of mechanical ven-
tilation, using either general anesthesia or muscle re-
laxation or both (5, 6). Although theoretically accept-able, this procedure for stabilizing PaCO2 followingbicarbonate infusion has not proven to be very reliablein practice; indeed, sizeable increments as well as dec-rements in PaCO2have been reported and no consid-eration has been given to the possible effects of these
878 H. J. Adrogue, J. Brensilver, J. J. Cohen, and N. E. Madias
70
00
060 F0
50s_tj
(6
9)q.401_
30_
JA-I
7.10IL
L
S _ram L

90 min
60 min
30 min
I . I I I I I I
1o 7.20Initial Plasma pH
7.30 7.40
FI(xRE 4 Relationship between initial plasma pH and apparent bicarbonate space followingsodium bicarbonate infusion in animals with respiratory acidosis and respiratory alkalosis (opencircles) and animals with normal acid-base status (filled triangles). The left-hand panel depictsthe relationship at 30 min after infusion. The least squares regression line drawn through thedata conforms to the equation y = 71.8x - 480.0 (r = 0.608). The right-hand panel comparesthe relationship at 30 min with those obtained at 60 min (y = 79.5x - 529.7, r = 0.507) and90 min (y = 113.8x - 775.7, r = 0.493) after the infusion. The intercepts of these relationshipsare significantly different from each other and the slope of each relationship is significantlydifferent from zero.
changes in PaCO2 on the observed levels of plasmabicarbonate concentration (5, 6). In the current study,we allowed our animals to breathe spontaneously, thusavoiding the uncertain effects of anesthesia as well as
the stresses associated with mechanical ventilation; indoing so, a small but significant increase in PaCO2 of3-6 mmHgwas observed following bicarbonate in-fusion in all but the respiratory acidosis group (TableII). The effects of these changes in PaCO2 on plasmabicarbonate concentration were then discounted dur-ing data analysis; to do this, we used correction factorsobtained from acute carbon dioxide titration studiescarried out over an identical PaCO2 range in animalswith experimental acid-base disturbances identical to
those used here (22, 23). Webelieve this approach to
eliminating the unwanted effects of increments inPaCO2 is equally sound on theoretic grounds and
avoids the many pitfalls of controlled ventilation. Atmost, the required correction resulted in a downwardadjustment in plasma bicarbonate concentration of 1.3meq/liter. Although a truly accurate representationof the internal distribution of administered alkali musttake proper cognizance of this small effect of second-ary hypercapnia, it is noteworthy that an analysisbased on the uncorrected data for extracellular bicar-bonate yielded identical overall conclusions.
A major finding of this study is that the initial ex-
tracellular bicarbonate concentration exerts a strikinginfluence on the apparent space of distribution foradministered bicarbonate. What accounts for this ef-fect? One theoretic possibility is that this influencemight have reflected sizeable differences in the "ana-tomic" portion of the bicarbonate space, that is, in theactual volume of the ECF. This possibility is clearly
Bicarbonate Space in Chronic Acid-Base Disturbances
70
60
00
0
0
50_
0
k
q)
no
4..
q)
4ox
t3
tbl
0
0
"O
0
A
A
A
40kOo
0
30k
30min
I I I I IJ L A a I7.7.20 7.30 7.4
I I I I I --ILIIA--L.... I 'If A i
879

@0a 0
0
O'00i.- 0o. 4
A
301_0 So
30 min
I -1I I I
10 20 30 40 50 0 10Initial Extracellulor
90 min
60 min
30 min
I I I I I
20 30
[HCOf]40 50
meq/liter
FIGURE 5 Relationship between initial extracellular bicarbonate concentration and the fractionof retained bicarbonate that disappeared from the ECF following sodium bicarbonate infusion.The left-hand panel depicts the relationship at 30 min after infusion. Filled circles denotevalues obtained in dogs with metabolic acidosis and metabolic alkalosis. Open circles denotevalues obtained in dogs with respiratory acidosis and respiratory alkalosis. Filled trianglesdenote values obtained in dogs with normal acid-base status. The pooled data were best de-
259.5scribed by the hyperbolic function, y = + 28.1 (r = 0.660). The right-hand panel compares
x
the relationship at 30 min with those obtained at 60 min y 1= + 42.3, r = 0.416) and 90
min = + 49.4, r = 0.354) after the infusion. The intercepts of these relationships are
significantly different from each other. The slope of each relationship is significantly differentfrom zero.
excluded by the present study. Radiosulfate measure-
ments and chloride space arithmetic indicate that hy-pobicarbonatemic animals had neither a larger initialECF volume nor a larger increment in extracellularvolume following the acute infusion to account fortheir larger bicarbonate space. Maximal differences inextracellular volume between hypo- and hyperbicar-bonatemic animals did not exceed 4% of body wt atany time during the experiments, whereas the con-
comitant differences in apparent space of distributionfor bicarbonate were -20% of body wt.
Thus, the influence of initial extracellular bicarbon-ate concentration on the apparent space of distributionof bicarbonate must have been a manifestation largelyof variable bicarbonate removal from the extracellularcompartment. Why did hypobicarbonatemic animals
transfer a larger fraction of retained bicarbonate outof the extracellular compartment than did normal or
hyperbicarbonatemic animals? Previous studies, inwhich alterations in plasma bicarbonate concentrationwere induced solely by metabolic acid-base derange-ments, also detected an enlargement of bicarbonatespace in the presence of hypobicarbonatemia (5, 6).The explanation advanced was that the associatedacidemia was the critical determinant of the altereddistribution of administered base; it was reasoned thatanimals with metabolic acidosis were poised to dissi-pate (through intracellular and extracellular buff er-
ing) an abnormally large fraction of administered bi-carbonate because of the large burden of hydrogenions sequestered on nonbicarbonate buffers as pH fellduring induction of the basal acidosis (5, 6). It is clear
880 H. J. Adrogue, J. Brensilver, J. J. Cohen, and N. E. Madias
80 K
601-
50 F0 40 _
ctq)
CZ
IC:
t3j
'%3'3
201_
lo-
0
70 _

from the present study that this interpretation is notvalid. Animals with comparably low levels of extra-cellular bicarbonate concentration but with alkalemiarather than acidemia (i.e., chronic respiratory alkalosisrather than metabolic acidosis) exhibited comparableenlargements of the apparent bicarbonate space. Ifanything, such animals would probably experience areduction in the amount of hydrogen ion sequesteredin the buffer pool during their response to prolongedhypocapnia.
The data from this study indicate that the criticalfactor accounting for the influence of initial plasmabicarbonate concentration on the internal distributionof alkali is the change in pH induced by acute alkaliloading, rather than the prevailing pH at the onset ofthe infusion. In obeying the constraints of the Hen-derson-Hasselbalch equation, animals with hypobicar-bonatemia for whatever reason will experience a largerchange in pH in response to a given increment inplasma bicarbonate than will normal or hyperbicar-bonatemic animals. In our experiments, the mean in-crement in plasma bicarbonate concentration pro-
30 min
duced by the infusion protocol was remarkably similarin all five groups (Table II). This similarity reflects thefact that animals with smaller bicarbonate spaces (i.e.,those in the hyperbicarbonatemic groups) retained asmaller fraction of the administered base during theperiod of observation than did animals with largerbicarbonate spaces. In any event, the complex set ofinteracting factors that determined the observed in-crement in bicarbonate concentration culminated ina striking inverse correlation between the initial levelof plasma bicarbonate and the change in pH (Fig. 1);on average, animals with low bicarbonate levels ex-perienced a shift in pH at least 0.10 U greater thanthose with normal or elevated levels.
Given this inverse correlation and given the likeli-hood that changes in extracellular pH are accompaniedby roughly proportional shifts in intracellular pH (30-32), it seems reasonable to hypothesize that the ob-served differences in the apparent space of distributionfor administered base resulted from the widely dif-ferent range of pH over which nonbicarbonate bufferswere titrated in the various states of acid-base equi-
60 min 90 min
4
Q
'4..3
CZ'b
2t ,.%
*q
0.05 0.10 0.15 0.20 0.25
* 00 9
0 .00
o0o 00 0.l 0.0.2
0 * 0. 0
0
A A
I I I I
0.05 0.10 0.15 0.20 0.25
A Plasma pHc
S
-. 0~~ 0
,S9
0 -0 ~~~0
00
A
0.05 0.10 0.15 0.20
FI(;URE 6 Relationship between change in plasma pH and amount of retained bicarbonate thatdisappeared from the ECF after sodium bicarbonate infusion. Experimental values for plasmapH were calculated from the corrected plasma [HCO3] and the preinfusion PaCO2 (Methods).The left-hand, middle and right-hand panels depict the relationship at 30, 60, and 90 min afterinfusion, respectively. Filled circles denote values obtained in dogs with metabolic acidosis andmetabolic alkalosis. Open circles denote values obtained in dogs with respiratory acidosis andrespiratory alkalosis. Filled triangles denote values obtained in dogs with normal acid-basestatus. The least squares regression lines drawn through the data conform to the equations,y = 7.16x + 0.78, r = 0.719 (30 min), y = 7.61x + 1.07, r = 0.735 (60 min) and y = 8.57x+ 1.21, r = 0.696 (90 min). The intercepts of these relationships are significantly different fromeach other and the slope of each relationship is significantly different from zero.
Bicarbonate Space in Chronic Acid-Base Disturbances
* METABOLICo RESPIRATORYA NORMAL
0o 0 0
000
0 00
. 00A 010 0
0 * A .0
0**a0 00.0
I I a I I
4
3
2
0.25
a
I
881

librium studied.5 If the aggregate buffer value of non-bicarbonate buffers is constant over the range of pHinduced in the present study groups,6 this hypothesiswould predict a linear relationship between the ob-served change in plasma pH and the quantity of bi-carbonate that disappeared from the extracellularcompartment in each of the circumstances examined.As shown in Fig. 6, pooled data from all experimentsanalyzed in this fashion reveals just such a linear cor-relation for each of the three points of observation.
Fig. 6 also illustrates the second major finding ofthis study, namely the striking time dependence of thebuffering response; over each 30-min interval follow-ing infusion, progressively more retained bicarbonatewas dissipated by buffering for a given change in pH.The calculations upon which this conclusion is basedcannot distinguish between ongoing production of en-dogenous acid and slowly equilibrating buffer stores(34, 35). However, if one assumes that endogenous acidproduction continued at rates typically observed fordogs ingesting the diets used in this study (8), <0.2meq/kg body wt of administered alkali would havebeen consumed by this process over the entire 90-minperiod of study.
Slow equilibration of tissue buffers was, of course,manifestly present in animals with metabolic acidosisin which virtually none of the infused bicarbonate wasexcreted but in which plasma bicarbonate fell pro-gressively from its peak value at 30 min (Table II).For each of the other groups, in which appreciableexcretion of administered bicarbonate did occur, closeanalysis of Fig. 6 reveals that slow equilibration oftissue buffers contributed importantly to the continueddissipation of infused base and, hence, contributed tothe postinfusion decline in plasma bicarbonate. Thisstudy sheds no light on the precise location(s) at whichslow equilibration of nonbicarbonate buffers takesplace. Bone is obviously an attractive candidate forsuch a sluggish response. Indeed previous investigatorshave demonstrated that bone buffers do begin to par-ticipate importantly in dissipating administered bi-carbonate within the intervals examined here (27).
The erythrocythemia characteristic of animals with hy-poxia-induced respiratory alkalosis did contribute in smallpart to the larger apparent space of distribution of bicar-bonate. However, even if one discounts this effect, animalswith chronic respiratory alkalosis would still feature a largerapparent bicarbonate space than did animals with chronicrespiratory acidosis.
6 The buffer value of hemoglobin and plasma proteins ofnormal subjects is stable over the physiologic range of pH(24). Moreover, the buffer value of plasma proteins is notsignificantly different in chronic metabolic acidosis as com-pared with chronic metabolic alkalosis (33). There are nodata on the buffer value of tissue nonbicarbonate buffersduring chronic alterations in acid-base equilibrium.
ACKNOWLEDGMENTSThis study was supported in part by grants HL-00759 andHL-15810 from the National Heart, Lung, and Blood Insti-tute and AM-07078 from the National Institute of Arthritis,Metabolism, and Digestive Diseases and by funds from theAmerican Heart Association, Massachusetts Affiliate.
REFERENCES
1. Swan, R. L., and R. F. Pitts. 1955. Neutralization ofinfused acid by nephrectomized dogs. J. Clin. Invest.34: 205-212.
2. Swan, R. C., D. R. Axelrod, M. Seip, and ft. F. Pitts.1955. Distribution of sodium bicarbonate infused intonephrectomized dogs. J. Clin. Invest. 34: 1795-1801.
3. Singer, R. B., J. K. Clark, E. S. Barker, A. P. Crosley,Jr., and J. R. Elkinton. 1955. The acute effects in manof rapid intravenous infusion of hypertonic sodium bi-carbonate solution. I. Changes in acid-base balance anddistribution of the excess buffer base. Medicine (Balti-more). 34: 51-95.
4. Schwartz, W. B., K. J. Orning, and R. Porter. 1957. Theinternal distribution of hydrogen ions with varying de-grees of metabolic acidosis. J. Clin. Invest. 3: 373-382.
5. Russell, C. D., M. M. Illickal, J. V. Maloney, Jr., H. D.Roeher, and E. C. DeLand. 1972. Acute response to acid-base stress in the dog. Am. J. Physiol. 223: 689-694.
6. Garella, S., C. L. Dana, and J. A. Chazan. 1973. Severityof metabolic acidosis as a determinant of bicarbonaterequirements. N. Engl. J. Med. 289: 121-126.
7. Palmer, W. W., and D. D. Van Slyke. 1917. Relationshipbetween alkali retention and alkali reserve in normaland pathological individuals. J. Biol. Chem. 32: 499-507.
8. Polak, A., G. D. Haynie, R. M. Hays, and W. B.Schwartz. 1961. Effects of chronic hypercapnia on elec-trolyte and acid-base equilibrium. I. Adaptation. J. Clin.Invest. 40: 1223-1237.
9. DeSousa, R. C., J. T. Harrington, E. S. Ricanati, J. W.Shelkrot, and W. B. Schwartz. 1974. Renal regulationof acid-base equilibrium during chronic administrationof mineral acid. J. Clin. Invest. 53: 465-476.
10. Schwartz, W. B., and L. Silverman. 1965. A large en-vironmental chamber for the study of hypercapnia andhypoxia. J. Appl. Physiol. 20: 767-774.
11. Gennari, F. J., M. B. Goldstein, and W. B. Schwartz.1972. The nature of the renal adaptation to chronic hy-pocapnia. J. Clin. Invest. 51: 1722-1730.
12. Tannen, R. L., H. L. Bleich, and W. B. Schwartz. 1966.The renal response to acid loads in metabolic alkalosis;an assessment of the mechanisms regulating acid excre-tion. J. Clin. Invest. 45: 562-572.
13. Goldstein, M. B., F. J. Gennari, and W. B. Schwartz.1971. The influence of graded degrees of chronic hy-percapnia on the acute carbon dioxide titration curve.J. Clin. Invest. 50: 208-216.
14. Severinghaus, J. W., M. Stupfel, and A. F. Bradley. 1956.Accuracy of blood pH and pCO2determinations. J. Appl.Physiol. 9: 189-196.
15. Severinghaus, J. W., M. Stupfel, and A. F. Bradley. 1956.Variations of serum carbonic acid pK' with pH and tem-perature. J. Appl. Physiol. 9: 197-200.
16. Rosenthal, T. B. 1948. The effect of temperature on thepH of blood and plasma in vitro. J. Biol. Chem. 173:25-30.
882 H. J. Adrogue, J. Brensilver, J. J. Cohen, and N. E. Madias

17. Rubini, M. E., and A. V. Wolf. 1957. Refractometricdetermination of total solids and water of serum andurine. J. Biol. Chem. 225: 869-876.
18. Elkinton, J. R., and T. S. Danowsky. 1955. The BodyFluids. The Williams & Wilkins Company, Baltimore.85.
19. Walser, M., D. W. Seldin, and A. Grollman. 1953. Anevaluation of radiosulfate for the determination of thevolume of extracellular fluid in man and dogs. J. Clin.Invest. 32: 299-311.
20. Rettori, V., T. Gral, S. G. Massry, and M. F. Villamil.1972. Exchangeable potassium content and distributionin normal subjects and uraemic patients on chronic hae-modialysis. Clin. Sci. (Lond.). 42: 673-684.
21. Giebisch, G., L. Berger, and R. F. Pitts. 1955. The extra-renal response to acute acid-base disturbances of respi-ratory origin. J. Clin. Invest. 34: 231-245.
22. Madias, N. E., H. J. Adrogue, and J. J. Cohen. 1977. Theeffect of chronic metabolic acid-base disturbances on theacute "whole-body" CO2equilibration curve in the dog.Proc. Am. Soc. Nephrol. 10: 114a. (Abstr.)
23. Madias, N. E., H. J. Adrogue, F. J. Gennari, and J. J.Cohen. 1978. The effect of chronic respiratory acid-basedisturbances on the acute "whole-body" CO2 titrationcurve in the dog. Proc. Int. Congr. Nephrol. 7: H-2a.(Abstr.)
24. Siggaard-Andersen, 0. 1974. The Acid-Base Status ofthe Blood. The Williams & Wilkins Company, Balti-more. 41-43.
25. Dill, D. B., H. T. Edwards, and W. V. Consolazio. 1937.Blood as a physicochemical system. XI. Man at rest. J.Biol. Chem. 118: 635-648.
26. Woodbury, J. W. 1974. Body acid-base state and its reg-
ulation. In Physiology and Biophysics. T. C. Ruch andH. D. Patton, editors. Vol. II. Circulation, Respiration,and Fluid Balance. 20th edition. W. B. Saunders Co.,Philadelphia. 480-524.
27. Burnell, J. M. 1968. In vivo response of muscle tochanges in CO2tension or extracellular bicarbonate. Am.J. Physiol. 215: 1376-1383.
28. Adrogue, H. J., J. Brensilver, and N. E. Madias. 1978.Changes in the plasma anion gap during chronic met-abolic acid-base disturbances. Am. J. Physiol. 235:F291-F297.
29. Madias, N. E., J. C. Ayus, and H. J. Adrogue. 1979.Increased anion gap in metabolic alkalosis: the role ofplasma-protein equivalency. N. Engl. J. Med. 300:1421-1423.
30. Waddell, W. J., and R. G. Bates. 1969. Intracellular pH.Physiol. Rev. 49: 285-329.
31. Khuri, R. N., S. K. Agulian, and K. K. Bogharian. 1976.Intracellular bicarbonate of skeletal muscle under dif-ferent metabolic states. Am. J. Physiol. 230: 228-232.
32. Adler, S., A. Roy, and A. S. Relman. 1965. Intracellularacid-base regulation. 1. The response of muscle cells tochanges in CO2tension or extracellular bicarbonate con-centration. J. Clin. Invest. 44: 8-20.
33. Adrogue, H. J. 1979. The buffer value of the non-bi-carbonate buffers of plasma during chronic metabolicacid-base disturbances. Clin. Res. 27: 406a. (Abstr.)
34. Siesj6, B. K., and K. Messeter. 1971. Factors determiningintracellular pH. In Ion Homeostasis of the Brain. B. K.Siesj6 and S. C. Sorensen, editors. Munksgaard, Copen-hagen. 244-269.
35. Relman, A. S. 1972. Metabolic consequences of acid-basedisorders. Kidney Int. 1: 347-359.
Bicarbonate Space in Chronic Acid-Base Disturbances 883