Acid fast staining, A PRESENTATION FOR BIOTECHNIC AND BIOTECHNOLOGY CLASS
62873556 Acid Fast Staining for TB
-
Upload
ketdalal1687 -
Category
Documents
-
view
22 -
download
0
description
Transcript of 62873556 Acid Fast Staining for TB
Dr.T.V.Rao MD
ACID FAST STAINING IN
TUBERCULOSIS PRINCIPLES, PRACTICE, AND APPLICATIONS
DR.T.V.RAO MD 1
MICROBIOLOGIC DIAGNOSIS OF TB
DR.T.V.RAO MD 2
Overview:
• Significance of microbiologic testing in TB care
• Sputum staining and processing • Direct smears, unconcentrated
• Fluorochrome staining and fluorescence microscopy
• Concentration and chemical processing
• Specimen collection and transport
• Culture and drug-susceptibility testing
• Rapid diagnostic testing
WHY MICROBIOLOGIC DIAGNOSIS OF TB IS
IMPORTANT
DR.T.V.RAO MD 3
Significance of microbiologic testing for
public health goals and patient care:
• WHO global target of 70% case detection of new smear-positive cases
• Rapid and accurate case detection coupled with effective treatment is essential to reduce the incidence of TB
• Failure to perform a proper diagnostic evaluation before initiating treatment potentially:
• Exposes the patient to the risks of unnecessary or wrong treatment
• May delay accurate diagnosis and proper treatment
• Smear microscopy plays a central role in the diagnosis and management of tuberculosis.
• It is important to understand the aspects of specimen handling and processing that can ensure or enhance accurate results.
MICROBIOLOGIC DIAGNOSIS OF TB
DR.T.V.RAO MD 4
• Sputum smear microscopy is the most important test for the diagnosis of pulmonary TB in many areas of the world
• Direct smears (unconcentrated specimen) are most common
• Fluorescence microscopy and chemical processing can increase sensitivity
• Assessment of laboratory quality is essential
SPUTUM SMEAR MICROSCOPY
DR.T.V.RAO MD 5
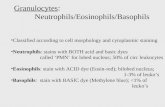
PRINCIPLES OF ZIEHL–NEELSEN STAIN
• The Ziehl–Neelsen stain, also known as the acid-fast stain,
was first described by two German doctors; Franz Ziehl (1859 to
1926), a bacteriologist and Friedrich Neelsen (1854 to 1898), a
pathologist. It is a special bacteriological stain used to identify
acid-fast organisms, mainly Mycobacteria. Mycobacterium
tuberculosis is the most important of this group, as it is
responsible for the disease called tuberculosis (TB) along with
some others of this genus. It is helpful in diagnosing
Mycobacterium tuberculosis since its lipid rich cell wall makes it
resistant to Gram stain. It can also be used to stain few other
bacteria like Nocardia. The reagents used are Ziehl–Neelsen
carbolfuchsin, acid alcohol and methylene blue. Acid-fast bacilli
will be bright red after staining.
DR.T.V.RAO MD 6
PRINCIPLE OF ACID FAST STAINING
• Primary stain binds cell wall mycolic
acids
• Intense decolonization does not release
primary stain from the cell wall of AFB
• Color of AFB-based on primary stain
• Counterstain provides contrasting background
DR.T.V.RAO MD 7
MYCOBACTERIUM ARE ACID FAST
BACILLI • Mycobacterium are Gram-resistant (waxy cell walls),
non-motile, pleomorphic rods, related to the Actinomyces.
Most Mycobacteria are found in habitats such as water or
soil. However, a few are intracellular pathogens of
animals and humans. Mycobacterium tuberculosis, along
with M. bovis, M. africanum, and M. microti all cause the
disease known as tuberculosis (TB) and are members of
the tuberculosis species complex. Each member of the
TB complex is pathogenic, but M. tuberculosis is
pathogenic for humans while M. bovis is usually
pathogenic for animals.
8 DR.T.V.RAO MD
r r r r r
r
Acid Fast Cell Envelope
Cytoplasm
r r r r
Peptidoglycan-mycolic acid-arabinogalactan
Cytoplasmic membrane
Mycolic acid lipids
DR.T.V.RAO MD 9
MYCOBACTERIA STRUCTURE
• Contain large amount
of fatty waxes
(mycolic acid) within
their cell wall resist
staining by ordinary
methods
• Require a special stain
for diagnostic Acid
Fast stain.
DR.T.V.RAO MD 10
ZIEHL-NEELSEN STAIN
• Ziehl-Neelsen staining is used to stain
species of Mycobacterium tuberculosis that
do not stain with the standard laboratory
staining procedures like Gram staining.
• The stains used are the red colored Carbol
fuchsin that stains the bacteria and a
counter stain like Methylene blue or
Malachite green.
DR.T.V.RAO MD 11
AFB STAINING METHODS
• Zeihl Neelsen’s-
hot stain
• Kinyoun’s-cold
stain
• Modifications
12 DR.T.V.RAO MD
EXAMPLE OF ACID-FAST BACTERIA
Each person will make a smear and Acid-Fast stain of a mixed
broth containing:
Mycobacterium smegmatis (Gram +) &
Staphlococcus epidermis (Gram +)
Blue=Non acid-fast bacteria
Red= acid fast bacteria
DR.T.V.RAO MD 13
SPUTUM MICROSCOPY:
DIRECT SMEARS Direct smears of unconcentrated
sputum:
Fast, simple, inexpensive,
widely applicable
Extremely specific for
M. tuberculosis in
high-incidence areas
Ziehl-Neelsen staining (carbol
fuchsin type) most common
DR.T.V.RAO MD 14
• 1. Carbolfuchsin (Red)
• 2. Acid Alcohol
• 3. Counterstain with
Methylene Blue
• Acid - Fast Cells Red
• Non Acid - Fast Blue
ACID - FAST STAIN
BASIC REQUIREMENTS
DR.T.V.RAO MD 15
PROCEEDING WITH ZIEHL- NEELSEN
PROCEDURE
1. Make a smear. Air Dry. Heat Fix.
2. Flood smear with Carbol Fuchsin stain
• Carbol Fuchsin is a lipid soluble, phenolic compound, which is able to penetrate the cell wall
3. Cover flooded smear with filter paper
4. Steam for 10 minutes. Add more Carbol Fuchsin stain as needed
5. Cool slide
6. Rinse with DI water
7. Flood slide with acid alcohol (leave 15 seconds). The acid alcohol contains 3% HCl and 95% ethanol or 20% H2 SO4
• The waxy cell wall then prevents the stain from being removed by the acid alcohol (decolorizer) once it has penetrated the cell wall. The acid alcohol decolorizer will remove the stain from all other cells.
DR.T.V.RAO MD 16
ZIEHL- NEELSEN PROCEDURE
(CONTINUED)
8. Tilt slide 45 degrees over the sink and add acid alcohol drop wise (drop by drop) until the red color stops streaming from the smear
9. Rinse with DI water
10. Add Loeffler’s Methylene Blue stain (counter stain). This stain adds blue color to non-acid fast cells!! Leave Loeffler’s Blue stain on smear for 1 minute
11. Rinse slide. Blot dry.
12. Use oil immersion objective to view.
DR.T.V.RAO MD 18
• Acid-fast cells contain a
large amount of lipids
and waxes in their cell
walls
• primarily mycolic
acid
• Acid fast bacteria are usually
members of the genus
Mycobacterium or Nocardia
• Therefore, this stain is
important to identify
Mycobacterium or Nocardia
ACID-FAST STAIN HOW IT WORKS
DR.T.V.RAO MD 19
BRIGHT-FIELD TECHNIQUES
• Hot Ziehl-Neelsen in practice Most reliable
* more visible AFB
* stronger color
• Cold methods : Kinyoun, Tan Thiam Hok…
* less laborious but also less robust
* higher concentration fuchsin, longer staining time
errors !!
* not recommended for low-income countries
DR.T.V.RAO MD 20
SELECTING A IDEAL SPUTUM SAMPLE
• W What is a good sample?
• What is saliva?
• Good sample = yellow? mucous fluid?
• Discharge from the bronchial tree
• May contain solid or purulent substances
• Minimal amounts of oral/ nasal material
• May contain macrophages and other cells indicative of infectious disease
• Follow-up examination samples?
DR.T.V.RAO MD 22
• Collect specimens in a laboratory-approved, leak-proof container
• Label all containers (name and date collected)
• Collect specimens prior to initiation of therapy
• Infection Control: Consider the safety of other patients and healthcare workers
• Collect sputum in well-ventilated area, preferably outdoors
SPECIMEN COLLECTION AND
TRANSPORT
DR.T.V.RAO MD 23
• Minimize contamination of specimens by:
• Instructing the patient to rinse mouth with water before collection
• Transport the specimen to the lab as soon as feasible after collection
• Keep specimens refrigerated if possible
SPECIMEN COLLECTION AND
TRANSPORT
DR.T.V.RAO MD 24
Standard 2: All patients
(adults, adolescents, and
children who are capable of
producing sputum)
suspected of having
pulmonary TB should have
at least two sputum
specimens obtained for
microscopic examination
in a quality-assured
laboratory. When possible,
at least one early morning
specimen should be
obtained.
STANDARD 2: SPUTUM MICROSCOPY
DR.T.V.RAO MD 25
Sputum processing for optimizing smear
results (vs. direct smear of unconcentrated
sputum): Concentration by centrifugation and/or sedimentation
Chemical pretreatment (e.g., bleach, NaOH, NaLC) for decontamination and
digestion
Usually both
Higher sensitivity (15-20% increase) and
higher smear positive rate
SPUTUM PROCESSING
Steingart KR, et al. Lancet Infect. Dis. 2006; 6 (10):664-74 DR.T.V.RAO MD 26
Standard 3: For all patients (adults, adolescents, and children) suspected of having extra pulmonary TB, appropriate specimens from the suspected sites of involvement should be obtained for microscopy, culture, and histopathological examination.
Standard 4: All persons with chest radiographic findings suggestive of tuberculosis should have sputum specimens submitted for microbiological examination
STANDARDS 3 & 4: SPUTUM
MICROSCOPY
DR.T.V.RAO MD 27
MICROSCOPIC READING:
Red slender rods on blue background
accept only typical shape, at least some
depends condition of microscope! Light
binocular, mechanical stage, good optics
100x oil immersion objective, 10x eyepieces
• Requires: patience, sincerity
AFB microscopy is not difficult but tough
DR.T.V.RAO MD 29
ADVANTAGES AND DISADVANTAGE
OF ACID FAST BACTERIA
• Advantages:
• Acid-fast cells contain a large amount of lipids and waxes in
their cell walls, making them relatively impermeable and
resistant to many disinfectants
• Also enables resistance to desiccation, antibiotics, and other
toxins
• Disadvantage:
• Waxes delay nutrient uptake, so cells grow slower
• Ziehl-Neelsen Method is used to stain acid-fast bacteria
DR.T.V.RAO MD 30
ZEIHL NEELSEN AND FLUOROCHROME MICROSCOPY AFB QUANTIFICATION SCALES
System & Quantification Scale
No. of AFB
per field
Brightf. &
IUATLD/WHO
Scale (1000x)
Brightf. & ATS
Scale
(1000x)
Fluor. &
IUATLD/WHO
Scale
(200-250x)
Fluor. & ATS
Scale
(200-250x)
None
1-2/300 fields
1-9/100 fields
1-9/10 fields
1-9/1 field
10-99/1field
>=100/1field
Negative
Actual
Actual
1+
2+
3+
3+
Negative
Actual
1+
2+
3+
4+
4+
Negative
Actual
Actual
Actual
1+
2+
3+
Negative
Actual
Actual
1+
2+
3+
4+
DR.T.V.RAO MD 31
SPUTUM MICROSCOPY:
FLUOROCHROME STAIN Fluorochrome stain
• Fluorochrome stained smears require a
fluorescent microscope
• Generally read at 250X-450X magnification
which allows rapid scanning of the smear
• Auramine-rhodamine is an example of such a
stain where the AFB appear yellow against a
black background
DR.T.V.RAO MD 32
* More rapid and sensitive
* Specificity : same with sufficient expérience
* Equipment cost , bulbs, technical demands
* for busy labs
* External quality assessment should be done if this method is performed
FLUOROCHROME AFB MICROSCOPY
DR.T.V.RAO MD 33
FLUORESCENCE MICROSCOPY Advantages:
• More accurate: 10% more sensitive
than light microscopy, with specificity
comparable to ZN staining
• Faster to examine = less technician
time
Disadvantages:
• Higher cost and technical complexity,
less feasible in many areas
Steingart KR, et al. Lancet Infect. Dis. 2006; 6 (9):570-81 DR.T.V.RAO MD 34
FLUORESCENCE MICROSCOPY Advantages:
• More accurate: 10% more sensitive than light microscopy, with specificity comparable to ZN staining
• Faster to examine = less technician time
Disadvantages:
• Higher cost and technical complexity, less feasible in many areas
Steingart KR, et al. Lancet Infect. Dis. 2006; 6 (9):570-81 DR.T.V.RAO MD 37
Although sputum
microscopy is the first
bacteriologic diagnostic
test of choice, both
culture and drug
susceptibility testing
(DST) can offer
significant advantages in
the diagnosis and
management of TB.
CULTURE AND DRUG
SUSCEPTIBILITY TESTING
DR.T.V.RAO MD 38
INTERNATIONAL STANDARDS FOR
TUBERCULOSIS CARE.
DR.T.V.RAO MD 39
The International Standards for Tuberculosis Care (ISTC) describe a widely
endorsed level of care that all practitioners should seek to achieve in managing
individuals who have, or are suspected of having, tuberculosis.
The basic principles of care for people with, or suspected of having, tuberculosis
are the same worldwide: a diagnosis should be established promptly;
standardized treatment regimens should be used with appropriate treatment
support and supervision; response to treatment should be monitored; and
essential public-health responsibilities must be carried out. Prompt and accurate
diagnosis, and effective treatment are essential for good patient care and
tuberculosis control. All providers who undertake evaluation and treatment of
patients with tuberculosis must recognize that not only are they delivering care
to an individual, but they are also assuming an important public-health function.
APPLICATION OF INTERNATIONAL STANDARDS FOR
TUBERCULOSIS CARE (ISTC) STANDARDS BETTER
CARE OF TUBERCULOSIS PATIENTS
DR.T.V.RAO MD 40
•The ISTC consist of 21 evidence-based standards. The original
17 standards from 2006 were revised and renumbered in 2009.
•Standards differ from existing guidelines in that standards present
what should be done, whereas, guidelines describe how the
action is to be accomplished.
•To meet the requirements of the Standards, approaches and
strategies, determined by local circumstances and practices and
developed in collaboration with local and national public health
authorities, will be necessary. There are many situations in which
the level of care can, and should, go beyond what is specified in
the Standards
BETTER GOALS IN MICROBIOLOGIC
DIAGNOSIS OF TB
• Culture and drug-
sensitivity testing should be obtained, when feasible, for smear-negative TB and treatment failure.
• Quality assurance is essential for all TB diagnostic procedures
DR.T.V.RAO MD 42
SUMMARY: ISTC STANDARDS
COVERED* Standard 2: All TB suspects should have at least 2
sputum specimens obtained for microscopic
examination (at least one early morning specimen if
possible).
Standard 3: Specimens from suspected extra pulmonary
TB sites should be obtained for microscopy, culture and
histopathological exam.
Standard 4: All persons with chest radiographic findings
suggestive of TB should have sputum specimens
submitted for microbiological examination. DR.T.V.RAO MD 43
SUMMARY: ISTC STANDARDS
COVERED*
s
Standard 5: The diagnosis of smear-negative pulmonary TB should be based on the following: at least two negative sputum smears (including at least one early morning specimen); CXR finding consistent with TB; lack of response to broad-spectrum antibiotics (avoid fluoroquinolones), and culture data. Empiric treatment if severe illness.
Standard 6*: In all children suspected of having intrathoracic and extrapulmonary TB, specimens (sputum, extrapulmonary tissue) should be obtained for microscopy, culture, and histopathological (tissue) examination. TB diagnosis should be based on chest radiography, history of TB exposure, positive TB test, and suggestive clinical findings if bacteriologic studies are negative.
DR.T.V.RAO MD 44
SUMMARY: ISTC STANDARDS
COVERED* Standard 10 (partial): Response to therapy in
patients with pulmonary tuberculosis should be monitored by follow-up sputum smear microscopy (2 specimens) at the time of completion of the initial phase of treatment (2 months).
If the sputum smear is positive at completion of the initial phase, sputum smears should be examined again at 3 months and, if possible, culture and drug susceptibility testing should be performed.
DR.T.V.RAO MD 45
SUMMARY: ISTC STANDARDS
COVERED* Standard 11: An assessment of the likelihood of drug resistance,
based on history of prior treatment, exposure to a possible source case having drug-resistant organisms, and the community prevalence of drug resistance, should be obtained.
• DST should be performed at the start of therapy for all previously treated patients
• For patients in whom drug resistance is considered to be likely, culture and testing for susceptibility/resistance to at least isoniazid and rifampicin should be performed promptly
• Patient counseling and education should begin immediately to minimize the potential for transmission
• Infection control measures appropriate to the setting should be applied
DR.T.V.RAO MD 46
ISTC: KEY POINTS • 21 Standards (revised/renumbered in 2009)
• Differ from existing guidelines: standards present
what should be done, whereas, guidelines
describe how the action is to be accomplished
• Evidence-based, living document
• Developed in tandem with Patients’ Charter for
Tuberculosis Care
• Handbook for using the International Standards for
Tuberculosis Care DR.T.V.RAO MD 47
• Audience: all health care practitioners, public and
private
• Scope: diagnosis, treatment, and public health
responsibilities; intended to complement local and
national guidelines
• Rationale: sound tuberculosis control requires the
effective engagement of all providers in providing
high quality care and in collaborating with TB control
programs
ISTC: KEY POINTS
DR.T.V.RAO MD 48
• Successful implementation of the
Global Plan depends on
implementation of the new 6-point
STOP TB strategy recommended by
WHO. This strategy promotes use of
the new International Standards for
Tuberculosis Care to engage all
care providers (including those in
the private sector) in delivering high-
quality care. It specifically addresses
HIV-associated TB, MDR-TB and
other challenges, and strengthens
human rights and health systems.
However, the plan also relies on new
diagnostic tests, new drugs and TB
vaccines being developed by or
before 2015.
PLAN OF ACTION BY WHO
DR.T.V.RAO MD 49
CREATED FOR MICROBIOLOGISTS AND
HEALTH CARE WORKERS IN DEVELOPING
WORLD
DR.T.V.RAO MD 52
































































![Amino acid profile, microbiological and farinographic ...€¦ · methylene blue was added for staining [19]. After staining, the slide was mounted on a microscope for identification](https://static.fdocuments.net/doc/165x107/5f05f7f77e708231d415a17b/amino-acid-profile-microbiological-and-farinographic-methylene-blue-was-added.jpg)