Accuracy of current clinical diagnosis in recreational drug-related attendance to the emergency...
Transcript of Accuracy of current clinical diagnosis in recreational drug-related attendance to the emergency...

ORIGINAL RESEARCH
Accuracy of current clinical diagnosis inrecreational drug-related attendance to theemergency departmentEmma West,1 Peter Cameron,1 Gerard O’Reilly,1 Olaf H Drummer2 and Adam Bystrzycki11The Alfred Hospital, and 2Victorian Institute of Forensic Medicine, Department of Forensic Medicine,Monash University, Melbourne, Victoria, Australia
Abstract
Objective: To determine the accuracy of current clinical diagnosis in recreational drug-related atten-dances to emergency by blood analysis.
Methods: A prospective convenience sample of 103 patients who attended hospital with suspectedrecreational drug-related presentations was collected. Doctors’ clinical impression of drugsresponsible for presentation was compared with a detailed forensic blood analysis forrecreational drugs.
Results: Among 103 samples, 80 (78%, 95% confidence intervals [CI] 70–86%) were found to havecorrect clinical suspicion of the recreational drug responsible for clinical presentationconfirmed by laboratory analysis. Clinical diagnosis was most accurate for gamma-hydroxy butyrate (GHB) (sensitivity 97%, specificity 91%) and less accurate for amphet-amines (sensitivity 61%, specificity 79%), alcohol (sensitivity 42%, specificity 84%) andopiates (sensitivity 46%, specificity 100%). Multiple drug ingestion was found in 70%(95% CI 61–79%) of samples. Sensitivity and specificity of clinical impression for predic-tion of multiple drug ingestion presence is 75% (95% CI 66–83%) and 85% (95% CI78–92%), respectively.
Conclusion: Clinical diagnosis in recreational drug-related attendances to the ED was correct in mostcases. Drugs, such as GHB, were the most accurately diagnosed. Inaccuracy in recognizingother drugs, like amphetamines, opiates and alcohol, occurs where a coingestant producesa more profound clinical picture. Multiple drug ingestion is a common scenario in recre-ational drug presentations to emergency.
Key words: blood analysis, diagnosis, emergency department, recreational drug, Street drug.
Correspondence: Dr Emma West, The Alfred Hospital, Commercial Road, Melbourne, Vic. 3004, Australia. Email: [email protected]
Emma West, MB BS, Registrar; Peter Cameron, MB BS, MD, FACEM, Consultant; Gerard O’Reilly, MB BS, FACEM, Grad Cert CT, MPH,Consultant; Olaf H Drummer, B.App.Sci, PhD, ARCPA, Head Forensic and Scientific Services; Adam Bystrzycki, MB BS, FACEM, Consultant.
doi: 10.1111/j.1742-6723.2008.01110.x Emergency Medicine Australasia (2008) 20, 333–338
© 2008 The AuthorsJournal compilation © 2008 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine

Introduction
Recreational drug use is increasing1,2 and, inevitably,overdose or adverse effects necessitating medical careoccur.3 Drug-related medical attendances to the ED arecommon,4,5 and illicit or recreational drugs cause a sig-nificant proportion of these attendances.3 The patternof recreational drug use appears to be changing withincreased attendances attributed to GHB – gamma-hydroxy butyrate, and decreased attendances due toheroin.6
This change is reflected by recent case reports andcase series on GHB in Australian and International Jour-nals,7,8 although not all literature is consistent.9 GHB,a drug popular in the dance party scene, commonlycauses respiratory depression requiring airway supportin the ED. Doctors treat overdose on the basis of pre-sumed drug ingestion, with most centres not performingblood tests for recreational drugs.
There is limited evidence that presentation might berelated to ingestion of multiple recreational drugs;10,11
however, laboratory testing of drug levels has gen-erally not been available. Drugs other than GHB,including MDMA – methylenedioxymethamphetamine(street name ecstasy or XTC) and other amphetamines,cocaine, marijuana, opiates and alcohol, are suspected inthe illicit or multiple recreational drug ingestion picture.These drugs produce a clinical spectrum of presenta-tions ranging from hypertension and anxiety to stroke,respiratory depression, arrhythmias and myocardialischaemia. As a consequence, recreational drug use is acommon problem seen in the ED.3 The significant mor-bidity and mortality associated with these drugs is welldocumented.12–15
Recreational drug use can be detected in the ED byblood or urine sample analysis; however, current avail-able testing does not allow detection of GHB and thusappears incomplete given the changing pattern of rec-reational drug use. Retrospective16 and prospective17
case series describing the clinical features of GHBintoxication, coingestants and outcomes have been pub-lished, but no studies have examined the accuracy ofclinical diagnosis in suspected GHB or other recre-ational drug ingestion. Clinical history is unreliable inthe case of drug ingestion,18–20 especially in relation torecreational drugs where there is no quality control inthe manufacture of these illegal substances. Currently,as accuracy of clinical diagnosis of patterns associatedwith specific recreational drugs is unknown, laboratoryanalysis is required in the setting of suspected drugingestion. Our study compares clinical impression
regarding type of drugs used and frequency of multipledrug ingestion with laboratory confirmed drug pres-ence, including GHB.
Methods
The present study was conducted at the ED of theAlfred Hospital, Melbourne, Victoria, Australia betweenOctober 2004 and July 2005. The hospital is an adult,urban, tertiary referral centre with annual ED census ofapproximately 40 000 patients per year. It is an inner-city hospital in close proximity to many all-hours’ night-life venues.
Hospital Ethics Committee approval as a qualityimprovement project was obtained.
The study was a prospective observational study of aconvenience sample of emergency patients suspectedclinically of recreational drug use. Recreational drugswere defined as amphetamines (including MDMA,methamphetamine and other related compounds),cocaine, cannabis, GHB, ketamine, heroin and otheropiates, hallucinogens, benzodiazepines and alcohol.
All patients presenting to our hospital ED between 1January 2004 and 31 June 2005 were eligible for thestudy. Doctors and nurses were asked to includepatients suspected of having a recreational drug-relatedpresentation to the ED. Overdose presentations whererecreational drugs were not suspected were notincluded. Attendances related to alcohol use where otherrecreational drug use was suspected were included.Patients having blood tests performed for investigationof their presentation were included in the study pro-vided that an additional de-identified sample wascollected for complete analysis for recreational drugpresence.
Enrolled patients were assigned a study pack, whichincluded de-identified forms, a blood sample collectiontube and a study information sheet. The treating doctorcompleted documentation at the end of the clinicalassessment. Information documented included demo-graphic details, time of assessment, time of study bloodtest, clinical features reflecting the assessment andreason for enrolment in the study. Based on clinicalassessment, the doctor was asked to document the likelydrug or drugs responsible for the attendance to emer-gency and whether the attendance was multiple drugingestion-related. Multiple drug ingestion was definedas more than one recreational drug being responsible forthe presentation. Amphetamines (including metham-phetamine and MDMA) were considered as one group.
E West et al.
334 © 2008 The AuthorsJournal compilation © 2008 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine

The doctor was instructed to make the diagnosis onthe basis of clinical information at the completion of theexamination without reference to laboratory results.Time of assessment and blood test were recorded toensure that clinical assessment could be correlated withserum levels at the time the assessment was made.
All de-identified blood samples were sent for detailedforensic laboratory analysis for recreational drugs to theVictorian Institute of Forensic Medicine (VIFM). Theseresults were not available to treating clinicians at thetime of the assessment. Administration of any thera-peutic agent (e.g. induction drugs for intubation orsedatives for agitation) were recorded to avoid falserepresentation as recreational drugs in drug analysis.
Analysis
The 10 mL de-identified sample of blood collected wasanalysed by the VIFM toxicology section as follows;Opiates by enzyme-linked immunosorbent assay.Common drugs and poisons, including the recreationaldrugs – amphetamines (MDMA, methamphetamine andrelated drug compounds), ketamine, cocaine, benzodiaz-epines and codeine – were measured by gas chromato-graphy and mass spectrometer. Drug screen alsoincluded antidepressants, antipsychotics, many cardio-vascular drugs, GHB and other opiates, includingcodeine and methadone. All drug concentrations were inmg/L. Alcohol and cannabis were tested in the labora-tory of the Alfred Hospital at the discretion of the treat-ing doctor.
Statistics
Clinical diagnosis was compared with laboratoryresults to determine accuracy of clinical assessments.Correct diagnosis was assigned if one or more of thedrugs indicated by doctors were present on bloodtesting. If the analysis and doctor both indicated mul-tiple drug ingestion, the clinical impression was posi-tive. The results are expressed as a percentage with95% confidence intervals (CI). The sensitivity, specific-ity and likelihood ratios of a clinical impression for theprediction of drug presence confirmed by blood testingwere calculated.
Results
The study included 107 subjects suspected of having arecreational drug-related presentation to the ED. Four
samples had incomplete paper work and were notincluded, leaving a sample size of 103. All subjects witha completed study information pack and an additionalblood sample for recreational drug analysis wereeligible for inclusion in the study. Doctors seeing thepatients enrolled were predominately emergency regis-trars (91%) and otherwise consultants (6%) or residentmedical staff (3%). The median age was 23.5 with amean of 25 and a range of 15–50 years of age. Amongthem, 57% (n = 59) were male and 43% (n = 44) female.
Doctors recorded one drug or one drug plus alcohol asresponsible for the presentation in 87/103 (84%) ofsamples. Two drugs were recorded in 11/103 (11%) – 9of these cases recorded the combination of GHB andan amphetamine. Four of the one hundred and threesamples had drug unknown recorded and one indictedthree drugs.
Eighty out of the one hundred and three (78%, 95%CI 70–86%) samples were found to have a correct clini-cal impression of the drug responsible for the majorclinical effect confirmed by laboratory analysis. Table 1shows data for the four most common drugs detected.The sensitivity, specificity and likelihood ratios of aclinical impression for the prediction of drug presenceconfirmed by blood testing are shown. In all caseswhere GHB was clinically suspected but not found ontesting, the patient presented with depressed consciousstate. Amphetamines were not clinically suspected in 25cases, where blood testing confirmed their presence.Twenty out of twenty-five missed diagnosis for amphet-amines occurred in the setting of GHB ingestion. Theadjusted sensitivity for amphetamine diagnosis insamples with no GHB was 39/44 = 89%.
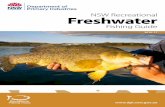
Figure 1 shows the percentage of samples containingeach recreational drug tested for. All samples were
Table 1. Data for the four most common drugs detected
Drug bloodresult
Clinicalsuspicion
Sensitivity (%)specificity (%)
Positive LRnegative LR
+ -GHB + 29 1 97 10.8
- 6 67 91 0.03Amphetamine + 39 25 61 2.9
- 8 31 79 0.49Alcohol + 20 27 42 2.6
- 7 37 84 0.7Opiates + 6 7 46 -
- 0 90 100 0.54
Negative LR, negative likelihood ratio; positive LR, positivelikelihood ratio.
Accuracy of current clinical diagnosis
335© 2008 The AuthorsJournal compilation © 2008 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine

tested for amphetamines, GHB, opiates, benzodiaz-epines, ketamine and cocaine. Doctors did not indicateany presentations due to cannabis or hallucinogens.Alcohol was requested for testing by doctors in 91/103(89%) of samples. No hallucinogens were found ontesting. The concentration in mg/L of GHB, metham-phetamine and MDMA are displayed in Table 2. Whereconcentrations of metamphetamine or MDMA werebelow 0.1 mg/L and recorded as a positive result, theywere always in the presence of another form of am-phetamine (MDMA or metamphetamine) higher than0.1 mg/L.
Multiple drug ingestion was found in 70% (95% CI61–79%) of samples. Sensitivity and specificity of clini-cal impression for prediction of multiple drug ingestionpresence is 75% (95% CI 66–83%) and 85% (95% CI78–92%), respectively. Trends for the most common
multiple drug ingestion combinations are shown inTable 3. Ketamine was found in 5% of samples andalways in the presence of MDMA.
MDMA and methamphetamine were the mostcommon amphetamines found. Fifty-nine samplestested positive for MDMA and thirty-five for metham-phetamine. When amphetamines were found in a bloodsample, 30/64 (47%) tested positive for combination ofmethamphetamine and MDMA and 29/64 (45%) forMDMA as the only amphetamine.
Discussion
The study examines the accuracy of clinical assessmentof likely recreational drugs responsible for presentationto the ED. Numerous studies have commented on theclinical presentation and epidemiology of GHB use16,17,21
and the laboratory confirmation of drug ingestion,22,23
but few19,24 have prospectively examined accuracy ofclinical diagnosis of suspected ingestant on the basis ofclinical findings.
In the present study, the correct ED diagnosis of thedrug responsible for presentation was made in 78%(95% CI 70–86%) of cases. Our clinical impression ratewas significantly better than other ED-based studies,19
but similar to that reported by Bjornaas et al.24 whofound correct clinical evaluation in more than 75% ofcases tested for GHB, amphetamine, ecstasy (MDMA),cannabis and cocaine. The study differed from ours inthat it examined patients admitted to hospital for all-cause acute poisoning. Despite the different diagnosticsetting and purpose, the accuracy of clinical perceptionwas similar, perhaps reflecting inaccurate present-ing history and overlap between clinical syndromesbecause of similar high rates of multiple drug ingestion.
ED doctors are familiar with the clinical presentationof GHB ingestion, reflected in the high sensitivity andlikelihood ratio. Doctors are familiar with GHB causingdepressed conscious state and incorrectly attributedpresentation due to GHB in six cases of depressed con-scious state. Diagnostic accuracy for other drugs is
51
29
12 105 2
62
0
10
20
30
40
50
60
70
Amphetam
ine
ETOH
GHBOpiate
Benzodiazepine
Ketamine
Cocaine
Figure 1. Per cent samples containing each drug.
Table 2. Drug concentrations
Drug Mean concentrationin mg/L
Range ofconcentrations
in mg/L
GHB 130 18–265MDMA 0.32 0.09–1.38Methamphetamine 0.16 0.02–3.25
GHB, gamma-hydroxy butyrate; MDMA, methylenedio-xymethamphetamine.
Table 3. Common multiple ingestion combinations
Drug Found alone Multiple ingestion Most commonly found with Drug and alcohol
GHB (n = 30) 5/30 (17%) 25/30 (83%) Amphetamine 25/30 (83%) 2/30 (7%)Amphetamine
(n = 64)18/64 (28%) 46/64 (72%) Alcohol and GHB.
Other – ketamine 4/64 (6%),benzodiazepine 4/64 (6%).
22/64 (34%)
Opiate (n = 13) 2/13 (15%) 11/13 (85%) Amphetamine 6/12 (50%) 4/13 (31%)
E West et al.
336 © 2008 The AuthorsJournal compilation © 2008 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine

influenced by certain patterns of multiple drug inges-tion. Sensitivity of clinical diagnosis for amphetamineuse was low (61%) and might reflect multiple drugingestion being overlooked in the presence of GHB,which produces a profound clinical presentation ofdepressed conscious state. Sensitivity of clinical suspi-cion of amphetamine use is greatly improved whenadjusted for GHB (89%). It is not surprising that sensi-tivity for amphetamines is low as these drugs often donot cause significant clinical impairment or behaviouralchanges. As well, diagnosis of opiate use also might beinfluenced by the high rate of multiple drug ingestion(85%) – particularly with amphetamine.
Our study confirms the suspicion of recreationaldrug use in the ED setting commonly being a multipledrug ingestion picture. Seventy per cent (95% CI,61–79%) of cases with suspected recreational drug-related attendances were found to have more than onedrug present on detailed laboratory analysis. Previousstudies have also noted multiple drug ingestionscomplicating recreational drug use,10,11 although not atsuch high proportions.25
Drug-related presentation to the ED is common andreflects the frequency of drug use in the community.In 2001, 16.9% of the population in Australia aged14 years and over reported the recent use of any recre-ational drug.1 The current study reflects a changingpattern in recreational drug use, with opiate attendancesfound in 12% (95%, CI 6–18%) of presentations andamphetamines represented most frequently being foundin 62% (95%, CI 60–64%). We found GHB representedin 29% (95% CI, 20–38%) of tested specimens and cor-rectly identified 29/30 possible times. Previous studieshave documented the high rate of opiate-related atten-dances.3 Our study shows a different pattern in Austra-lia possibly because of the use of ambulance naloxoneresulting in low levels of patient transportation to hos-pital,20 along with other new recreational drugs gainingpopularity. Other studies reported detection of drugslike amphetamines and GHB most frequently, particu-larly in age groups under 30 years,6,25 a pattern reflectedin the young cohort sampled in our study.
Investigating diagnostic accuracy allows the treatingphysician to recognize error rates relying on historyand examination alone and consider the common andcomplex picture of a multiple ingestion overdose.Studies such as ours have an important role not only inindividual patient care, but also in prompting publichealth campaigns to alert the community of the risksassociated with recreational drug use and confirm theharmful nature of these drugs.
Limitations
We identify a number of limitations related to potentialselection bias. Doctors and nurses were asked to enrollpatients with suspected recreational drug-related presen-tations and it is likely that more severe presentationswere enrolled and younger patients considered morelikely to have a recreational drug-related attendance.Information of cases not suspected as recreational drug-related presentations was not collected. The location ofthe hospital close to a number of all-hours venues fre-quented by people under 30 years of age might lead to anoverrepresentation of this age group, although our agerange is in-keeping with multiple previous studies.6,26
GHB was present in the lay media on frequent occa-sions during the study period, perhaps increasing thelikelihood of doctors recognizing this as a recreationaldrug presentation. It is more likely, however, that mediareports reflected the increased use of the drug and thismight explain its high representation in the studysample.
Finally, we acknowledge that detection of a drugon laboratory analysis does not definitively prove thatthe drug was responsible for the presentation. Somepatients might have low concentrations of drug detectedthat might not be clinically significant. However, thispoint does not significantly detract from the high diag-nostic accuracy noted in our study.
Conclusion
Clinical diagnosis in recreational drug-related atten-dance to the ED was correct in most cases. Drugs pro-ducing significant morbidity, like GHB, are the mostaccurately diagnosed. Inaccuracy in recognizing otherdrugs, like amphetamines, opiates and alcohol, occurswhere a coingestant produces a more profound clinicalpicture. Multiple drug ingestion is a common scenario inrecreational drug presentations to emergency.
Acknowledgements
Dimitri Gerostamoulos and Jessica Wood – VIFM. DrMichael Bailey – Department of Epidemiology and Pre-ventive Medicine, The Alfred Hospital.
Competing interests
None declared.
Accepted 11 June 2008
Accuracy of current clinical diagnosis
337© 2008 The AuthorsJournal compilation © 2008 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine

References
1. Australian Institute of Health and Welfare. Statistics on drug usein Australia 2002. Australian Institute of Health and Welfare,Canberra, 2003, p 113. Available from URL: http://www.aihw.gov.au/publications/
2. Maxwell JC. Update: comparison of drug use in Australia and theUnited States as seen in the 2001 National Household Surveys.Drug Alcohol Rev. 2003; 22: 347–57.
3. Gibbs T, Ross L. Illicit drug use related attendances at accidentand emergency services in Aberdeen: a prospective six-monthsurvey. Health Bull. (Edinb). 2000; 58: 170–6.
4. Drug-related problems in London accident and emergencydepartments. A twelve-month survey. Lancet 1981; 2: 859–62.
5. Stanton LA, Peterson GM, Rumble RH et al. Drug related admis-sions to an Australian hospital. J. Clin. Pharm. Ther. 1994; 19:341–7.
6. Miro O, Nogue S, Espinosa G et al. Trends in illicit drug emer-gencies: the emerging role of gamma-hydroxybutyrate. J. Toxicol.Clin. Toxicol. 2002; 40: 129–55.
7. Li J, Stokes S, Woeckener A. A tale of novel intoxication: sevencases of gamma-hydroxybutyric acid overdose. Ann. Emerg.Med. 1998; 31: 723–8.
8. Haraway S., Stephenson L. GHB: intoxication: the Gold Coastexperience. Emerg. Med. 1999; 11: 45–8.
9. Anderson IB, Kim SY, Dyer JE et al. Trends in gamma-hydroxybutyrate (GHB) and related drug intoxication: 1999–2003. Ann. Emerg. Med. 2006; 47: 177–83.
10. Quinn DI, Wodak A, Day RO. Pharmacokinetic and Pharmaco-dynamic principles of illicit drug use and treatment of illicit drugusers. Clin. Pharmacokinet. 1997; 33: 344–400.
11. Zhao. H, Brenneisen R, Scholer A et al. Profiles of urine samplestaken from ecstasy users at rave parties: analysis by immunoas-says, HPLC, and GC-MS. J. Anal. Toxicol. 2001; 25: 258–69.
12. Gowing LR, Henry-Edwards SM, Irvine RJ et al. The Healtheffects of ecstasy: a literature review. [Review]. Drug Alcohol Rev.2002; 21: 53–63.
13. Stewart CE. Ketamine as a street drug. Emerg. Med. Serv. 2001;30: 30–4.
14. Okun MS, Boothby L, Bartfield R et al. GHB: an importantpharmacologic and clinical update. [Review]. J. Pharm. Pharm.Sci. 2001; 4: 167–75.
15. Dove HW. Phencyclidine: pharmacologic and clinical review.Psychiatr. Med. 1984; 2: 189–209.
16. Liechti ME, KunZ. I, Greminger P et al. Clinical features of gam-mahydroxybutyrate and gamma-butyrolactone toxicity and con-comitant drug and alcohol use. Drug Alcohol Depend. 2006; 81:323–6.
17. Couper FJ, Thatcher JE, Logan BK. Suspected GHB overdoses inthe emergency department. J. Anal. Toxicol. 2004; 28: 481–4.
18. Taylor RL, Cohan SL, White JD. Comprehensive toxicologyscreening in the emergency department: an aid to clinical diag-nosis. Am. J. Emerg. Med. 1985; 3: 507–11.
19. Brett AS. Implications of discordance between clinical impres-sion and toxicology analysis in drug overdose. Arch. Intern. Med.1988; 148: 437–41.
20. Bailey DN, Manoguerra AS. Survey of drug-abuse patterns andtoxicology analysis in an emergency-room population. J Anal.Toxicol. 1980; 4: 199–203.
21. Mason PE, Kerns WP 2nd. Gamma hydroxybutyric acid (GHB)intoxication. Acad. Emerg. Med. 2002; 9: 730–9.
22. Baskin LB, Morgan DL. Drugs detected in patients suspected ofacute intoxication. Tex. Med. 1997; 93 (9): 50–8.
23. Bury RW, Mashford ML. Use of a drug-screening service in aninner-city teaching hospital. Med. J. Aust. 1981; 1: 132–3.
24. Bjornaas MA, Hovda K, Mikalsen H et al. Clinical vs. laboratoryidentification of drugs of abuse in patients admitted for acutepoisoning. Clin. Toxicol. 2006; 44: 127–34.
25. Dietze P, Jolley D, Cvetkovski S et al. Characteristics of non fatalopioid overdoses attended by ambulance services in Australia.Aust. NZ. J. Public Health. 2004; 28: 569–75.
26. Dengenhardt L, Darke S, Dillon P. The prevalence and correlatesof gammahydroxybutyrate (GHB) overdose among Australianusers. Addiction 2003; 98: 199–204.
E West et al.
338 © 2008 The AuthorsJournal compilation © 2008 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine