3 s2.0-b9780323067942000481-maingez
-
Upload
egn-njeba -
Category
Government & Nonprofit
-
view
15 -
download
0
Transcript of 3 s2.0-b9780323067942000481-maingez

Chap
ter
48Ann K. Kim, MD, Gul Moonis, MD, andLaurie A. Loevner, MD
Brain: anatomy, trauma, and tumors
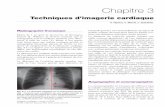
1. Identify the parts of the brain labeled 1 through 6 in Fig. 48-1.See figure legend for answers.
2. What are the two primary imaging modalities used to image the brain?The two major noninvasive cross-sectional imaging modalities used in neuroimaging are computed tomography (CT) and magnetic resonance imaging (MRI). Catheter angiography is reserved for the detection of intracranial vascular processes, such as aneurysms and intracranial vasculitis. Myelography involves the injection of contrast material into the subarachnoid space by lumbar puncture, allowing visualization of the spinal cord and nerve roots, which are seen as “filling defects” within the contrast-opacified cerebrospinal fluid (CSF). Myelography (usually followed by postmyelography CT) is reserved for patients with contraindications to MRI (e.g., patients with pacemakers or severe claustrophobia), patients with surgical hardware (pedicle screws), patients with equivocal MRI findings, and obese patients who exceed weight limits for MRI scanners.
3. What are the clinical indications for obtaining CT and MRI of the brain?A CT scan is a good initial screening examination for evaluating the brain for the presence of abnormalities. It is the primary imaging modality for assessing for acute intracranial hemorrhage, subarachnoid hemorrhage (SAH), mass effect, hydrocephalus, and stroke. The greater tissue contrast of MRI and its multiplanar capabilities make MRI the imaging modality of choice, however, for the assessment of a large spectrum of pathologic processes, including, but not limited to, metastatic disease, primary glial neoplasms, neurodegenerative disorders, and inflammatory and infectious processes. MRI is less sensitive than CT for the detection of SAH and calcification. In many instances, CT and MRI have complementary roles in the evaluation of pathologic conditions (especially lesions at the skull base and lesions involving the calvaria).
327
5
5
1
1
2
2
3
3
6
6
4
4
A B
Figure 48-1. A, Axial T2-weighted MR image of the brain at the level of the basal ganglia (1, caudate head; 2, putamen; 3, third ventricle; 4, insular cortex; 5, septum pellucidum; 6, thalamus). B, Sagittal T1-weighted image of the brain at midline (1, anterior genu of the corpus callosum; 2, posterior lobe of the pituitary gland [“pituitary bright spot”]; 3, pons; 4, tectal plate; 5, splenium of the corpus callosum; 6, mass intermedia).

328 Brain: anatomy, trauma, and tumors
4. What are contraindications for performing MRI of the brain?Contraindications include implanted electronic devices, such as pacemakers, neurostimulator devices, non–MRI-compatible vascular clips, ferromagnetic metallic implants, and foreign bodies in the eye. Severe claustrophobia is a relative contraindication, and, if necessary, most patients with this condition can successfully undergo MRI with sedation. MRI cannot be performed on individuals who have a metallic intracranial aneurysm clip. Most aneurysm clips used after 1995 are made of titanium and are MRI-compatible.
5. Define the terms intra-axial and extra-axial, which are commonly used to localize intracranial pathologic conditions.An intra-axial abnormality arises from the brain parenchyma. An extra-axial lesion is one that arises outside of the brain substance and may be pial, dural, subdural, epidural, or intraventricular in origin. The most common extra-axial mass is a meningioma. In adults, the most common solitary intra-axial masses are primary brain tumors and metastatic disease. An intra-axial mass lesion expands the brain, results in gyral swelling, or results in effacement of the cerebral sulci. Imaging features that identify a mass as extra-axial include inward buckling of the gray and white matter, the presence of a cleft (which may be CSF, dura, or small vessels) separating the extra-axial mass from the brain, and the presence of remodeling of the adjacent osseous calvaria (Fig. 48-2).
6. What is nephrogenic systemic fibrosis (NSF), and who is at risk for developing this complication?NSF is a rare systemic syndrome that involves fibrosis of the skin, muscles, joints, eyes, and internal organs. It is a disease process seen in patients with severe renal dysfunction and patients with renal dysfunction awaiting liver transplants (concomitant liver failure). At the time of this writing, no known cases of NSF have been seen in patients with normal renal function. There is an accepted association of the administration of the MRI contrast agent gadodiamide (Omniscan) with the development of NSF in patients with renal failure. Gadolinium-based contrast agents are metabolized entirely through the renal system; gadolinium agents have a prolonged half-life in renal failure patients. Metabolic by-products may result in the formation of free Gd3+, which is very toxic. Not all patients with renal failure who received gadodiamide developed NSF, however, so other factors are present that contribute to its development. Increased incidence of NSF was seen in patients when there was a delay of greater than 2 days between administration of contrast agent and receiving dialysis. Research in this area is ongoing.
A B
Figure 48-2. A, Intracranial meningioma. Sagittal T2-weighted MR image shows large meningioma in the left frontotemporal region that is isointense to gray matter. Note the inward buckling of the gray and white matter (arrows) and the CSF cleft (arrowheads), indicating its extra-axial site of origin. B, Axial T1-weighted contrast-enhanced image shows homogeneous enhancement of this mass with a dural tail (arrow), characteristic of a meningioma.

Brain: anatomy, trauma, and tumors 329neuroradiology
7. Is gadodiamide the only MRI contrast agent available?No. There are five U.S. Food and Drug Administration(FDA)–approved gadolinium-containing MRI contrast agents: gadodiamide (Omniscan), gadoversetamide (OptiMARK), gadopentetate dimeglumine (Magnevist), gadobenate dimeglumine (MultiHance), and gadoteridol (ProHance). NSF has been reported only with Omniscan as of this writing. The FDA is actively investigating potential associations with all gadolinium-containing contrast agents. It is imperative for one to be familiar with the specific institution’s guidelines on the administration of MRI contrast agents in patients with renal insufficiency.
8. What is the imaging modality of choice for imaging acute head trauma?The imaging modality of choice for imaging acute head trauma is an unenhanced brain CT scan. CT is readily available and is a fast, accurate method for detecting acute intracranial hemorrhage. On CT, acute hemorrhage is hyperdense to brain and may display mass effect. Emergency physicians and neurosurgeons want to know the exact cause of clinical symptoms in a trauma patient. Specifically, the most significant concern is whether there is a treatable lesion. CT plays a primary role in evaluating the extent of trauma and in determining the appropriate management. It is sensitive in distinguishing brain contusions from extra-axial hematomas (subdural and epidural). CT is also excellent for detecting depressed facial and calvarial fractures. When diffuse axonal shear injury is suspected, MRI is more sensitive and can be obtained when the patient is clinically able to tolerate this examination.
9. How does one differentiate a subdural hematoma from an epidural hematoma?An epidural hematoma is usually caused by an arterial injury (most commonly, the middle meningeal artery is injured as a result of a fracture of the temporal bone through which it courses) (Fig. 48-3A). An epidural hematoma is extra-axial, runs between the periosteum of the inner table of the skull and the dura, and is confined by the lateral sutures (especially the coronal sutures) where the dura inserts. As a result, an epidural hematoma is usually lenticular in shape. In contrast, a subdural hematoma is usually caused by injury to the bridging cortical veins (Fig. 48-3B). A subdural hematoma runs between the dura and the pia-arachnoid meninges on the surface of the brain and is not confined by the lateral sutures. As a result, subdural hematomas are usually crescentic in shape. In the midline, the dural reflection is attached to the falx cerebri, however. Subdural hematomas (in contrast to epidural hematomas) do not cross the midline, but rather track in the interhemispheric fissure. Subdural hematomas are commonly seen in patients with closed head trauma; elderly patients with minor head trauma; and patients with rapid decompression of hydrocephalus and extra-axial hematomas, where abrupt changes in intracranial pressure make the bridging cortical veins vulnerable.
A B
Figure 48-3. A, Axial unenhanced CT scan shows hyperdense, lenticular-shaped epidural hematoma in the left temporoparietal region. Note the mass effect on the adjacent left lateral ventricle that is effaced (arrows). B, Axial unenhanced CT scan shows right hemispheric subdural hematoma (arrows) that crosses the coronal and lambdoid sutures. Note the hyperdensity in the sulci of the left cerebral hemisphere, consistent with acute SAH (arrowheads).

330 Brain: anatomy, trauma, and tumors
Key Points: Subdural Hemorrhage
1. This is a venous injury to bridging cortical veins.2. Skull fracture may not be present.3. It is usually crescentic in shape and not contained by
sutures; it does not cross falx or tentorium.4. This is found in trauma patients, older patients, and
child abuse victims.
Key Points: Epidural Hemorrhage
1. This is an arterial injury, usually the middle meningeal artery.
2. It is associated with temporal bone or other skull fractures.3. It has a biconvex, lenticular shape; blood is contained
by dural sutures.4. This is a surgical emergency.
10. What is the CT appearance of traumatic SAH?SAH appears as hyperdensity in the subarachnoid spaces. The subarachnoid spaces are identified by their serpentine appearance, dipping in between the gyri of the brain (see Fig. 48-3B). SAH in the setting of trauma usually indicates the presence of superficial cortical contusions.
Key Points: Subarachnoid Hemorrhage
1. Blood is in subarachnoid spaces; hyperdensity is in CSF spaces.
2. Aneurysm rupture or post-traumatic superficial cortical contusions are the cause.
3. Vasospasm several days afterward may lead to secondary infarction.
11. What is the Glasgow Coma Scale? How is it used?The Glasgow Coma Scale was devised to provide a uniform approach to clinical assessment of trauma patients with acute head trauma. To measure level of awareness and responsiveness, the scale assigns numeric values (1 to 5) to each of the following: eye opening, best motor response, and best verbal response. Scores of 13 to 15 correspond to mild closed head injury; 9 to 12, to moderate head injury; and 8 or less to severe brain injury. The Glasgow Coma Scale does not correlate with survival outcome in cases of severe head trauma with coma.
12. What are the advantages and drawbacks of MRI in assessing a trauma patient?The availability and speed of CT and its high sensitivity in detecting treatable lesions make it the imaging modality of choice for the initial assessment of trauma patients with head injury. MRI is more sensitive in distinguishing between the different ages of hemorrhage (hyperacute, acute, subacute, and chronic), in detecting shear injury (diffuse axonal injury), and in detecting injury in the posterior fossa and the undersurfaces of the frontal and temporal lobes. MRI is less sensitive than CT in detecting intracranial air and fractures. In addition, logistic difficulties occur in performing MRI on trauma patients: MRI times are significantly longer, performing MRI in patients on ventilators and other monitoring devices can be very cumbersome, and the location of most MRI scanners is outside of the emergency department. Although the fluid-attenuated inversion recovery (FLAIR) sequence on MRI can be as sensitive or more sensitive than CT in detecting subarachnoid hemorrhage, it is less specific, and the difficulty in quickly obtaining MRI in the acute trauma setting still renders CT the study of choice in assessing a trauma patient.
13. Define penetrating injury to the brain, and identify common causes.Penetrating injuries result in brain “lacerations,” and they are most commonly associated with bullets, stab wounds, and depressed or dislodged bone fragments. There is risk of injury to all vital structures traversed by the penetrating object. The most important of these are the brain and vascular structures (arteries and veins/dural venous sinuses).

Brain: anatomy, trauma, and tumors 331neuroradiology
14. What are the five patterns of brain herniation and herniation syndromes?The brain is in a confined compartment (the skull) and is compartmentalized further by inelastic dural attachments (falx cerebri, falx cerebelli, and tentorium). Brain swelling, or mass lesions when large enough, forces brain from one compartment into another. If untreated, this herniation can result in further brain damage and vascular injury. Five patterns of brain herniation are as follows:
• Inferior tonsillar/cerebellar• Superior vermian (upward)• Temporal lobe• Subfalcine• Central transtentorial
Mass effect, especially in the posterior fossa, may also result in acute, obstructive hydrocephalus.
15. What is the imaging manifestation of a brain contusion?Contusions are parenchymal bruises of the brain with associated petechial hemorrhage usually related to direct trauma to the head. The most common locations are the inferior, anterior, and lateral surfaces of the frontal and temporal lobes, owing to direct impact of the brain against the rough edges of the inner table of the skull along the floor of the anterior cranial fossa, the sphenoid wing, and the petrous ridges. On CT, hemorrhagic contusions appear as focal areas of hyperdensity (blood) with surrounding hypodensity (edema) in characteristic anatomic locations of the brain. On T2-weighted MR images, acute hemorrhagic contusions are hypointense (dark) with surrounding high-intensity (bright) edema. On gradient-echo susceptibility images, these lesions are detected with increased sensitivity as areas of signal drop-out (hypointensity, or “dark”).
16. What are the imaging manifestations of diffuse axonal injury?Diffuse axonal injury is commonly associated with coma, immediate cognitive decline, and poor outcome in patients with significant closed head injury. The stress induced by rotational acceleration/deceleration movement of the head causes differential motion to occur between the neuronal body and axon, which is the area of greatest density difference in the brain. This motion causes axon disruption and formation of retraction balls. The sites most commonly involved include the body and splenium of the corpus callosum, brainstem, superior cerebellar peduncle, internal capsule, and gray-white junction of the cerebrum. On CT, diffuse axonal injury may not be initially detected. On follow-up MRI, rounded or elliptic T2 hyperintense foci are seen in characteristic locations, and they are commonly hemorrhagic.
17. Primary brain tumors in adults usually arise from what cell line?Most primary intra-axial tumors of the brain arise from the supporting microglial cells. Gliomas account for 35% to 45% of all intracranial tumors. Glioblastoma multiforme accounts for 35% of gliomas and has a very poor prognosis, with survival rates commonly less than 1 year. Astrocytomas, ependymomas, medulloblastomas, and oligodendrogliomas are other, more commonly encountered primary brain tumors.
18. What is the most common benign extra-axial tumor in adults?The prototypic extra-axial tumor in adults is meningioma. This tumor commonly affects middle-aged women and arises from the arachnoid of the meninges. The most common locations are the parasagittal dura of the falx, the cerebral convexities, the sphenoid wing, the olfactory groove, and the planum sphenoidale. Other locations include the tuberculum sella and orbit, the cerebellopontine angle, and the cavernous sinus. On unenhanced CT, most meningiomas are slightly hyperdense compared with normal brain tissue, with calcifications present in approximately 20%. There may be associated osseous hyperostosis involving the adjacent bone. On MRI, meningiomas are isointense to slightly hyperintense relative to gray matter on T2-weighted images. Meningiomas enhance intensely and homogeneously (see Fig. 48-2). A CSF cleft between the mass and the brain is often present, identifying its extra-axial location. Although the presence of a dural tail is typical of a meningioma, it may not be seen in 30% of cases (see Fig. 48-2B).
19. What are the most common neoplasms arising in the corpus callosum?The corpus callosum is the largest white matter tract, and it connects the two cerebral hemispheres in the midline. The most common tumors that affect the corpus callosum are glioblastoma multiforme and lymphoma. The extension of a neoplasm from one hemisphere to the other via the corpus callosum produces the so-called butterfly pattern (Fig. 48-4). Other non-neoplastic white matter diseases that commonly involve the corpus callosum include demyelinating disease (especially multiple sclerosis) and trauma (diffuse axonal injury).
20. What are the most common systemic neoplasms to metastasize to the brain?Breast cancer, carcinoma of the lung, and melanoma most commonly spread hematogenously to the brain. Hemorrhagic brain metastases are common with melanoma, choriocarcinoma, thyroid cancer, and renal cell carcinoma; however, because breast and lung cancer are so much more common, it is more likely that a hemorrhagic metastasis is related to

332 Brain: anatomy, trauma, and tumors
AA B C
Figure 48-4. Glioblastoma multiforme. A, Axial unenhanced CT scan shows ill-defined hyperdense mass in both frontal lobes (arrows), crossing the corpus callosum in a pattern characteristic of a “butterfly” glioma. B, Axial FLAIR MR image shows the mass is hyperintense (bright) relative to brain. C, Axial T1-weighted postcontrast image shows diffuse faint enhancement with a central area of necrosis (arrow).
one of these latter cancers. Calcified metastases may be seen with mucinous adenocarcinomas (lung, colon, stomach,ovary, and breast) and bone cancers (osteosarcoma and chondrosarcoma).
21. What are the most common primary brain tumors that calcify?Oligodendroglioma, ependymoma, astrocytoma, craniopharyngioma, and ganglioglioma are primary central nervous system tumors that most commonly calcify.
22. What is the imaging appearance of leptomeningeal carcinomatosis or subarachnoid seeding? What are the most common tumors producing it in adults?Subarachnoid seeding or leptomeningeal tumor is characterized by tiny nodules of tumor implanted on the surface of the brain or spinal cord or both. There is “sugar-coating” of the subarachnoid spaces. T1-weighted MRI with contrast enhancement is best at showing this nodular enhancement, particularly in the basilar cisterns, over the cerebral convexities, and along the cranial nerves (Fig. 48-5). Communicating hydrocephalus may result from obstruction of thearachnoid villi.
23. What are the most common tumors producing subarachnoid seeding in adults?Many primary central nervous system tumors seed the subarachnoid spaces (e.g., glioblastoma multiforme, oligodendroglioma, ependymoma). Metastatic systemic tumors that commonly spread to the CSF or leptomeninges include breast and lung carcinoma, melanoma, and hematologic malignancies (lymphoma and leukemia).
A B C
Figure 48-5. Leptomeningeal spread of lymphoma. A-C, Axial T1-weighted postcontrast MR images show abnormal enhancement of bilateral internal auditory canals (arrows in A), bilateral fifth cranial nerves (arrows in B), and subarachnoid spaces of the right frontal lobe (arrows in C).

Brain: anatomy, trauma, and tumors 333neuroradiology
A B
Figure 48-6. Vestibular schwannoma. A, Axial high-resolution T2-weighted MR image shows hypointense mass (arrow) in the left cerebellopontine angle extending into the internal auditory canal and expanding the porus acusticus (arrowheads). B, Axial T1-weighted postcontrast image shows characteristic enhancement of the mass.
24. Why would a mass appear hyperdense on unenhanced CT scan of the head?Masses may be hyperdense because of the presence of acute blood, calcification, dense cellularity (lymphoma, meningioma, medulloblastoma, and germinoma), or proteinaceous material.
25. What is the most common tumor in the cerebellopontine angle cistern?Most tumors in the cerebellopontine angle cistern are vestibular schwannomas (75%), followed by meningiomas (10%) and epidermoid tumors (5%). Uncommon neoplasms that may involve the cerebellopontine angle include metastatic disease, facial nerve schwannoma, exophytic brainstem glioma, and hemangioma. Non-neoplastic lesions that may occur include aneurysms arising from the vertebrobasilar arteries, arachnoid cysts, and lipomas. On imaging, small vestibular schwannomas are usually isolated to the internal auditory canal (IAC), isointense to brain parenchyma, and homogeneously enhanced. Contrast-enhanced MRI is commonly necessary to detect them. Larger tumors are usually heterogeneous because of the development of cystic or necrotic areas (or both), and they cause expansion of the porus acusticus (the opening of the IAC) (Fig. 48-6). Of vestibular schwannomas, 85% involve the IAC. In contrast, meningiomas rarely involve the IAC (5%), they usually enhance homogeneously, and there is usually associated dural enhancement. It is important for the radiologist to try to distinguish schwannoma from meningioma because this information can affect the surgical approach in resecting these lesions.
26. What is the most common clinical presentation of a vestibular schwannoma?The most common clinical presentation of a vestibular schwannoma is unilateral sensorineural hearing loss. Adults with unilateral sensorineural hearing loss should be evaluated with enhanced MRI. Conductive hearing loss is usually evaluated with temporal bone CT to assess for an abnormality of the ossicles and middle ear. In children, temporal bone CT is commonly the first imaging modality used to assess sensorineural and conductive hearing loss because the sensorineural hearing loss in pediatric patients is often related to congenital malformations easily detected on CT.
27. Define transtentorial herniation.To understand this, one must appreciate important central anatomy. The medial temporal lobes (uncus, hippocampus) overhang the tentorium; the brainstem passes through the tentorial hiatus; the posterior cerebral arteries course around the brainstem and medial to the temporal lobes; and the third cranial nerves originate from the midbrain, crossing the interpeduncular cistern below the posterior cerebral arteries and medial to the medial lobes. Transtentorial herniation is caused by a mass effect with a vector force that is directed inferiorly and medially. The temporal lobe shifts over the tentorium, resulting in compression of the third nerve (leading to ipsilateral papillary dilation), posterior cerebral arteries, and midbrain. Compression of the contralateral cerebral peduncle against the tentorium produces ipsilateral motor weakness, referred to as the “Kernohan-Woltman notch” phenomenon (false localizing sign).
28. What is the most common posterior fossa/infratentorial mass in adults?The most common infratentorial neoplasm in adults is a metastasis. A metastasis appears as a well-defined, enhancing mass at the gray-white junction and may have surrounding vasogenic edema. The most common primary posterior fossa tumor in adults is a hemangioblastoma. The typical imaging findings of hemangioblastoma are a cystic mass with an enhancing mural nodule (Fig. 48-7). The mural nodule is highly vascular. Solidly enhancing hemangioblastomas can also be seen, however. Multiple hemangioblastomas are associated with von Hippel-Lindau disease.

334 Brain: anatomy, trauma, and tumors
A B
Figure 48-7. Hemangioblastoma. A, Axial T1-weighted MR image shows T2 hyperintense, cystic, midline cerebellar mass with a small mural nodule (arrow). There is mass effect on the fourth ventricle. B, Coronal T1-weighted postcontrast image shows that the mural nodule is intensely enhancing (arrow).
29. What are the three parts of the anterior lobe of the pituitary gland?The pituitary gland is composed of two physiologically and anatomically distinct lobes—anterior and posterior. The anterior lobe, or adenohypophysis, represents 75% of the volume of the gland and is divided into the pars tuberalis, pars intermedia, and the pars distalis. The posterior lobe, or neurohypophysis, is composed of the posterior pituitary lobe, the infundibular stalk, and median eminence of the hypothalamus. Microadenomas are the most common intrasellar neoplasm in adults. Microadenomas are defined as neoplasms that are 10 mm or smaller. They are hypointense relative to the pituitary gland on unenhanced and enhanced T1-weighted MRI (Fig. 48-8A). Autopsy series indicate that small, incidental lesions of the pituitary gland are common. Clinical correlation is crucial so that insignificant lesions (e.g., cysts) are not treated. In about 75% of cases, microadenomas have associated hormonal abnormalities.
A B
Figure 48-8. A, Pituitary microadenoma. Enhanced coronal T1-weighted MR image through the sella turcica shows a small, round lesion in the right lateral aspect of the pituitary gland (arrow). B, Pituitary macroadenoma. Coronal enhanced T1-weighted image shows large mass centered within the pituitary sella and extending into the suprasellar space. Despite its large size, the mass is not compressing the optic chiasm (arrow).

Brain: anatomy, trauma, and tumors 335neuroradiology
A B
Figure 48-9. Pineoblastoma. A, Sagittal T1-weighted MR image shows mass in the region of the pineal gland (asterisk) that compresses the tectum (arrow). B, Enhanced coronal T1-weighted image shows intense enhancement of the mass.
Macroadenomas are larger than 10 mm, enlarge the sella turcica, and commonly spread outside of the sella into the suprasellar cistern or cavernous sinus. As a result, patients with macroadenomas often present with visual symptoms (classically, bitemporal hemianopsia) related to compression of the optic chiasm and prechiasmatic optic nerves (Fig. 48-8B), headache, and other cranial nerve palsies.
30. Name newer imaging techniques that help diagnose brain tumors.These techniques include magnetic resonance spectroscopy, perfusion MRI, and diffusion MRI. Functional MRI is used for preoperative localization of eloquent brain cortex before surgery.
31. Pineal region masses are associated with what visual disturbance?The clinical manifestations of pineal region masses depend on their size and location near critical anatomic structures—the aqueduct of Sylvius, the tectal plate, and the vein of Galen/internal cerebral veins. Pineal region masses may cause paresis of upward gaze (Parinaud syndrome) because of compression of the tectal plate or obstructive hydrocephalus because of compression of the aqueduct. Pineal region tumors are categorized into tumors of germ cell origin (60%) and tumors of pineal cell origin. Most of these tumors arise from germ cells, are seen in male patients, and are germinomas. Intrinsic pineal cell tumors (pineocytoma and pineoblastomas) are seen in male and female patients equally. CSF seeding is common. Because pineal tumors are commonly hypercellular, they appear hyperdense on unenhanced CT, and they are intermediate in signal intensity on T1-weighted and T2-weighted MRI (Fig. 48-9).
BiBliography
[1] S.J. Nelson, T.R. McKnight, R.G. Henry, Characterization of untreated gliomas by magnetic resonance spectroscopic imaging, Neuroimaging Clin. N. Am. 12 (2002) 599–613.
[2] P.E. Ricci, Imaging of adult brain tumors, Neuroimaging Clin. N. Am. 9 (1999) 651–669. [3] J.G. Smirniotopoulos, The new WHO classification of brain tumors, Neuroimaging Clin. N. Am. 9 (1999) 595–613. [4] C.D. Wiginton, B. Kelly, A. Oto, et al., Gadolinium-based contrast exposure, nephrogenic systemic fibrosis, and gadolinium detection
in tissue, AJR. Am. J. Roentgenol. 190 (2008) 1060–1068.