485 Is the etiology of low birthweight births different in rural and urban populations?
Click here to load reader
Transcript of 485 Is the etiology of low birthweight births different in rural and urban populations?

378 spa Abstracts
482 SIGNIFICANT RESPIRATORY DISTRESS SYNDROME AT GESTATIONAL AGES GREATER THAN 34 WEEKS IN OLMSTED COUNTY. J Iverson*, JANey, CSField*, RD Ellefson*, Mayo Clinic, Rochester, MN
Most urban centers report a low incidence of respiratory distress syndrome (RDS) after 34 weeks. Our population is primarily upper middle class, caucasian, with good compliance with early prenatal care. We tested the hypothesis that significant RDS exists in this well-dated population after 34 weeks. First, all deliveries from 1/90 to 7/90 were reviewed for the incidence of RDS at gestational ages of 32-37 weeks. Then, all pulmonary maturity studies from 1/88 to 6/90 were reviewed for the absence of phosphati dyl glycero 1 (PG) and clinical RDS if delivered within four days of testing.
Incidence RDS Amnio Neonatal Total Population rested Population
weeks n (%J PG - PG - with RDS 32-33 10/16 (63) 12/16 (75) 8/12 (67) 34-35 7/30 (23) 26/40 (65) 11/26 (42) 36-37 2/94 (2) 33/72 (46) 3/33 (9) Conclusions: In our population, initiation of tocolysis may be warranted as late as 34-35 weeks with an incidence of RDS of 23% and with significant RDS in 42% of patients who deliver with PG negative.
483 A 10-YEAR REVIEW OF PRETERM BIRTH OF TWINS AT A REFERRAL TERTIARY CARE CENTER Edward Wolf,Angie Mallozzi, John F. RodlS, Winston Campbell, Judith Mead, Anthony M Vlntzileos. Univ of Connecticut Health Center, Farmington, CT.
The incidence of preterm delivery in tWin gestations may be as high as 50%. Study protocols to detect and treat preterm labor have reported a decrease In the InCidence of preterm delivery but the preterm birth rate has remained well above that for singletons. Little attention has been paid to the question of whether the frequency of conditions that resutt in preterm twin delivery differs from those that result In the delivery of preterm singletons. All 221 twin gestations that delivered at 24-36 completed gestational weeks from 1980-1989 were reviewed to determine the primary complication resulting in preterm delivery. These were then compared to all 1,976 singleton preterm deliveries that occurred over the same time period:
TWINS SINGLETON COMPLICATIONS n % n % pvalue PROM 93 42 906 46 NS PTL 68 31 402 20 .001 HEMORRHAGE 8 4 177 9 .01 PIH 25 11 296 15 NS IUGR 14 6 38 2 .001 OTHER 13 6 157 8 NS The tWin gestations that delivered from 24-31 weeks were compared to those that delivered from 32-36 weeks. The only statistically significant difference was an increase in the 32-36 week group of IUGR as the indication for delivery (p=.05). Preterm labor is responsible for a greater proportion of the preterm delivery of twin gestations than singletons. Nonetheless in both singletons and twins the most frequent single cause of preterm delivery is premature rupture of the membranes. Preterm labor prevention programs may exclude the primary complication that leads to preterm delivery in over two-thirds of twin gestations.
J<lnLl,l" )'19) Am J O)),ll'l G\ nl'w)
484 A 10-YEAR REVIEW OF PRETERM BIRTHS AT A REFERRAL TERTIARY CARE CENTER. Edward J Wolf, Angle MallOZZI, John F. Rodis, Winston A Campbell, Anthony M. Vlntzlleos. University of Connecticut Health Center, Farmington, CT.
Preterm birth is the major cause of pennatal mortality in the United States but the preterm birth rate has remained stable over the past 30 years. Most preterm birth prevention programs are primarily structured to detect and prevent preterm labor as the primary cause of preterm birth. Delivery and/or hospltaJ records were reViewed for all 1,976 preterm (24-36 completed gestational weeks) singleton pregnancies delivered at our institution from 1980-1989 to determine the primary complication that resuJted in preterm delivery. COMPLICATION Ll % of TOTAL Premature rupture of membranes 906 46 Preterm Jabor 402 20 PregnancY-Induced hypertension 296 15 Hemorrhage 177 9 Other (fetal distress, JUGR, etc.) ill 1Q
TOTAL 1,976 100 Those pregnancies of 24-31 weeks were compared to those of 32-36 weeks gestation to determine If the primary complication differed: COMPLICATION 24-31 weeks 32-36 weeks
n % n % pvaJue PROM 411 46 495 46 NS Preterm Jabor 204 23 198 18 .01 PIH 112 13 184 17 .01 Hemorrhage 107 12 70 6 .01 Other .5Q..a 1.39.. 1.3. .01
TOTAL 890 100 1,086 1 00 Idiopathic preterm Jabor compromised only 20% of 1,976 preterm Singleton deliveries and further research into the etiology and prevention of preterm birth should focus more strongly on the prevention of PROM.
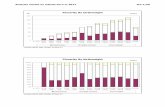
485 IS THE ETIOLOGY OF LOW BIRTHWEIGHT BIRTHS DIFFERENT IN RURAL AND URBAN POPULATIONS? Mary Lou Moore, Ph.D" RNC: Paul Meis, M.D., Robert Michielutte, Ph.D.,' J.M. Ernest, M.D., Paul Buescher, Ph.D.' Departments of Obstetrics and Gynecology and Family and Community Medicine, Bowman Gray School of Medicine of Wake Forest University, Winston-Salem, NC and N C Carolina Center for Health Statistics, Raleigh, NC
In two studies, programs to decrease low birthweight births (LBW) in rural areas have been successful; not all studies in urban areas have reported success. One explanation may lie in the etiology of LBW among women living in rural and urban areas. We reviewed maternal records and classified 3,910 LBW births from 7 rural, 8 semi-urban and 3 urban counties in North Carolina Perinatal Region II for the years 1984-1987 by etiology, There was a statistically significant difference (p = ,0006) between rural and urban areas in the incidence of 4 etiologies (idiopathiC preterm labor, preterm-PROM, termLBW, medically indicated birth) in the 3 areas, When age and race were controlled, the difference remained significant (p = .023). LBW at term was the most frequent etiology in rural populations; idiopathic preterm labor was most frequent among urban women. PCT Urban T-LBW P-PROM
0-19% 33.67 24.50 20-49% 30.74 21.40 50+% 27.42 27.47
MEDIND 15.14 16.79 15.20
IPL 26.69 31.07 29.92