2011 junecb managementtreeendocrinology
-
Upload
minakata-jin -
Category
Education
-
view
80 -
download
0
description
Transcript of 2011 junecb managementtreeendocrinology

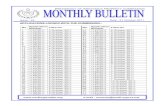
Trilostane Treatment for CaninePituitary-Dependent Hyperadrenocorticism
Ellen Behrend, VMD, PhD, Diplomate ACVIMAuburn University
Managemen t Tre e / ENDOCRINOLOGY Peer Reviewed
Investigation
Diagnosis
Treatment
ResultACTH = adrenocorticotropic hormone, stim = stimulation
This algorithm can be downloaded from cliniciansbrief.com and printed for use in your clinic.
Trilostane• 2 mg/kg Q 24 H OR • 1 mg/kg Q 12 H
• Decreased appetite, vomiting, diarrhea, listless-ness or water intake < 60 mL/kg Q 24 HOR• After 10–14 days of treatment
• Run ACTH stim test beginning 4–6 H aftertrilostane administration• Check with your reference laboratory for “idealrange”; it is approximately 30–150 nmol/L or1–5 mcg/dL pre- and post-ACTH stim testing
Response below ideal Response ideal Response above ideal
• Discontinue for 2–3 days• Restart medication at 25%lower dose• Recheck ACTH stim test in 7days
OR• Recheck ACTH stim test in 3days• Restart medication at 25%lower dose when cortisol levelis ideal or higher
• Continuetherapy• Recheck ACTHstim test at 30days and, ifdoing well, at90 days; thenevery 90–120days, if signsrecur, or if signsof cortisol insuf-ficiency arepresent
Clinical signscontrolled
Clinical signspresent
• On day 30 orbeyond? If giv-ing Q 24 H,then halve thedose and giveQ 12 H• Recheck ACTHstim test after10 days
• If on recheck ACTH stim test atday 10–14, cortisol concentra-tions are lower or clinical signsimproved, then maintain doseand recheck ACTH stim testagain at day 30
• If recheck ACTH stim test resultsstill above ideal after > 30 dayson therapy or at day 10–14 noimprovement was noted,increase dose 25%; recheckACTH stim test in 7 days
See Aids & Resources,back page, for references& suggested reading.
Clinical signspresent
32 ........................................................................................................................................................................NAVC Clinician’s Brief / June 2011 / Management Tree

![[XLS] · Web view2011 1/3/2011 1/3/2011 1/5/2011 1/7/2011 1/7/2011 1/7/2011 1/7/2011 1/7/2011 1/7/2011 1/7/2011 1/7/2011 1/7/2011 1/11/2011 1/11/2011 1/11/2011 1/11/2011 1/11/2011](https://static.fdocuments.net/doc/165x107/5b3f90027f8b9aff118c4b4e/xls-web-view2011-132011-132011-152011-172011-172011-172011-172011.jpg)




![[GESTIÓN+MEDICIÓN=PROGRESO] · 2015-12-03 · 3 Dic ’ 2010’ Ene’ 2011’ Feb’ 2011’ Mar’ 2011’ Abr’ 2011’ May’ 2011’ Jun’ 2011’ Jul’’ 2011’ Ago’](https://static.fdocuments.net/doc/165x107/5ecede15b16df948656232b5/gestinmedicinprogreso-2015-12-03-3-dic-a-2010a-enea-2011a-feba.jpg)











