A Magnet three-peat!Experiential Learning. The final two days were specific to plastic surgery, with...
Transcript of A Magnet three-peat!Experiential Learning. The final two days were specific to plastic surgery, with...

N E W S F R O M T H E R E G I O N ’ S P R E M I E R A C A D E M I C M E D I C A L C E N T E R
ADVANCES SEPTEMBER 8, 2016
Program Spotlight:Plastic surgery boot camp
2
Award honors nursing practice consistency, excellence at hospital
For the third consecutive term, The University of Kansas Hospital has achieved Magnet® designation, which honors hospitals for the high-est level of nursing excellence and is a benchmark of quality patient care.
The designation, which is from the American Nurses Credentialing Center’s (ANCC) Magnet Recognition Program, is effective for five years. Our hospi-tal first earned Magnet status in 2006 – the first in the state – and again in 2011.
Of the nation’s nearly 6,000 hospitals, just 434 (7.8 percent) have achieved Magnet designa-tion. Less than 4 percent have earned it three times in a row.
“This indicates a very strong consistency in the practice of nurs-ing at our hospital,” said Tammy Peterman, RN, executive vice president, chief operating officer
and chief nursing officer.“Our nurses come to work every
day to do the very best they can to provide support and care to our patients and their families,” she added. “They provide exceptional care every day and at every location, and consistently maintain and sustain great outcomes for patients.”
During the Aug. 26 announce-ment, a representative from the Magnet program highlighted several areas of nursing excellence
at our hospital, including men-toring, leadership, community partnerships, professional nursing certification, patient placement and nursing satisfaction.
While Magnet designation is widely accepted as the gold standard of nursing excellence, redesignation is an even more rigorous process. Organizations must provide evidence they have met and exceeded Magnet standards in the years since.
A nursing committee at our hospital spent several years preparing, providing documented evidence of how Magnet con-cepts, performance and quality were improved in the organiza-tion. Four Magnet appraisers visited in June, conducting a rigorous evaluation of nurs-ing services and extensive staff interviews.
“It takes a complete team effort to achieve Magnet designation, especially for the third time as the standards are raised to a higher level of nursing performance,” said Amanda Gartner, RN, who serves as our Magnet program coordinator.
“Achieving Magnet redesignation is truly a continuous journey to improve clinical outcomes and the quality of care our nurses provide.”
A Magnet three-peat!
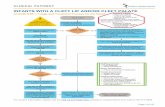
By the Numbers: Our amazing nurses Last week’s major Magnet redesignation announcement underscores one of the many strengths of The University of Kansas Hospital: a reliable and talented nursing staff.
Nursing turnover at our hospital (%)
To suggest a By the Numbers, email [email protected].
2,400 Approximate number of nurses at our hospital
880 of our nurses hold certifications (up from 681 in 2015) in cancer care, trauma, operating room and other
areas of specialization, reflecting their increased training.
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
1816141210
86420
The hospital’s Magnet redesignation was announced Aug. 26 to a standing-room-only crowd of nurses, dignitaries, hospital leaders, physicians and other hospital staff.
13.9
12.6
9.5 11
.3
8.5 8.7
8.3 10
.3
7.1
9.6
10.5
7.9
17.2%National nursing turnover rate 2016
Source: 2016 National Healthcare Retention and RN Staff Report

Events Living with multiple
myeloma – Sponsored by the International Myeloma Foundation, the workshop for patients and families features experts from The University of Kansas Cancer Center, University of North Carolina and Mayo Clinic discussing myeloma ba-sics, transplant, novel therapies and more. The free conference is 9 a.m.-3 p.m. Saturday, Sept. 10, in Overland Park. To register, call 800-452-2873 and ask for the Regional Community Workshop registration.
Stroke Walk team – The University of Kansas Hospital has formed a team to participate in the 14th annual Stroke Walk, which is Saturday, Sept. 10, at Theis Park near the Country Club Plaza. It includes live music, a pan-cake breakfast and more. To join our team, go to americanstroke.org, select “The Stroke Walk,” then register and choose “The University of Kansas Hospital” from the drop-down menu.
Guided imagery for pain – Your brain doesn’t know if you’re really on a beach or just pictur-ing how relaxing it would be. It’s called guided imagery, and research has shown it can help reduce pain and the anxiety and depression that often go with it. Learn more about this powerful technique during a class 2-3 p.m. Wednesday, Sept. 14, at Turning Point: The Center for Hope and Healing in Leawood. Call 913-574-0900 to register.
Ladies’ night – The University of Kansas Cancer Center is hosting a free Ladies’ Night Out series, with local lifestyle special-ists and physicians discussing healthy living in a comfortable, supportive setting. The next ses-sion, “Girls Grill Too,” is 6-8:30 p.m. Tuesday, Sept. 20, at the South location (I-435 and Holmes Road). Get tips from grilling experts and learn about prostate cancer (for the men in your life). Go to kucancercenter.org/lno or call 913-588-1227 to register and for more information.
PROGRAM SPOTLIGHT
A plastic surgery boot camp? Sir, yes sir!Future plastic surgeons are get-
ting an early jump learning their skills, thanks to an innovative “boot camp” held this summer at the University of Kansas Medical Center.
The three-day camp, spon-sored by the American Council of Academic Plastic Surgeons, is designed to provide a solid grounding in the basics of plastic surgery before residents embark on their formal specialty training.
Nineteen medical students attended the July camp, most from the Midwest but a few from Mississippi and Colorado. Similar camps were held at the University of Pittsburgh and the University of South Florida.
“Our goal was to introduce students to major concepts within plastic surgery and also to give them hands-on training with a variety of skills they would not have been exposed to previ-ously,” said Richard Korentager, MD, chair of our Department of Plastic Surgery. He served as course director along with James Butterworth, MD, director of the plastic surgery residency program.
Students spent most of the first day on the basics of operating
room procedures, from how to put on gloves to suturing a patient. They also worked in simulation scenarios in the new Zamierowski Institute for Experiential Learning. The final two days were specific to plastic surgery, with students focused on everything from cleft lips to microsurgery techniques.
Boot camps aren’t new to medical education. Other fields, such as neurosurgery, have used the camps as a way to give their interns a leg up as they transition from general medical school training to learning the specific skills required in their specialty.
Participants of the plastic surgery boot camp lauded the experience. “I love the field of plastic surgery, and to be immersed in it for three days was great,” said Kevin Xiao, MD, a first-year plastic surgery resident at our medical center. “It starts our intern year on a high note.”
The program’s success, said Korentager, is a testament to how well plastic surgery residents, faculty and advanced practice providers delivered an interac-tive experience for students. He already has his sights set on bringing the boot camp back to the medical center next year.
EXPOSURE
Supporting our friends in pink Approximately 200 people joined The University of Kansas Cancer Center’s team during the Aug. 14 Susan G. Komen Greater Kansas City Race for the Cure. The 23rd annual event, held at Union Station, was a fundraiser for breast cancer research and patient care. At our cancer center booth, Communications Specialist Pauline Horton (left) and others handed out thousands of “Get Your Pink On” bags to participants.
Richard Korentager, MD (left), spearheaded the three-day boot camp for aspiring plastic surgeons.

Top rating for Neonatal Medical Home The University of Kansas Hospital’s Neonatal Medical Home
has been designated a Level 3 Patient-Centered Medical Home, the highest level awarded by the National Committee for Quality Assurance.
The top rating is the first in the country for a medical home that specializes in providing primary pediatric care specifically for high-risk Neonatal ICU (NICU) graduates.
The recognition reflects “the way we organize medical care for our young patients and work as a team to coordinate and track care over time,” said Debbie Pennington, RN, the Neonatal Medical Home’s clinical program coordinator.
The Neonatal Medical Home debuted in 2010. The program offers a single point of contact for more than 600 families of medically complex children through age 5. The majority of them were NICU babies discharged from our hospital.
After two successful years, the practice expanded into its own physical clinic, with five exam rooms on the first floor of the main hospital.
A professorship for medical oncology A $1.3 million challenge grant from the Hall Family Foundation
sparked a gift commitment of $650,000 from the Sunderland Family Fund, and together the gifts will establish the A. Drue Jennings Professorship in Medical Oncology at the University of Kansas Medical Center.
The gift will support the salary, travel and associated costs for the medical oncology professorship, which will be at The University of Kansas Cancer Center and in the Department of Internal Medicine at KU Medical Center.
The professorship is named in honor of Drue Jennings, former chairman of the Board of Trustees of KU Endowment. Jennings, of Leawood, is a KU alumnus with a bachelor’s degree in education and a law degree. He is a retired senior counsel for the law firm Polsinelli PC in Kansas City, former interim athletic director for KU and former chairman and CEO of Kansas City Power & Light.
Jennings said he was overwhelmed by the donors’ generos-ity and honored to be the professorship’s namesake.
“Many lives have been improved by the team at our cancer center,” he said, citing the generosity of the Hall Family Founda- tion and the Sunderland Family Fund and the “outstanding leadership” of Roy Jensen, MD, cancer center director, and Bob Page, hospital president and CEO. “We are a better com-munity because of them, and I am personally grateful.”
New
s Br
iefsIn the News
A recap of recent articles, TV segments and other media coverage of the region’s leading academic medical center
Hospital’s training simulations aren’t for dummies – Kansas City Business Journal, Sept. 2. In his column, Editor Brian Kaberline writes about the new Zamierowski Institute for Experiential Learning, a simula-tion lab at The University of Kansas Hospital and University of Kansas Medical Center. The simulation center “offers a completely different level of realism,” he writes. “There, a gauge shows whether CPR chest compressions are at the optimal pressure and speed, and ultrasound shows whether a line is inserted correctly.”
Surgeons protest proposed change in organ donation rules – Buzzfeed News, Aug. 28. A proposal to alter the way donated livers are allo-cated around the country is drawing sharp criticism from many physicians. Timothy Schmitt, MD, director of organ transplantation at The University of Kansas Hospital, is helping lead opposition to the United Network for Organ Sharing (UNOS) proposal, which would send more livers from the Midwest to the East and West coasts, where organ donor rates are lower. If the new rule goes into effect, Schmitt expects our hospital would perform fewer transplants. “We’d have more complexity, more costs and more death.”
KU, community colleges partner on nursing education – The Kansas City Star, Aug. 26. In an effort to help solve a national nursing shortage, the University of Kansas School of Nursing is partnering with five Kansas community colleges in an education program that allows students to earn an associate degree at the same time they work toward their bachelor of science in nursing. Beginning this fall, 43 students from the community colleges are enrolled in the program.
The challenge of treating sepsis – The Washington Post, Aug. 23. The Centers for Disease Control and Prevention has declared sepsis a medical emergency. While physicians and even some specialists around the country struggle to diagnose it, The University of Kansas Hospital has made an astounding reduction in its sepsis mortality rate, according to Steven Simpson, MD, pulmonary and critical care medicine. The turnaround, he said, is due to persistent efforts to catch it early and treat it aggressively.
A Nightingale welcome for new nursing students
The University of Kansas School of Nursing last month hailed a new class of incoming bachelor of science in nursing (BSN) students. During the sixth annual Nightingale Ceremony, 104 students, such as Thea Hack, donned white coats and were welcomed into the nursing profession by Dean Sally Maliski, RN, PhD.
Debbie Pennington, RN, is part of a core team at the Neonatal Medical Home that cares for approximately 600 children, such as 1-year-old Kaden. Many of them are former NICU babies at our hospital.

ADVANCES
is a biweekly publication produced by:
The University of Kansas Hospital Corporate Communications
5799 Broadmoor, Suite 700 Mission, KS 66202
Send story ideas to [email protected].
Bob Page, President and CEO The University of Kansas Hospital
Doug Girod, MD, Executive Vice Chancellor University of Kansas Medical Center
Kirk Benson, MD, President The University of Kansas Physicians
Staff: Mike Glynn, Editor Kirk Buster, Graphic Designer
facebook.com/kuhospital facebook.com/kucancercenterfacebook.com/kumedicalcenter
youtube.com/kuhospitalyoutube.com/kucancercenteryoutube.com/kumedcenter
@kuhospital@kucancercenter@kumedcenter
Our People Award honors nurse’s grace – At
The University of Kansas Hospital, Radiation Oncology’s Liza Murray, APRN, has received a DAISY Award for Extraordinary Nursing.
The award honors the grace she displayed as a nurse on Unit 41, when she helped ease a patient and family through the end of the patient’s life.
It was nearly a year ago when Murray started her shift and de-termined the patient, who had leuke-mia, was deteriorating rapidly. After calling physicians to the bedside, she and the physicians talked with the patient about her status and how her condition had changed.
Working closely with the rest of the healthcare team, Murray com-passionately articulated the serious-ness of her condition and urged the husband to contact family.
“Because Liza initiated conversa-tions, supported the husband and patient with their decisions and used her clinical reasoning to identify the pressing timeline, she was able to encourage the family to come to the bedside and see their loved one,” a fel-low nurse wrote of Murray that night.
“They were able to say their goodbyes, share words of love, and the patient was able to see she was
surrounded by those she cared about.”Her approach to patient care,
Murray notes, was shaped in part by Patch Adams, one of her favorite movies.
“There are several lines in that movie that inspired me when I was a young new nurse, and they still do today,” she said.
“One of them, which I have shared with many of the nurses I trained, is this: ‘You treat a disease, you win, you lose. You treat a person, you will always win.’ This became ever so true working with cancer patients, and it was espe-cially true in this particular situation.”
50 years in the OR – Aline Thomas started as a service aide at The University of Kansas Hospital in August 1966, back when Bonanza and Red Skelton ruled TV.
Thomas went onto become an accomplished surgical tech, working side-by-side with surgeons, handing them scalpels, sponges, clamps and other instruments they needed.
She’s still here a half-century later, and her hospital colleagues in Perioperative Services surprised her with a 50th anniversary celebration.
Her secret? “I love my job,” Thomas said during last month’s festivities, “and our hospital has been good to me.”
Barry Skikne, MD Hematology/Oncology
New
Phy
sici
ans
Alexander Chiu, MD, Otolaryngology
Cameron Ledford, MD Orthopedics
Chantal Lucia Casadonte, MD Pediatrics Gastroenterology
Haley Goucher, MD Anesthesiology
Natasha Ahmed, MD Obstetrics/Gynecology
Liza Murray, APRN (front), was honored by nurses and Radiation Oncology colleagues.
Aline Thomas (front) celebrated with Perioperative Services supervisors (from left) Lisa Elm, RN; Sandy Turner, RN; and Tim Kistner, RN.