2010 - Ji Et Al - J Neuroscience
-
Upload
galhardopapers -
Category
Documents
-
view
216 -
download
0
Transcript of 2010 - Ji Et Al - J Neuroscience
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
1/14
Behavioral/Systems/Cognitive
Cognitive Impairment in Pain through Amygdala-Driven
Prefrontal Cortical Deactivation
Guangchen Ji,1 Hao Sun,1 YuFu,1 Zhen Li,1 MiguelPais-Vieira,2 VascoGalhardo,2 andVolkerNeugebauer11Department of Neuroscience and Cell Biology, The University of Texas Medical Branch, Galveston, Texas 77555-1069, and 2Instituto de Histologia e
Embriologia, Faculdade de Medicina, and Instituto de Biologia Molecular e Celular, Universidade do Porto, 4200-319, Porto, Portugal
Cognitive deficits such as impaired decision-making can be a consequence of persistent pain. Normal functions of the intact amygdalaand prefrontalcortex are required for emotion-based decision-makingthat relies on the ability to assess risk, attributevalue,and identify
advantageousstrategies.We tested the hypothesisthat pain-related cognitivedeficitsresult fromamygdala-drivenimpairment of medial
prefrontal cortical (mPFC) function. To do this, we used electrophysiological single-unit recordingsin vivo
, patch clamp in brain slices,and various behavioral assays to show that increased neuronal activity in the amygdala in an animal model of arthritis pain wasaccompanied by decreased mPFC activation and impaired decision-making. Furthermore, pharmacologic inhibition (with a
corticotropin-releasing factor 1 receptor antagonist) of pain-related hyperactivity in the basolateral amygdala (BLA), but not centralamygdala (CeA), reversed deactivation of mPFC pyramidal cells and improved decision-making deficits. Pain-related cortical deactiva-
tion resulted from a shift of balance between inhibitory and excitatory synaptic transmission. Direct excitatory transmission to mPFCpyramidal cellsdid not change in the pain model, whereas polysynaptic inhibitorytransmission increased.GABAergictransmission was
reduced by non-NMDA receptor antagonists,suggesting that synaptic inhibition was glutamate driven. The results are consistent with amodel of BLA-driven feedforward inhibition of mPFC neurons. In contrast to the differential effects of BLA versus CeA hyperactivity on
cortical-cognitivefunctions,both amygdala nucleimodulateemotional-affectivepain behavior.Thus,this studyshows thatthe amygdalacontributesnot onlyto emotional-affectivebut alsocognitiveeffects of pain.The novelamygdalo-cortical painmechanismhas important
implications for our understanding of amygdala functions and amygdalo-cortical interactions.
IntroductionDecision-making represents a critical cognitive function that re-quires the integration of sensory, affective, and cognitive pro-cesses (Bechara et al., 1999; Paulus, 2007; Seymour and Dolan,2008). A strong emotional stimulus, pain, can impair decision-making in humans (Apkarian et al., 2004b) and animals (Pais-Vieira et al., 2009). The underlying mechanism remains to bedetermined, but recent evidence suggests that dysfunction of pre-frontal cortical (PFC) areas is involved (Apkarian et al., 2004a;Metz et al., 2009). The PFC, particularly its medial and orbitalregions, plays a key role in value-based decision-making that
avoids risky choices and guides advantageous goal-directed be-haviors in animals and humans (Bechara et al., 1999; Vertes,2006; Stalnakeret al., 2007a;Kouneiher et al., 2009).PatientswithPFC lesions (Bechara et al., 1999) show similar deficits in anemotion-based decision-making task as pain patients (Apkarian
et al., 2004b). They perseverate in making disadvantageouschoices that yield high immediate monetary gains at the risk ofhigher future losses in a gambling task.
Advantageous decision-making in the gambling task requiresalso the intact amygdala (Bechara et al., 1999, 2003), a key playerin emotions and affective disorders (Maren and Quirk, 2004;Phelps and LeDoux, 2005; Seymour and Dolan, 2008; Ehrlich etal., 2009). The amygdala consists of several functionally distinctnuclei, including the lateral (LA), basolateral (BLA), and central(CeA) nuclei (Sah et al., 2003). Associative processing in theLABLA networkattachesemotional significance to sensorystimuli.
Affect-relatedinformationis thentransmittedto theCeAto regulatebehavioral responses through interactions with hypothalamus andbrainstem (Maren andQuirk, 2004; Phelps andLeDoux, 2005; Ehr-lich et al., 2009). The amygdalacanalso modulate cortical functionsand interactions between BLA and medial PFC (mPFC) are impor-tant for emotional associative learning and behavior (Garcia et al.,1999; Holland and Gallagher, 2004; McGaugh, 2004; Laviolette andGrace, 2006; Herry et al., 2008; Roozendaal et al., 2009).
Recent work from our group and others showed that pain-related plasticity in the CeA contributes critically to theemotional-affective component of pain (Neugebauer et al., 2004,2009; Carrasquillo and Gereau, 2007; Ikeda et al., 2007; Myers andGreenwood-Van Meerveld, 2007). Less is known about the role of
the BLA in pain. Although the BLA receives polymodal, includingnociceptive, information (Neugebauer et al., 2009) and has beenimplicated in top-down pain modulation (McGaraughty and
Received Jan. 14, 2010; revised Feb. 22, 2010; accepted March 4, 2010.
This work was supported by National Institute of Neurological Disorders and Stroke Grants NS-38261 and
NS-11255. We thank Drs. Richard E. Coggeshall and William D. Willis Jr. (University of Texas Medical Branch,
Galveston,TX)and Dr.Brad Keele(BaylorUniversity, Waco,TX)for criticalreadingof andvaluablecommentson this
manuscript. We also thank Margarida Dourado for excellent technical experimental assistance.
G.J. and H.S. contributed equally to this work.
Correspondence should be addressed to Dr. Volker Neugebauer, Department of Neuroscience and Cell Biology,
The University of Texas Medical Branch, 301 University Boulevard, Galveston, TX 77555-1069. E-mail:
[email protected]:10.1523/JNEUROSCI.0225-10.2010
Copyright 2010 the authors 0270-6474/10/305451-14$15.00/0
The Journal of Neuroscience, April 14, 2010 30(15):54515464 5451
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
2/14
Heinricher, 2002; Jasmin et al., 2003), processing of pain-relatedinformation in the BLA and upstream interactions with corticalareas in pain remain to be determined. Based on the LABLACeA circuitry model of amygdala function in aversive behavior(Sah et al., 2003; Maren and Quirk, 2004; Phelps and LeDoux,2005; Ehrlich et al., 2009), we hypothesized that pain leads tohyperactivity in the BLA, as in the CeA (Neugebauer et al., 2009),
and that both nuclei contribute to emotional-affective aspects ofpain. Different from the CeA, however, the BLA is a major sourceof input to the mPFC (Kita and Kitai, 1990; McDonald, 1991;Bacon et al., 1996; Gabbott et al., 2006). Therefore, we furtherhypothesized that pain-related plasticity in the BLA, but notCeA,impairs mPFC function and produces cognitive decision-makingdeficits.
Materials andMethodsArthritis pain modelA localized mono-arthritis was induced in the left knee joint by intra-articular injections of kaolin (4%, 80100 l) and carrageenan (2%,80100l) through the patellar ligament (Neugebauer et al., 2007). Thistreatment paradigm reliably leads to inflammation and swelling of the
knee within 13 h, reaches a maximum plateau at 5 6 h, and persists fordays (Neugebauer et al., 2007). The 56 h time point was selected fortestingdrug effects, behavioral assays, andobtaining brain slices for elec-trophysiology. Details of the kaolincarrageenan arthritis pain modelhave been given previously (Neugebauer et al., 2007).
Electrophysiologyin vivo Animal preparation. Extracellular single-unit recordings were made inpentobarbital-anesthetized adult rats (250350 g) as described previ-ously in detail (Neugebauer and Li, 2003; Ji and Neugebauer, 2007).Animals were kept under anesthesia maintained at a constant level withpentobarbital (15 mg kg1/h1, i.v.). They were paralyzedwith pancu-ronium (0.3 mg/h, i.v.) and artificially ventilated (33.5 ml; 5565strokes/min). End-tidal CO2 levels (kept at 4.0 0.2%), heart rate, andelectrocardiogram pattern were continuously monitored. Core body
temperature was maintained at 37C by means of a homeothermic blan-ket system. These measures ensured a constant internal state of bodyfunctions. Animals were mounted in a stereotaxic frame (David KopfInstruments), and a small unilateral craniotomy was performed at thesutura frontoparietalis level.
Extracellular single-unit recordings. Long-term extracellularrecordingswere made from single neurons in the BLA and medial (prelimbic) PFCwith glass-insulated carbon filament electrodes (35 M), using the fol-lowing stereotaxic coordinates (inmm): posteriorBLA, 2.53.0 caudaltobregma, 4.55.2 lateral to midline, 7.59 depth; prelimbic PFC, 3.0 3.2rostral to bregma, 0.51.0 lateral to midline, 35 depth. Recordings weremade in the right hemisphere to allow comparison with our previousstudiesthat showedpain-related changes in theright,but notleft, centralnucleusof theamygdala(Ji andNeugebauer,2009). Because connectionsbetween BLA and mPFC are predominantly ipsilateral (Bacon et al.,1996; Gabbott et al., 2006), recordings of BLA and mPFC neurons weremade in the same (right) hemisphere. Recorded signals are amplified,displayed on storageoscilloscopes, fed into a window discriminator, dig-itized (1401plus interface; Cambridge Electronic Design), and recordedon a Pentiumpersonalcomputer.Spike2software(version 3; CambridgeElectronic Design) was used for online and offline analysis of single-unitactivity (see next section).
Identification and classification of BLA and mPFC neurons. An individ-ual neuron was identified by the configuration, shape, and height of therecorded action potentials (spikes) that occurred spontaneously (back-ground activity) or in response to mechanical (tissue compression)search stimuli (evoked responses). Spike detection and recoding wasbased on the waveform signal that crossed a trigger level and matched apreset shape or template that was created for theindividual neuronat the
beginning of the recording period.BLA projection neurons were identified by antidromic activation us-
ing square-wave current pulses (50500 A, 150 s) delivered with a
monopolar stimulation electrode inserted into the mPFC, using the fol-lowing coordinates (in mm): 3.2rostral to bregma, 0.8lateral to midline,35 depth of tip. Criteria for antidromic activation were as follows(Neugebauer et al., 1999): constant latency of the evoked spike; ability tofollow high-frequency (333 Hz) stimulation; and collision of ortho-dromic spikes withelectrically evokedantidromic spikes. mPFC pyrami-dal cells were distinguished from inhibitory interneurons based on wellestablished criteria (Constantinidis and Goldman-Rakic, 2002; Lavio-
lette and Grace, 2006), including broader action potential waveform(spike width500 s) and lower baseline discharge rate (10 Hz) .
In each animal, background activityand evokedresponses of oneneu-ronwere recorded.Brief (15s) mechanical test stimuli of innocuous (500g/30 mm2) and noxious (2000 g/30 mm2) intensities were applied to theknee joint by means of a calibrated forceps equipped with a force trans-ducer, whose output signal was amplified, displayed in grams on a liquidcrystal display screen, digitized by the Cambridge Electronic Design in-terface, and recorded on the Pentium personal computer for online andoffline analysis (Ji and Neugebauer, 2007). For the analysis of net evokedactivity, background activity precedingthe stimuluswas subtractedfromthe total activity during stimulation. To determine changes in the arthri-tis pain model, one and the same neuron was recorded continuouslybefore and after arthritis induction, allowing paired analysis.
Drug application by microdialysis. Drugs were administered into theBLA (or CeA as a control) of the right hemisphere by microdialysis. Amicrodialysis probe [CMA11; (CMA/Microdialysis); membrane diame-ter, 250 m; membrane length, 1 mm; 8 kDa cutoff, sufficient for theapplication of small molecules such as NBI27914 (5-chloro-4-[N-(cyclopropyl)methyl-N-propylamino]-2-methyl-6-(2,4,6-trichlorophenyl)amino-pyridine)] was positioned stereotaxically in thebrain, using the following coordinates (in mm): BLA, 3.3 caudal tobregma, 5.0 lateral to midline, 9.0 depth; CeA, 2.3 caudal to bregma, 4.0lateral to midline, 8.5 depth. The probe was connected to a HarvardApparatus infusion pump and perfused with artificial CSF (ACSF) con-taining the following (in mM): 125.0 NaCl, 2.6 KCl, 2.5 NaH2PO4, 1.3CaCl2, 0.9 MgCl2, 21.0 NaHCO3, and 3.5 glucose, oxygenated and equil-ibrated to pH 7.4 (at 5 l/min. Throughout the experiment, ACSF waspumped through the fiber to establish equilibrium in the tissue. Drugs
were administered for20 min.They were dissolved in ACSFon theday ofthe experiment at a concentration 100-fold that predicted to be neededbased on data from our previous microdialysis and in vitro studies anddata in the literature (Ji and Neugebauer, 2007; Fu and Neugebauer,2008). Drug concentrationin the tissue is at least 100 times lower than inthe microdialysis probe as a result of the concentration gradient acrossthe dialysis membrane and diffusion in the tissue (Ji and Neugebauer,2007). Numbers in the text refer to drug concentrations in the microdi-alysis fiber.
Electrophysiology in brain slicesSlice preparation. Brain slices containing the amygdala or mPFC wereobtained from normal (control) and arthritic rats (150250 g) as de-scribedpreviously(Neugebauer et al., 2003; Orozco-Cabal et al.,2006; Fuand Neugebauer, 2008). Coronal brain slices (300500 m) containingthe BLA were cut at 2.53.5 mm caudal to bregma using a vibratingmicrotome. Brain slices containing the PFC were cut at 3.03.2 mmrostral to bregma. At this level, slices contain both the prelimbic cortex(recording site) and infralimbic cortex (stimulation of BLA afferentspassing through). A single brain slice was transferred to the recordingchamber andsubmergedin ACSF(31 1C), which superfusedthe sliceat2 ml/min.ACSF containedthe following (inmM): 117 NaCl, 4.7KCl,1.2 NaH2PO4, 2.5 CaCl2, 1.2 MgCl2, 25 NaHCO3, and 11 glucose. TheACSF was oxygenated and equilibrated to pH 7.4 with a mixture of 95%O2/5% CO2. Only one or two brain slices per animal were used, oneneuronwas recordedin each slice, and a fresh slicewas used for each newexperimental protocol. Numbers in the text refer to the number of neu-rons tested for each parameter.
Patch-clamp recording. Whole-cell patch-clamp recordings were ob-
tained from BLA neurons using the blind-patch technique and fromvisualized PFC neurons using infrared differential interference contrast(DIC) video microscopy. Recordings were made in theright hemisphere.
5452 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions in Pain
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
3/14
The boundaries of the different amygdalar nuclei are easily discernedunder light microscopy (Fu and Neugebauer, 2008). Pyramidal cells inthe mPFC were visualized in layer V (700m lateral to the interhemi-spheric fissure). Pyramidal cells in the BLA were identified by their ac-commodation properties to a sustained depolarizing intracellularcurrent injection (Sah et al., 2003). Recording pipettes (35 M tipresistance) made from borosilicate glass were filled with intracellular solu-tion containing thefollowing (inmM): 122 K-gluconate,5 NaCl,0.3 CaCl2, 2
MgCl2, 1 EGTA, 10 HEPES, 5 Na2-ATP, and 0.4 Na3-GTP, pH adjusted to7.27.3 with KOH (osmolarity adjusted to 280 mOsm/kg with sucrose).Data acquisition and analysis of voltage and current signals wasdoneusing adualfour-poleBesselfilter(WarnerInstruments),a low-noiseDigidata1322interface (Molecular Devices), an Axoclamp-2B amplifier (Molecular De-vices), a Pentium personal computer, and pClamp9 software (MolecularDevices). Head-stage voltage was monitored continuously on an oscillo-scope to ensure precise performance of the amplifier. Neurons were voltageclamped at 70 or 0 mV (reversal potential of EPSCs) for the study ofexcitatory and inhibitory transmission, respectively. High (gigaohm) sealand low series (20 M) resistances were checked throughout the experi-ment (using pClamp9 membrane test function) to ensure high-qualityrecordings.
Synaptic transmission. Using concentric bipolar stimulating electrodes(David Kopf Instruments), EPSCs were evoked in BLA neurons by focalelectricalstimulation(Grass Instruments S88 stimulator) of inputs from thelateral amygdala. EPSCs and IPSCs were evoked in PFC neurons by focalelectrical stimulation (150 s square-wave pulses) of presumed BLA affer-ents in the infralimbic cortex as described by the Gallagher group (Orozco-Cabal et al., 2006). Thestimulating electrodewas placed in layer V (500mfrom the medial surface of the slice) of the infralimbic cortex in which BLAafferents were identified by the fluorescent signal originating fromanterogradely labeled fibers after stereotaxic injections of a fluorescent tracer[1,1-dioctadecyl-3,3,3,3-tetramethylindocarbocyanine perchlorate (DiI) (In-vitrogen); dissolved in N,N-dimethylformamide dimethyl acetal (Sigma-Al-drich); 2l at40 nl/min) intothe BLA (same coordinates as for microdialysisprobes) 1012 d before brain tissue was taken. The distance betweenstimulation and recording sites was 600 800m.
Spontaneous and miniature (in 1 M TTX) EPSCs and IPSCs were
recorded at70 and 0 mV, respectively, as described previously (Fu andNeugebauer, 2008). A fixed length of traces (5 min) was analyzed forfrequency and amplitude distributions using MiniAnalysis program 5.3(Synaptosoft).The root mean square(RMS)of thebackground noise wascomputed for each set of data. The detection threshold for an event wasset to three to four times the RMS value. Peaks were detected automati-cally, but each detected event was then visually inspected to prevent theinclusion of false data.
Drug application. Drugs were applied by gravity-driven superfusion ofthebrainsliceintheACSF(2 ml/min). Solution flowinto therecordingchamber (1 ml volume) was controlled with a three-way stopcock.
Behavioral testsSpinal reflexes. Thresholds of hindlimb withdrawal reflexes evoked bymechanical stimulation of the knee joint were measured as describedpreviously (Neugebauer et al., 2007). Mechanical stimuli of continuouslyincreasing intensity were applied to the knee joint using a calibratedforceps (see above, Electrophysiologyin vivo). Withdrawal threshold wasdefined as the minimum stimulus intensity that evoked a withdrawalreflex.
Vocalizations. Audible and ultrasonic vocalizations were recorded andanalyzed as described previously(Neugebaueret al., 2007; Fu andNeuge-bauer, 2008). The experimental setup (United States Patent 7,213,538)included a custom-designed recording chamber, a condenser micro-phone (audible range, 20 Hz to 16 kHz) connected to a preamplifier, anultrasound detector (25 4 kHz), filter and amplifier (UltraVox four-channel system; Noldus Information Technology), and data acquisitionsoftware (UltraVox 2.0; Noldus Information Technology), which auto-matically monitored the occurrence of vocalizations within user-defined
frequencies and recorded number and duration of digitized events (vo-calizations). The computerized recording system was set to suppressnonrelevant audible sounds (background noise) and to ignore ultra-
sounds outside the defined frequency range. Animals were placed inthe recording chamber for acclimation 1 h before the vocalizationmeasurements. Brief (15 s) innocuous (500 g/30 mm 2) and noxious(2000 g/30 mm 2) mechanical stimuli were applied to the knee, usinga calibrated forceps (see above, Electrophysiologyin vivo). The totalduration of vocalizations (arithmetic sum of the duration of individ-ual events) was recorded for 1 min, starting with the onset of themechanical stimulus. Audible and ultrasonic vocalizations reflect su-
praspinally organized nocifensive and affective responses to aversivestimuli (Neugebauer et al., 2007).
Plus-maze test. Anxiety-like behavior was measured in the elevatedplus-maze test as a decrease of open-arm choices (ratio of open-armentries to the total number of entries expressed as percentage), using acomputerized recording and analysis system (Multi-Varimex version1.00; Columbus Instruments) as described previously (Ji et al., 2007).Entries were measured every 5 min for a total observation period of 45min. Open-arm ratio during the first 5 min period was used for theassessment of anxiety-like behavior (Walf and Frye, 2007).
Gambling task. Decision-making was measured in a behavioral task(Pais-Vieira et al., 2007, 2009; Neugebauer et al., 2009) using a custom-designed computerized behavioral system (Coulbourn Instruments).The system included a behavioral arena (octagon) with two levers oneach side for automated delivery of chocolate-coated food pellets (Re-search Diets). The levers were separated by a Plexiglas divider so that theanimal needed to make a choice between the two sides/levers. A runwayconnected to the octagon by an automated guillotine door housed theanimal briefly (10 s) between each trial. The rat was given 20 s to choosebetween two levers to recover a food reward in 90 consecutive trials: onelever released three food pellets only in 3 of 10trials (high risk); the otherlever gave one food pellet in 9 of 10 trials (low risk). The side of thehigh-risk lever remained the same throughout the experiment butchanged randomly between different animals to avoid any lateralizationbias. Main outcome measure was the preference index defined as theproportion of choices between the levers during the gambling task. Pref-erence index was calculated for each group of 10 consecutive trials usingthe formula: (low-risk lever choices high-risk lever choices)/numberof completed trials. A negative preference index reflects high-risk
decision-making.Drug application by microdialysis in awake behaving animals. As de-
scribedin detailpreviously (Jiet al., 2007;Neugebauer et al., 2007; Fu andNeugebauer, 2008), a guide cannula was implanted stereotaxically theday before behavioral measurements, using a stereotaxic apparatus(David Kopf Instruments). The animal was anesthetized with pentobar-bital sodium (Nembutal, 50 mg/kg, i.p.), and a small unilateral craniot-omy was performed at the sutura frontoparietalis level. The guidecannula was implanted on the dorsal margin of the BLA or CeA in theright hemisphere, using the following coordinates (in mm): BLA, 3.5caudal to bregma, 5.0 lateral to midline, 7.0 depth; CeA, 2.0 caudal tobregma, 4.0 lateral to midline, 7.5 depth. The cannula was fixed to theskull with dental acrylic (Plastics One). Antibiotic ointment was appliedto the exposed tissue to prevent infection. On the day of the experiment,a microdialysis probe (CMA/11; see above, Electrophysiology in vivo)
was inserted through the guide cannula so that the probe protruded by 1mm. The probe was connected to a Harvard Apparatus infusion pumpandperfused withACSF (oxygenated andequilibratedto pH 7.4). Beforeeach drug application, ACSF was pumped through the fiber for at least1 h to establish equilibrium in the tissue. Drugs were dissolved in ACSFon theday of theexperiment at a concentration100-foldthatpredicted tobe neededbecause of theconcentrationgradientacross thedialysis mem-brane and diffusion in the tissue (see above, Electrophysiology in vivo).Numbers in the text refer to drug concentrations in the microdialysisfiber.
DrugsThe following selective compounds purchased from Tocris Bioscience wereused: NBI27914 [selective non-peptide corticotropin-releasing factor 1 (CRF1)
receptor antagonist (Ji et al., 2007; Fu and Neugebauer, 2008)]; DL-2-amino-5-phosphonopentanoic acid (AP-5) (NMDA receptor antag-onist); 2,3-dioxo-6-nitro-1,2,3,4-tetrahydrobenzo[ f]quinoxaline-7-
Ji et al. Amygdalo-Cortical Interactions in Pain J. Neurosci., April 14, 2010 30(15):54515464 5453
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
4/14
sulfonamide disodium salt (NBQX) (non-NMDA receptor antago-nist); 6-cyano-7-nitroquinoxaline-2,3-dione disodium salt (CNQX)(non-NMDA receptor antagonist); and bicuculline ([R-(R*,S*)]-6-(5,6,7,8-tetrahydro-6-methyl-1,3-dioxolo[4,5-g]isoquinolin-5-yl)furo[3,4-e]-1,3-benzodioxol-8(6H)-one) (GABAA receptor antagonist). Drugswere dissolvedin ACSF on theday of theexperiment. ACSF servedas vehiclecontrol in all experiments.
Adrenocorticotropic hormone (ACTH) (Synacthen Depot, Novartis
Portugal) was used for the assessment of hypothalamicpituitaryadre-nal (HPA) axis influences on anxiety-likeand decision-making behaviors(see Fig. 4).
HistologyAt the end of an electrophysiological in vivo experiment, direct current(250 A, 3 min) was passed through the recording electrode to create asmall lesion to mark the recording site. The brain was removed andsubmerged in 10%Formalin andpotassiumferrocyanide. At theend of abehavioral experiment, the animal was killed,and thebrain was removedand submerged in 10% Formalin. Tissues were stored in 20% sucrosebefore they were frozen sectioned at 50 m. Sections were stained withNeutral Red, mounted on gel-coated slides, and coverslipped. Positionsof the microdialysis fibers and lesion/recording sites were identified un-der the microscope and plotted on standard diagrams (Ji et al., 2007; Fu
and Neugebauer, 2008).
Statistical analysisAll averaged values are given as the mean SE. Statistical significancewas accepted at the level p 0.05. Prism 3.0 software (GraphPad Soft-ware) was used for all statistical analyses. For multiple comparisons,one-way ANOVA or two-way ANOVA was used with appropriate posthoc tests as indicated in the text and figure legends (Dunnetts test tocompare all sets of data to a control value, Tukeys post hoctest to com-pare all pairs of data; and Bonferronis test to compare selected pairs ofdata).Students ttest (paired or unpaired when appropriate) was used tocompare two sets of data that have Gaussian distribution and similarvariances (Prism 3.0 software; GraphPad Software).
ResultsPain-related plasticity in the BLAAs a first step in the analysis of amygdalo-cortical interactions inpain, we determined pain-related functional changes in the BLA.Extracellular single-unit recordings in anesthetized rats weremade from individual BLA neurons (see location in Fig. 1e,f)before and after the induction of a localized arthritis in one kneejoint by intra-articular injection of kaolin and carrageenan (seeMaterials and Methods) (Neugebauer et al., 2007). BLA neuronswere activatedby antidromic stimulation in themPFC(Fig.1b,g).Only one neuron was studied in each animal. Focus on a homog-enous population of BLA projection neurons and use of a pairedexperimental paradigm in which each neuron serves as its owncontrol form a highly sensitive assay that allows the detection of
significant changes with relatively small numbers of animals anddata points (Neugebauer and Li, 2003; Ji and Neugebauer, 2007).
Like CeA neurons (Neugebauer et al., 2004), BLA neurons withsomatosensory receptive fields responded more strongly to noxiousthan innocuous stimuli (mechanical compression of peripheral tis-sue; n6 neurons). These neuronsrepresent so-called multirecep-tive neurons based on the classification of nociceptive amygdalaneurons (Neugebauer et al., 2004). After arthritis induction, back-ground activity and responses to innocuous (500 g/30 mm2) andnoxious (2000 g/30 mm2) stimulation of the knee increased signifi-cantly and reached a maximum plateau after 5 h (Fig. 1, see timecourse in a and summary data in c) (n 6 neurons; q(10) 5.739,background; q(10) 8.792, innocuous; q(10) 8.812, noxious; p
0.010.001, Tukeys multiple comparison test).Next we examined whether increased responsiveness was at-tributable to enhanced synaptic transmission and excitability
changes in BLA neurons. Whole-cell patch-clamp recordingswere made in brain slices from normal rats and from rats witharthritis (56 h after induction of kaolin/carrageenanarthritis). The56htimepointwasselectedasinourpreviousstudies(Neugebaueret al., 2003, 2004; Fu and Neugebauer, 2008) because continuousrecordings in vivo (Neugebauer and Li, 2003; Neugebauer et al.,2004; Ji and Neugebauer, 2007) show that neuronal changes reach a
maximum plateau at this stage (Fig. 1a).BLA neurons in slices from normal and from arthritic ratsselected for this study showed marked spike frequency accom-modation in response to intracellular injection of a depolarizingcurrent (200 pA, 500 ms) (Fig. 2a), suggesting that the same celltype was compared. Spike accommodation is a defining propertyof pyramidalneurons that constitute thepredominant cell type inthe BLA and function as projection neurons in this region of theamygdala (Washburn andMoises, 1992; Sah et al., 2003). BLA neu-ronsfromarthriticrats(n7neurons)hadahigheractionpotentialfiring rate and lower spike threshold than control neurons (n 10)fromnormal animals(Fig. 2a) (p0.001, F(1,105)18.18, two-wayANOVA), which is consistent with increased neuronal excitability.
Increased synaptic transmission was also measured in slicesfrom arthritic rats compared with controls (Fig. 2b). Monosyn-aptic EPSCs were evoked by electrical stimulation in the LA. TheLABLA synapse is part of the amygdala circuitry involved inaversive behavior (Sah et al., 2003; Maren and Quirk, 2004;Phelps and LeDoux, 2005; Ehrlich et al., 2009). EPSCs were me-diated by non-NMDA receptors because they were completelyblocked with CNQX (20M) (data not shown). Only one neuronwas recorded in each slice, and only one slice was used from eachanimal. Inputoutput (I/O) function of excitatory transmissionat the LABLA synapse was significantly increased in slices fromarthritic rats (n 5 neurons) compared with normal controls(n 5 neurons; p 0.001, F(1,88) 233.75, two-way ANOVA)(Fig. 2b). I/Ofunctionis a well accepted measure of thesensitivity
of a neuron to synaptic inputs (Carvalho and Buonomano, 2009)and has been used successfully in our previous studies to deter-mine synaptic plasticity in ex vivo slice preparations in differentdisease models (Neugebauer et al., 1997, 2000, 2003; Bird et al.,2005; Fu and Neugebauer, 2008).
Neural changes are not observed in slices from sham animalswith intra-articular saline injections (Neugebauer et al., 2003),suggesting that synaptic and excitability changes in slices fromarthriticrats are the resultof the arthriticlesion in the knee in thispain model. The results demonstrate pain-related synaptic plas-ticity in the BLA, as we showed before in the CeA (Neugebauer etal., 2004, 2009), because synaptic facilitation is preserved in thebrain slice preparation independently of continued input from
the site of injury (arthritic knee).
Blockade of CRF1 receptors restores normal activity inthe BLATo determine the correlation of neuronal activity in BLA withcortical function and behavior, we examined whether a selectiveantagonist for corticotropin-releasing factor 1 (CRF1) receptor(NBI27914) could be used to deactivate the BLA. CRF1 receptorwas targeted because of its critical contribution to pain-relatedplasticity, but not normal processing, in the CeA as shown in ourprevious studies (Ji and Neugebauer, 2007; Fu and Neugebauer,2008). CRF1 receptor activation is also important for BLA plas-ticity related to anxiety (Rainnie et al., 2004). However, pain-
related CRF1 receptor function in the BLA has not been shown.Here we tested the hypothesis that CRF1 receptor is critical forpain-related plasticity in the BLA.
5454 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions in Pain
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
5/14
Administration of a CRF1 antagonist (NBI27914, 10M, con-centration in microdialysis fiber; 20 min) into the BLA by micro-dialysis 56 h after arthritis induction inhibited background andevoked activity significantly (Fig. 1, see individual neuron in aand summary data in c,e) (n 6 neurons; q(10) 5.991, back-ground; q(10) 9.293, innocuous; q(10) 8.664, noxious; p 0.010.001, Tukeys multiple comparison test). Importantly, ad-ministration of NBI27914 into the CeA as a control for drugdiffusion had no effect on BLA neurons 56 h after arthritis
induction (Fig. 1d,f) (n
5 neurons; t(4)
0.3900, background;t(4) 0.6038, innocuous; t(4) 1.568; p 0.05, paired ttest) butinhibited pain-related sensitization of CeA neurons in our previ-
ous study (Ji and Neugebauer, 2007). Thedata suggest that inhibition of BLA activ-ity resulted from CRF1 receptor blockadein the BLA.
To determine the synaptic site of CRF1receptor action in the BLA, we tested theeffect of NBI27914 on evoked and minia-
ture EPSCs (Fig. 2).NBI27914 (500 nM; 15min) inhibited synaptic plasticity in BLAneurons in slices from arthritic rats (Fig.2b) (n 5 neurons; p 0.001, F(1,88) 37.97, two-way ANOVA) but had no sig-nificant effect under normal conditions(n 5 neurons; p 0.05, F(1,88) 4.89,two-way ANOVA). NBI27914 (500nM; 15min) decreased amplitude (Fig. 2f) butnot frequency (Fig. 2e) of miniatureEPSCs (in 1 M TTX) (original traces inFig. 2c,d) significantly (cumulative ampli-tude distribution,p 0.05, KolmogorovSmirnov test; mean amplitude, p 0.01,paired t test; n 8 neurons). MiniatureEPSC analysis wasdone only in slicesfromarthritic rats (obtained 56 h after induc-tion) because NBI27914 had no effect onbaseline synaptic transmission in slicesfrom normal animals (Fig. 2b). The dataare consistent with a postsynaptic actionon BLA neurons as shown previously inthe CeA (Fu and Neugebauer, 2008).
The pharmacological data show thatpostsynaptic CRF1 receptors contributeto synaptic facilitation and are useful tar-gets to restore normal activity in the BLA
(present study) or in the CeA (Ji andNeugebauer, 2007; Fu and Neugebauer,2008) in the arthritis pain model.
Pharmacologic deactivation of BLAinhibits pain responsesUsing the CRF1 receptor antagonist to re-store normal function of the BLA in ourpain model, we determined the contribu-tion of BLA hyperactivity to nocifensiveand affective pain behaviors (Fig. 3).Hindlimb withdrawal thresholds and au-dible vocalizations served as outcome
measures of spinally and supraspinally,respectively, organized nocifensive re-sponses. Ultrasonic vocalizations reflectaffective responses. The elevated plus-
maze test measured anxiety-like behavior. These tests have beenused successfullyin our previous studies to show theinvolvementof the CeA in nocifensive and affective components of arthriticpain (Ji et al., 2007; Neugebauer et al., 2007; Fu and Neugebauer,2008). Baseline values under normal conditions in the absence ofarthritis showed little variability in the sample of animals in thisstudy (Fig. 3a d).
In the arthritis pain state (56 h after induction), withdrawalthresholds decreased, indicating increased spinal nocifensive re-
flexes (Fig. 3a) (n
5; p
0.05, Tukeys multiple comparisontest). Duration of audible (Fig. 3c) and ultrasonic (Fig. 3d) vocal-izations increased (n 6; p 0.001 and p 0.01, respectively,
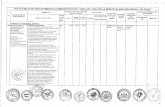
Figure1. Pain-related sensitization of BLAneurons involves CRF1receptors.a,Timecourseofactivitychangesinanindividual
BLA neuron recorded continuously before and after induction of an arthritis pain state (extracellular single-unit recordings in ananesthetizedrat).Eachsymbolshowsbackgroundactivityorresponsestoinnocuousandnoxiousstimuliappliedtothekneejoint.Net evoked activity was calculatedas the differencebetweentotal activity duringstimulation andprecedingbackgroundactivity.Administration of a CRF1 receptor antagonist (NBI27914, 10 M, concentration in microdialysis fiber) into the BLA inhibited theincreased activity in the pain state. b, Antidromic activation of BLA neuron by electrical stimulation in the prelimbic cortex (seeMaterials and Methods). Top, Six superimposed traces show constant latency of evoked spike; bottom, spikes follow high-frequencystimulation. * denotes stimulus artifact. c,Significanteffectsofarthritis( n 6)andNBI27914(n 6)inthesampleofneurons(Tukeysmultiplecomparisontest).Foreachneuron,twotothreevalueswereaveragedbeforearthritisinduction,56hafter induction, and during NBI27914 (15 min). d, Control administrations of NBI27914 into the CeA had no effect on BLAneurons(n 5; pairedttest). Bar histogramsin cand dshow mean SE;ns,notsignificant;**,##p 0.01,*** ,###p 0.001,compared withnormal and predrug, respectively. e, f, Recordingsitesin theBLA andpositions of microdialysis probesin theBLA
(e)andCeA(f).Numbersindicatedistanceposteriortobregma.g,StimulationsiteinthemPFC.Numberindicatesdistanceanteriorto bregma. Scale bars, 1 mm.
Ji et al. Amygdalo-Cortical Interactions in Pain J. Neurosci., April 14, 2010 30(15):54515464 5455
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
6/14
Tukeys multiple comparison test). Ani-mals spent less time exploring the openarm of the plus maze, which is consistentwith anxiety-like behavior (Fig. 3b) (n 5; p 0.001, Tukeys multiple compari-son test). Deactivation of the BLA withNBI27914 (10 M, 1520 min) reversed
pain-related changes of spinal reflexes(Fig. 3a) (n 5; p 0.05) and audible(Fig. 3c) and ultrasonic (Fig. 3d) vocaliza-tions (n 6; p 0.001 and p 0.05,respectively, Tukeys multiple compari-son test). NBI27914 also had anxiolytic-like effects in arthritic animals (Fig. 3b)(n 5; p 0.001, Tukeys multiple com-parison test). NBI27914 did not affect be-havioral outcome measures undernormalconditions (Fig. 3a d).
The behavioral effects of NBI27914 inthe BLA were similar to those in the CeAreported in our previous studies (Ji et al.,2007; Fu and Neugebauer, 2008). The re-sults show for the first time that pain-related plasticity in the BLA (this study) aswell as in the CeA (our previous studies)contributes to nocifensive and affectivecomponents of pain behavior, which isconsistent with a serialmodel of amygdalafunction involving BLA to CeA projec-tions to execute behavioral responses (Sahet al., 2003; Phelps and LeDoux, 2005).
Pharmacologic deactivation of BLA, butnot CeA, reverses pain-related
decision-making deficitsNext, we tested the hypothesis that pain-related hyperactivity in the BLA leads tocognitive deficits associatedwith pain, be-cause the BLA isa major sourceof input tothe mPFC, which plays a key role in cog-nitive functions such as decision-makingand avoidance of emotion-based riskychoices (see Introduction). Pain-relatedcognitive impairment was determined ina computerized behavioral task in whichrats decided between high-risk and low-risk strategies (Fig. 3e). This rodent gam-
bling task is based on serial choicesbetween food rewards of different valueand probability (Pais-Vieira et al., 2007,2009). In 90 consecutive trials, a rat entersthe test arena for 20 s to press one of twolevers associated with a food reward be-fore it is returned to the entry chamber.After the non-gambling training phase inwhich each of two levers provided onefood pellet in 9 of 10 visits, animals weretested on decision-making in a single ses-sion of 90 consecutive trials in which onelever was altered to return three pellets in
3 of 10 trials (high-risk choice), whereasthe other lever continued to deliver onepellet in 9 of 10 trials (low-risk choice).
Figure 2. Pain-related changes in BLA neurons involves CRF1receptors. a, Whole-cellcurrent-clamprecordings of action potentials
generatedbyintracellularcurrent injections (500ms)of increasing magnitudeshowsignificantlyincreasedspikefiringrateofBLA neuronsinslicesfromarthriticrats(obtained56hafterinduction; n7neurons)comparedwithnormalcontrols(n10;Bonferronisposthoc
testsaftertwo-wayANOVA;seeResults).SymbolsshowmeanSEnumberofspikesper500msaveragedforeachsampleofneurons. b,Whole-cellvoltage-clamp recordings of monosynapticEPSCsevoked at theLABLAsynapseshow thatinputoutputfunction increasedsignificantly(Bonferronisposthoctestsaftertwo-wayANOVA;seeResults)inslicesfromarthriticrats(obtained56hafterinduction;n5neurons)comparedwithcontrolslicesfromnormalrats( n5 neurons). NBI27914(500 nM;1015min)decreasedEPSCamplitudeinarthritis significantly (n 5 neurons; Bonferronis post hoctests) but had no effect on normal transmission (n 5 neurons). For eachneuron, peak amplitudes of threeto five EPSCsper stimulus intensitywereaveraged. Tracesshowaverages of 8 10evoked EPSCs.c,d,Original tracesof miniatureEPSCs recorded inTTX (1M) beforeand duringapplicationof NBI27914 (500 nM;15min)inaslicefromanarthriticrat (5 h after induction).e, NBI27914had nosignificanteffecton cumulativeintereventintervaldistribution andmean frequencyofminiatureEPSCs(n8neurons;p0.05,pairedttest;barhistograms). f,NBI27914shiftedcumulativeamplitudedistributiontoward
largervalues,increasingmean amplitudesignificantly(n8neurons;p0.01;barhistograms). e,f,BarhistogramsshownmeanSEbeforeandduringNBI27914.* ,#p0.05,** ,##p0.01,***p0.001(comparedwithnormaland predrug,respectively).
5456 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions in Pain
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
7/14
Normal rats (n 5) developed, after 40 trials, a preference
for the low-risk lever that provided smaller but more reliablerewards (Fig. 3e). In contrast, rats with arthritis (56 h afterinduction; n 5) failed to change strategies and perseverated in
preferring the high-risk lever associated with larger but infre-quent rewards, which is reflected in a negative preference index(Fig. 3e). Preference index of arthritic rats was significantly dif-ferent from that of normal rats after 40 trials ( p 0.050.001,Dunnettsmultiplecomparison test foreach group of 10 trials). Asimilar decision-making deficit has been observed in rats withPFC lesions (Pais-Vieira et al., 2007) or chronic pain (Pais-Vieira
et al., 2009). Impaired decision-making was not attributable topain-related motor or attention deficits, because reaching eachlever involved the same movements and choices were not cue-based in this task.
Pharmacologic deactivation of the BLAin arthriticrats (56 hafter induction; n 5) with NBI27914 (10 M, concentration inmicrodialysis fiber; 20 min) restored normal decision-making(Fig. 3e). Preference index of arthritic rats with deactivated BLAwas notsignificantly different from that of normalrats ( p 0.05,Dunnetts multiple comparison test). Administration ofNBI27914 into the BLA of normal rats (n 5) had no effect ontheir performance in the decision-making task, which is consis-tent with the lack of involvement of CRF1 receptor in normalprocessing in the BLA (Fig. 2b).
Importantly, deactivation of the CeA in arthritic rats (56 hafter induction; n 5) with NBI27914 did not restore normaldecision-making, although administration of NBI27914 into theCeA restores normal function of CeA neurons and inhibits no-cifensive and affective behaviors in the arthritis pain model (Jiand Neugebauer, 2007; Fu and Neugebauer, 2008). Preferenceindex of arthritic rats with deactivated CeA was significantly dif-ferent from that of normal rats ( p 0.05 0.001, Dunnetts mul-tiple comparison test). The data suggest that hyperactivity in theBLA, but not CeA, contributes to impaired decision-making inthe arthritis pain model.
Because theCeA canfacilitate theactivation of theHPA axis inresponse to stress (Phelps and LeDoux, 2005; Myers and
Greenwood-Van Meerveld, 2007), we considered the possibilitythat CRF1 receptor antagonist effects were attributable to alter-ations of HPA axis function and stress response. Electrophysio-logical data in this (Figs. 1, 2) and our previous study (Fu andNeugebauer, 2008) show a direct action on amygdala neurons.Differential effects of site-specific antagonist administrationinto BLA and CeA further argue against a generalized actionon the HPA axis. To better understand the contribution ofHPA axis-mediated stress responses to cognitive deficits ob-served in the arthritis pain model, we measured the effect ofACTH treatment on the performance in the gambling task andelevated plus maze (Fig. 4a,b). ACTH challenge is commonlyused to induce rapid increases of corticosterone levels (Mu-
rakami and Takahashi, 1983; Ferreira et al., 2004). Rats treatedwith systemic injections of ACTH (0.2 mg/kg, i.p.) showedsignificantly higher corticosterone blood levels (Fig. 4c) andincreased anxiety-like behavior (Fig. 4b) as expected (Myersand Greenwood-Van Meerveld, 2007) but were not impairedin the decision-making task (Fig. 4a). Preference index ofACTH-treated rats, like that of normal rats, was significantlydifferent from that of arthritic rats ( p 0.01, Dunnetts mul-tiple comparison test). The data strongly suggest that HPAaxis activation and anxiety are not sufficient to explain cogni-tive impairment in pain.
Pain-related deactivation of mPFC neurons is reversed by
deactivation of BLA but not CeAThe medial regions of the PFC are important for emotionalvalue-based decision-making, which is impaired in pain patients
Figure 3. BLA deactivation inhibits nocifensive and affective pain behaviors and restoresimpaireddecision-making.a,AdministrationofaCRF1receptorantagonist(NBI27914,10M;1520min)intothe BLAdecreased hindlimbwithdrawal thresholds inthe arthritispainstate butnot undernormalconditions.Thesameanimals(n5)weretestedbeforeand56hafterarthritisinduction.Foreachanimal, three measurementswere averaged.b, Anxiety-like behaviorwas measuredin the
elevatedplus mazeas decreasedopen-armchoice(ratio of open-armentries to thetotal number ofentriesexpressedas percentage;see Materialsand Methods).Normalanimals(n 15)weretestedwithvehicle (ACSF)administrationinto theBLA andthen assignedto oneof three treatment groups:NB27914 (10M; 1520 min) administration into BLA under normal conditions (n 5), vehicleadministrationintotheBLA56hafterarthritisinduction(n5),andNBI27914administrationintotheBLA56 hafterarthritisinduction(n5).c,d,Vocalizationsintheaudibleandultrasonicrangeweremeasuredinthesameanimalsbeforeand56hafterarthritisinduction( n6).NBI27914(10M;1520min)inhibitedvocalizationsin arthritisbutnotundernormalconditions.Barhistogramsin
adshowmeansSE;twotothreemeasurementswereaveragedforeachanimal.e, Deactivationof the BLA, but not CeA, with NBI27914 (10M, 20 min) restored normal reward-based decision-making in arthritic rats (56 h after induction). Symbols (mean SE) show the preference
index [(low-risk high-risk choices)/number of trials] averaged for 10 consecutive trials ofanimals in five experimental groups (n 5 each). Animals chose between low-risk (1 foodpelletin9 of10 visits)and high-risk(3pelletsin 3 of10 visits)levers.Preference indexof normalanimals and arthritic animals with deactivated BLA was not significantly different. Preferenceindex of arthritic rats with or without deactivated CeA was significantly different from normalanimals. ad, * ,#p 0.05, **p 0.01, *** ,###p 0.001 (compared with normal and pre-drug,respectively;Tukeysmultiplecomparisontest).e, * ,***p 0.05,0.001(comparedwithnormal; Dunnetts multiple comparison test).
Ji et al. Amygdalo-Cortical Interactions in Pain J. Neurosci., April 14, 2010 30(15):54515464 5457
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
8/14
(Apkarian et al., 2004b). Pain-related morphological changeshave been observed in the mPFC of animals (Metz et al., 2009)
and humans (Apkarian et al., 2004a). We tested the hypothesisthat mPFC function is impaired in pain through a mechanismthat involves amygdala hyperactivity (see Introduction).
Extracellular single-unit recordings in anesthetized rats weremade from individual neurons in the prelimbic part of the mPFC(n 26 neurons) (location shown in Fig. 5d). Action potentialduration (540 20 s peak-to-valley) and firing rate (2.9 0.3spikes/s) were consistent with presumed pyramidal cells ratherthan fast-spikinginterneurons, the latter havinga higher baselinefiring rate (10 Hz) and narrower spike waveform (300 s)
(Constantinidis and Goldman-Rakic, 2002; Laviolette and Grace,2006). Backgroundactivityand responses to innocuous (500g/30mm2) and noxious (2000 g/30 mm 2) stimuli were measured re-peatedly in the same mPFC neurons (n 26) before and forseveral hours after induction of an arthritis pain state (see indi-vidual neurons in Figs. 4b, 5a). Background and evoked activitydecreased in the sample of neurons (n 26) significantly ( p 0.05 0.01, paired ttest, comparing 56 h post-arthritis with pre-arthritis values) (Fig. 5c).
Pharmacologic deactivation of the BLA with NBI27914 (10M) increased the background and evoked activity of prelimbicmPFC neurons in the arthritis pain state (56 h after induction)significantly (n 5; p 0.010.001, paired ttest). An individual
example is shown in Figure 5a, and normalized data for the sam-ple of neurons are summarized in Figure 5e. In contrast, admin-istration of NBI27914 into the CeA had no effect on the pain-related decrease of mPFC activity 56 h after induction ofarthritis (n 5 neurons) (Fig. 5, see individual neuron in b andsummary data in f).
These results provide the first direct evidence that the amyg-dala (BLA) contributes to mPFC deactivation and dysfunction inpain,because blocking pain-related hyperactivity of BLA neuronsrestored normal activity in the prelimbic cortex.
Pain-related increase of glutamate-driven synaptic inhibitionof mPFC neurons
Using whole-cell patch recordings in a brain slice preparationcontaining the mPFC (Orozco-Cabal et al., 2006), we studiedsynaptic mechanisms of BLA-induced PFC inhibition. Specifi-cally, we tested the hypothesis that activation of inhibitory syn-aptic transmission to mPFC pyramidal cells is increased in thearthritis pain state and involves a glutamatergic mechanism. Ourhypothesis was based on anatomical evidence for direct, primar-ily ipsilateral projections from BLA to mPFC, which form gluta-matergic contacts with layer V pyramidalcellsas well as with localcircuit inhibitory neurons in the mPFC (Kita and Kitai, 1990;Gabbott et al., 2006).
EPSCs and IPSCs were evoked in visually identified prelimbiclayer V pyramidal cells (Fig. 6a) by stimulation of presumed af-
ferents from the BLA that traverse the infralimbic cortex as de-scribed previously (Orozco-Cabal et al., 2006). The stimulationelectrode was positioned on the track of anterogradely labeledfibers fromthe BLA (Fig. 6b d). Low stimulus intensities of twicethe threshold were used to avoid current spread and activation ofnearby fibers. Monosynaptic EPSCs were mediated by non-NMDA receptors because they were blocked significantly ( p 0.050.001, compared with predrug control, paired t test) byNBQX (2 M, n 6; 10 M, n 6 neurons) or CNQX (20 M,n 5 neurons) but not by an NMDA receptor antagonist (AP-5,n 4 neurons) (Fig. 6e,f). GABAergic IPSCs were blocked by aGABAA receptor antagonist (bicuculline, 10 M, n 6 neurons)(Fig. 6e). IPSCs recorded at 0 mV holding potential were also
reduced by non-NMDA receptor antagonists (NBQX, 2 M, n
7 neurons; 10 M, n 12; CNQX, 20 M, n 4; p 0.050.01,compared with predrug, paired ttest) (Fig. 6e,g), indicating that
Figure4. ACTHincreases anxiety-like behavior andcorticosteroneblood levelsbut doesnotimpair performance on the gambling task. ACTH (0.2 mg/kg in sterile physiological saline) or
sterile saline (vehicle) was injected intraperitoneally every day for 4 d. Behavioral tests wereperformed1hafterthefinalinjection. a,FinalpreferenceindexofACTH-treatedrats( n 6)inthe rodent gambling task (see Materials and Methods) was positive like that of normal controlrats(n5),reflectingpreferenceforthelow-riskchoice.PreferenceindexofACTH-treatedratsand control rats was significantly different from the negative preference index of arthritic rats(n 5). Final preference index was calculated for the last 30 consecutive trials using thefollowing formula: (low-risk lever choices) (high-risk lever choices)/number of completedtrials. A negative preferenceindex reflects high-risk decision-making (seeMaterialsand Meth-ods). b, In the elevated plus-maze test, open-arm preference (expressed as percentage; seeMaterials and Methods) of ACTH-treated rats (n 6) was significantly decreased compared
withvehicle-treatedcontrolrats (n 6). c, Corticosteroneserum levels (measured withradio-immunoassaykit;Siemens)(Ferreiraetal.,2004)weresignificantlyhigherinACTH-treatedrats(n6)thaninvehicle-treatedcontrolrats(n6).BarhistogramsshowmeanSE.* ,**p0.05, 0.01 (compared with control; ttest); ##,###p 0.01, 0.001 (compared with arthritis;Tukeys multiple comparison test).
5458 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions in Pain
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
9/14
they were polysynaptic. NMDA receptor blockade with AP-5 hadno effect (n 4 neurons) (Fig. 6e,g).
Average latency (from onset of stimulus artifact to onset ofsynaptic current) of monosynaptic EPSCs was significantly ( p0.001, ttest; n 23 neurons) shorter (6.2 0.3 ms) than that ofpolysynaptic IPSCs (8.3 0.4 ms) (Fig. 6h,i). Synaptic jitter (SDof variation in latency) of IPSCs was significantly higher (874
96s) than that of EPSCs (331
29s; p
0.001, ttest; n
23neurons). Average failure rate of IPSCs (27 3%) was signifi-cantly higher than that of EPSCs (8 1.6%) with low stimulusintensities of twice the threshold (n 23 neurons; p 0.001, ttest). EPSCs, but not IPSCs, followed high-frequency (10 Hz)synaptic stimulation.
The pharmacological profile (blockade by NBQX/CNQX andbicuculline) and synaptic characteristics (high jitter, longer la-tency, higher failure rate, inability to follow high-frequency stim-ulation) suggest that the IPSCs were polysynaptic, involving aglutamatergic synapse. In this serial two-step pathway, NBQXblocked an initial unobserved EPSC that was responsible forevoking the bicuculline-sensitive GABAergic IPSC (for discus-sion, see Doyle and Andresen, 2001). The results are consistentwith morphological evidence for glutamatergic projections fromBLA to GABAergic interneurons in the mPFC (Gabbott et al.,2006), suggesting glutamate-driven inhibition of prelimbicmPFC neurons by input from presumed BLA afferents.
Next we determined whether synaptic inhibition of PFC neu-rons increased in the arthritis pain model as a mechanism ofpain-related PFC deactivation and dysfunction. I/O function ofIPSCs (Fig. 7a,c), but not EPSCs (Fig. 7b,d), increased signifi-cantly ( p 0.0001, two-way ANOVA, F(1,242) 55.16) in slicesfrom arthritic rats (6 h after induction; IPSCs, n 7 neurons;EPSCs, n 9) compared with normal controls (IPSCs, n 17neurons; EPSCs, n 21). The data suggest that the strength ofinhibitory rather than excitatory transmission to PFC pyramidal
cells increased in the arthritis pain state.Increased synaptic inhibition of PFC pyramidal cells was
driven by a glutamatergic mechanism involving non-NMDA re-ceptors. Blockade of non-NMDA receptors with NBQX (2 M)decreased evoked IPSCs (Fig. 7a,c) significantly in control slices(n 7 neurons; p 0.0001, two-way ANOVA, F(1,242) 32.98)and in slices from arthritic rats (n 5 neurons; p 0.0001,two-way ANOVA, F(1,110) 129.91). In the presence of NBQX,I/O functions of inhibitory transmission under normal condi-tions and in arthritis were not significantly different ( p 0.05,two-way ANOVA, F(1,110) 0.10), suggesting that the pain-related increase of synaptic inhibition required non-NMDA re-ceptor activation. Accordingly, inhibitory effects of NBQX (2
M) on IPSCs were significantly greater in slices from arthriticrats (29 2.3% of predrug; n 5 neurons) compared withnormal controls (55 7.3% of predrug; n 7;p 0.05, ttest). Ageneral reduction of excitability by the blockade of postsynapticAMPA receptors on pyramidal cells cannot account for the re-sults. Inhibitory effects of NBQX on inhibitory synaptic trans-mission were recorded at the reversal potential for AMPAreceptors (0 mV), and AMPA receptor-mediated excitatory
Figure 5. Deactivation of BLA restores normal activity in PFC neurons. a, Time course ofactivitychangesinanindividualprelimbicmPFCneuronrecordedcontinuouslybeforeandafterinduction of an arthritis painstate (extracellular single-unitrecordingsin an anesthetized rat).Eachsymbol showsbackgroundactivityor responses to innocuous and noxious stimuli appliedto the knee joint (see Fig. 1 ). Administration of a CRF1 receptor antagonist (NBI27914, 10M,concentration in microdialysis fiber; 20 min) into the BLA increased the activity of the mPFCneuron. b, Time course of activity changes in another prelimbic mPFC neuron recorded beforeand afterarthritisinduction. Administrationof NBI27914 (10M)intotheCeAhadnoeffect. c,SignificantdecreaseofbackgroundandevokedactivityinthemPFCneurons56hafterarthri-
tisinduction(n 26 neurons).*p 0.05,**p 0.01 (compared withnormal; pairedttest).d, Recordingsitesin theprelimbic cortex. PL,Prelimbic partof themPFC; IL,infralimbicpart ofthemPFC. e,DeactivationoftheBLAwithNBI27914(10M)increasedthebackgroundactivity
4
of mPFC neurons and their responses to innocuous and noxious stimuli significantly (n 5neurons; p 0.010.001, paired ttest). f, Administration of NBI27914 into the CeA had noeffect on mPFC neurons (n 5). e, f, Bar histograms show mean SE normalized to control
valuesbefore arthritis(setto 100%).For each neuron, twoto three data pointswereaveragedbefore arthritis, 56 h after induction of arthritis, and during drug application (15 min).##,###p 0.01, 0.001 (compared with predrug; paired ttest).
Ji et al. Amygdalo-Cortical Interactions in Pain J. Neurosci., April 14, 2010 30(15):54515464 5459
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
10/14
transmission was not increased in theslices from arthritic animals.
These results are consistent with in-creased non-NMDA receptor function inthe modulationof polysynaptic inhibitorytransmission. The glutamate-driven in-crease of inhibitory, but not excitatory,
transmission to mPFC neurons results ina net shift toward inhibition and is consis-tent with mPFC deactivation shown inour in vivo studies.
DiscussionPain as a multidimensional experience of-fers valuable insight into neurobiologicalmechanisms of sensory, motor, emotional-affective, and cognitive aspects of behavior.Whereas sensorimotor aspects of pain havebeen studied in greatdetail andprogress hasbeen made in the better understanding ofemotional-affective pain processes, mecha-nistic analysis of cognition-related brainfunctions and dysfunctions in pain is lag-ging behind (Neugebauer et al., 2009). Thisstudy tested thehypothesis thatpain-relatedhyperactivity of the BLA, like the CeA, con-tributes to emotional-affective aspects ofpain; however, unlike the CeA, BLA hy-peractivity deactivates the mPFC throughglutamate-driven synaptic inhibition, re-sulting in decision-making deficits. Therationale was based on the accumulatingevidence for cognitive impairment in painin humans (Apkarian et al., 2004b) and
animals (Pais-Vieira et al., 2009), role ofthe PFC (Bechara et al., 1999; Vertes,2006; Pais-Vieira et al., 2007; Stalnaker etal., 2007a; Kouneiher et al., 2009) andamygdala (Bechara et al., 1999, 2003; Stal-naker et al., 2007b; Seymour and Dolan,2008) in emotion-based decision-making,implication of the PFC in pain-relatedcognitive deficits (Apkarian et al., 2004a;Pais-Vieira et al., 2009), and anatomicalconnections (Kita and Kitai, 1990; Mc-Donald, 1991; Bacon et al., 1996; Gabbottet al., 2006) and functional interactions
(Holland and Gallagher, 2004; McGaugh,2004; Laviolette and Grace, 2006; Stal-naker et al., 2007a; Herry et al., 2008;Roozendaal et al., 2009) between amyg-dala and mPFC as a neurobiological basisfor emotional learning and behavior.
The key result of the present study isthat pain-related hyperactivity of BLA neurons contributes notonly to emotional-affective aspects of pain but also to pain-related decision-making deficits through amygdalacortical in-teractions that involve increased glutamate-driven GABAergicsynaptic inhibition of PFC neurons. Specifically, our data showthat BLA neurons, like CeA neurons (Neugebauer et al., 2009),
develop central sensitization and synaptic plasticity in an animalmodel of arthritis pain. Pain-related hyperactivity of BLA neu-rons, like CeA neurons (Ji and Neugebauer, 2007; Fu and Neuge-
bauer, 2008), involves CRF1 receptors. Deactivation of the BLAwith a CRF1 receptor antagonist, like CeA deactivation (Ji et al.,2007; Fu and Neugebauer, 2008), inhibits nocifensive and affec-tive pain responses and pain-related anxiety-like behavior. Thisfirst set of data is consistent with a serial model that involves BLAto CeA projections to execute appropriate emotional responses
(Sah et al., 2003; Maren and Quirk, 2004; Phelps and LeDoux,2005; Seymour and Dolan, 2008; Ehrlich et al., 2009). The resultis novel and important because pain-related functional changes
Figure6. Glutamate-driveninhibitorysynaptictransmissionin themPFC.Whole-cell voltage-clamprecordingsof layerV mPFCpyramidal neurons. a, Individual pyramidal cell visually identified with infrared DIC video microscopy. b, Positions of recordingelectrode in prelimbic cortex (PL) and stimulation electrode on presumed BLA afferents in infralimbic cortex (IL). Level is 3.2 mmanterior to bregma. c, Identification of BLA afferents by anterograde labeling using tracer injections (DiI). Confocal microscopyanalysisofcoronalbrainslicesobtained1012dafterBLAinjectionshowsfluorescentlabelingoffiberbundlesthatdividetoreachlayers II and V of the infralimbic and prelimbic cortices, as described previously (Gabbott et al., 2006; Orozco-Cabal et al., 2006).
Labeling of fibers is only ipsilateral to the injection site, and no cell bodies are stained in layer V (arguing against retrogradelabeling).d, Tracerinjectionsitein theBLA(2.3posterior tobregma).Scalebars(inbd),1mm. eg,EPSCsandIPSCsevokedbystimulatingpresumedBLAafferents(seebf). e,Individualtraces(averageof810)evokedat70mV(downwarddeflections,EPSCs)or at0 mV(upwarddeflections,IPSCs;blocked bybicuculline,10M).Calibration:50pA,20ms.f,EPSCswereinhibitedby
NBQX(2M, n6;10M, n6)andCNQX(20M, n5)butnotbyAP-5(50M, n4).g,IPSCswerealsoinhibitedbyNBQX(2M, n 7;10M, n 12)andCNQX(20M, n 4)butnotbyAP-5(50M, n 4). f,g,Barhistogramsshowmeans SE.* ,** ,***p 0.05,0.01, 0.001(comparedwith predrug; pairedttest).h,IndividualIPSCsandEPSCsevokedwithtwice-thresholdstimulation.Latenciesof IPSCswere longerand more variable.Calibration:50 pA,10 ms. i, Distributionof IPSC andEPSClatenciesmeasuredfromonsetofstimulusartifacttoonsetofsynapticcurrentinoneneuron( n50events).j,MonosynapticEPSCs,butnotpolysynaptic IPSCs, follow high-frequency stimulation (20 Hz; 3 individual traces each).
5460 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions in Pain
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
11/14
in the BLA were not known and previous evidence suggestedpotentially different roles of BLA and CeA in pain modulation(Manning and Mayer, 1995; Tanimoto et al., 2003; Car-rasquillo and Gereau, 2007; Ortiz et al., 2007) and in certainaspects of emotion-related behaviors (Seymour and Dolan,2008; Roozendaal et al., 2009).
Our second set of data shows that hyperactivity in the BLA,but not CeA, is critically involved in pain-related decision-making deficits and deactivation of the medial PFC. Pharmaco-logic deactivation of BLA, but not CeA, restores normal behaviorand cortical activity. Differential effects of CRF1 receptor antag-onist administration into BLA versus CeA (Fig. 3) and lack ofdecision-making deficits in animals with ACTH-induced anxiety
(Fig. 4) argue against more generalized antagonist actions on theHPA axis and suggest that ACTH-induced stress response andanxiety are not sufficient to explain the cognitive impairment
observed in the arthritis pain model. Theconclusion about differential roles of BLAand CeA in amygdalo-cortical pain mech-anisms rests on the selective pharmaco-logical deactivation of BLA versus CeA inelectrophysiological in vivo and behav-ioral studies. The differential effects of
CRF1 receptor antagonist administrationinto theBLA versusCeA on mPFC activityand on decision-making behavior argueagainst the spread of drug from the injec-tion site to the other nucleus. As anotherimportant control for drug diffusion, ad-ministration of the antagonist into theCeA did not affect activity of BLA neu-rons. Conversely, drug administrationinto the BLA (this study) or CeA (previ-ous studies) had similar inhibitory effectson neuronal activity in the respective nu-cleus and on nocifensive and affective be-haviors. In theslice preparation, theCRF1antagonist acted postsynaptically directlyon BLA neurons in this study and on CeAneurons in the previous study. Thus, bothnuclei have functional CRF1 receptorsthat can be targeted to deactivate the neu-rons, but the consequences are nucleusspecific.
The underlying mechanism of pain-related BLA-driven cortical deactivationand cognitive deficits is increased synapticinhibition of mPFC pyramidal cells. Al-though details of the cortical circuitry re-main to be determined, pharmacological
and electrophysiological data of our studyare consistent with a polysynaptic pathway,in which glutamate activates GABAergictransmission onto pyramidal cells throughnon-NMDA receptors. Disynaptic feed-forward inhibition is found in variousbrain areas and involves activation of inhib-itory interneurons and their target cells bythe same excitatory input (Doyle and An-dresen, 2001; Silberberg and Markram,2007; Ferrante et al., 2009). In the rat so-matosensory cortex, GABAergic inhibi-tory transmission to layer V pyramidal
cells is driven via glutamatergic afferents arriving at non-NMDAreceptors on interneurons (Ling and Benardo, 1995). In contrast,axo-axonic ionotropic glutamate receptor-mediated excitationof the nerve terminals of inhibitory interneurons and subsequentsynaptic inhibition of nearby pyramidal cells that was reported inthe mouse visual cortex (Ren et al., 2007) has been questionedrecently (Hull et al., 2009).
Our model of glutamate-driven synaptic inhibition is sup-ported by anatomical data showing that pyramidal cells in theBLA, but not CeA, form monosynaptic glutamatergic connec-tions not only with layer V pyramidal cells but also nearbyGABAergic interneurons in the mPFC (Kita and Kitai, 1990; Ba-con et al., 1996; Gabbott et al., 2006). Additional evidence for the
glutamatergic drive originating in the BLA is based on our in vivostudies showing that deactivation of BLA projection neurons in-creased mPFC activity. The time course of BLA hyperactivity and
Figure 7. Increased synaptic inhibitionof PFC neurons in arthritis painmodel. Whole-cellvoltage-clamp recordingsof visuallyidentified prelimbic layer V pyramidal cells as in Figure 6. a, Evoked IPSCs (recorded at 0 mV) increased in arthritis and weredecreasedbyNBQX(2and10M).b,EvokedEPSCs(recordedat70mV)wereinhibitedbyNBQX(2and10 M)incontrolslicesand in slices from arthritic rats (6 h after induction). Calibration: 100 pA, 50 ms. Individual traces are averages of 810 IPSCs. c,Inputoutput functions of IPSCs increased in slices from arthritic rats (56 h after induction; n 7 neurons) compared withnormal controls (n 17 neurons) significantly (two-way ANOVA, F(1,242) 55.16, p 0.0001). NBQX (2 M) significantlydecreased IPSCs in control slices (n 7 neurons; two-way ANOVA, F(1,242) 32.98, p 0.0001) and in slices from arthritic rats
(n 5neurons;two-wayANOVA, F(1,110) 129.91,p 0.0001). d,InputoutputfunctionsofevokedEPSCsinslicesfromarthritic rats (n 9 neurons) and from normal controls (n 21 neurons) were not significantly different (two-way ANOVA,F(1,308) 1.84, p 0.05). NBQX (2M) had significant inhibitory effects under normal conditions (n 6 neurons; two-way ANOVA,F(1,275)70.69,p0.0001)andinarthritis(n6neurons;two-wayANOVA,F(1,143)46.25,p0.0001).*p0.05(comparedwithnormal;Bonferronisposthoctest).
Ji et al. Amygdalo-Cortical Interactions in Pain J. Neurosci., April 14, 2010 30(15):54515464 5461
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
12/14
of mPFC deactivation in the arthritis model was comparable. Inthe slice preparation, the stimulation site for evoking synapticresponseswas selected based on fluorescent labeling of fibersafteranterograde tracer (DiI) injections into the BLA. The course ofthe fibers through the infralimbic cortex has been shown in pre-vious studies of BLAPFC projections (Gabbott et al., 2006;Orozco-Cabal et al., 2006). Although activation of nearby fibers
attributable to current spread cannot be ruled out, the use of lowstimulus intensities (Fig. 6) and evaluation of the full range ofinputoutput relationships (Fig. 7) makes a confounding effectof multiple pathway activation unlikely.
Although the proposed model of glutamatergic BLA projec-tion to GABAergic mPFC interneurons can explain BLA-drivencortical deactivation, it remains to be determined why excitatorytransmission to mPFC pyramidal cells did not change in the ar-thritis pain model. One possible explanation is that separate linesof input account for excitatory transmission to pyramidal cellsand to inhibitory interneurons. Another possibility is thatglutamate-driven GABAergic transmission controls the directexcitatory input to pyramidal cells, and pain-related increase ofthe GABAergic tone prevents increased glutamatergic drive ontopyramidal cells. In support of this hypothesis, preliminary datasuggest that blockade of GABA receptors in the mPFC increasesmonosynaptic excitatory transmission to pyramidal cells (H. Sunand V. Neugebauer, unpublished observation). GABAergic con-trol of excitatory inputs to pyramidal cells may involve presynap-tic GABA receptors on the axon terminal (Miller, 1998) and/orpostsynaptic GABA receptors on the soma that would occlude orshunt an (increased) effect of excitatory drive. Greater sensitivityof cortical interneurons than pyramidal cells to excitatory inputsattributable to cell-type-specific differences in the relative kinet-ics of excitatory and inhibitory synaptic currents (Cruikshank etal., 2007) would further explain why inhibitory interneurons cancontrol excitatory transmission onto pyramidal cells. Expression
of faster gating AMPA receptors with higher Ca 2 permeabilityin interneurons than pyramidal cells (Markram et al., 2004) con-tributes to the faster synaptic kinetics of inhibitory interneurons(Cruikshank et al., 2007).
The novelty of these results is the functional changes ofamygdalo-cortical interactions in pain and the contribution ofthese upstream projections to decision-making deficits. Previousstudies showed that a majority of orbitofrontal neurons respondto noxious cutaneous (Snow et al., 1992) and/or visceral (Yangand Follett, 1998) stimuli. The present study not only identifiedneurons in the mPFC that respond to noxious stimuli but alsoshowedfor thefirsttime that activity of these neurons is inhibitedin a model of persistent pain. Reduced mPFC activity was also
observed in conditioned fear, but the neural mechanism remainsto be determined (Garcia et al., 1999). Inhibitory, but not excita-tory, synaptic transmissionto layer V pyramidalcellsincreased inour arthritis pain model. In a model of neuropathic pain, theNMDA, but not non-NMDA, receptor component of excitatorysynaptic transmission increased in layer II/III pyramidal cells,inhibitory transmission was not measured, and underlyingmechanisms and behavioral consequences remain to be deter-mined (Metz et al., 2009). These results may suggest differentialchanges in functionally distinct subsets of mPFC neurons in dif-ferent pain models.
Pain-related mPFC inhibition is the result of BLA hyperactiv-ity. In this relationship, the amygdala modulates cortical activity
through upstream projections, whereas the traditional view hasbeen top-down cortical (PFC) regulation of the amygdala (Urryet al., 2006; Delgado et al., 2008; Herry et al., 2008). However,
facilitatory upstream interactions between amygdala and cortexare important for emotional learning and memory (Roozendaalet al., 2009), including BLA-dependent plasticity of mPFC neu-rons in olfactory fear conditioning (Laviolette and Grace, 2006).The amygdala also influences sensory cortical plasticity and facil-itates attention and perception to emotionally significant stimuli(Phelps and LeDoux, 2005). Conversely, an inverse correlation
between amygdala and PFC has been found in the regulation ofnegative affect (Urry et al., 2006), conditioned fear (Garcia et al.,1999), and fear extinction (Milad et al., 2007) but also in cue-evoked reward-seeking behavior (Ishikawa et al., 2008).
In our study, the inverse relationship between BLA and mPFCproduced cortical deactivation and decision-making deficits inpain. The correlation of decreased PFC activity with impairedcognitive function is supported by neuroimaging (Breiter et al.,2001; Daw et al., 2006; Hampton et al., 2006; Taylor et al., 2006)and electrophysiological (Oya et al., 2005) data in humans.Cocaine-induced decision-making deficits (impaired cognitiveflexibility on reversal learning and gambling tasks) involve a lossof outcome-expectant encoding in the orbitofrontal cortex andsubsequently inflexible encoding of cue significance in the BLA(Stalnakeret al., 2007b). Impaired cognitiveflexibility induced byorbitofrontal cortical lesions is improved by BLA ablation (Stal-naker et al., 2007a). Cocaine-induced decision-making deficits(cognitive inflexibility) are reminiscent of those observed in thepresent study (failure to switch strategies), and both involve ab-normal amygdalar activity. However, BLA miscoding was theconsequence of cocaine-inducedorbitofrontal dysfunction (Stal-naker et al., 2007b), whereas our data show that abnormal BLAactivity drives mPFC dysfunction in pain. The inverse BLAmPFC interaction in pain is consistent with BLA-mediated de-pression of mPFC activityin conditioned fear (Garcia et al., 1999)and decreased amygdala activation but increased ventromedialPFC activation during fear extinction (Milad et al., 2007).
This study is thefirst demonstration of a neuralmechanism bywhich the amygdala impairs cortical and cognitive function inpain. Our results suggest a parallel model of BLAmPFC interac-tion for cognitive aspects of pain and BLACeA circuits involvedin emotional-affective pain responses. BLA encodes emotions intheir context and signals stimulus-specific information (Amaralet al., 2003; Balleine and Killcross, 2006; Herry et al., 2008). Con-nections with CeA execute appropriate emotional behavior (Sahet al., 2003; Phelps and LeDoux, 2005), whereas connections withPFC produce goal-directed actions (Seymour and Dolan, 2008)and are important for reappraisal of emotional stimuli, extinc-tion learning, and cognitive emotion-regulation strategies(Phelps and LeDoux, 2005; Delgado et al., 2008; Herry et al.,
2008), which may be impaired in pain and other disorders.
ReferencesAmaral DG, Bauman MD, Schumann CM (2003) The amygdala and au-
tism: implications from non-human primate studies. Genes Brain Behav2:295302.
Apkarian AV, Sosa Y, Sonty S, Levy RM, Harden RN, Parrish TB, GitelmanDR (2004a) Chronic back pain is associated with decreased prefrontaland thalamic gray matter density. J Neurosci 24:1041010415.
Apkarian AV, Sosa Y, Krauss BR, Thomas PS, Fredrickson BE, Levy RE,HardenRN, Chialvo DR (2004b) Chronic pain patients areimpaired onan emotional decision-making task. Pain 108:129136.
Bacon SJ, Headlam AJ, Gabbott PL, Smith AD (1996) Amygdala input tomedial prefrontal cortex (mPFC) in the rat: a light and electron micro-scope study. Brain Res 720:211219.
Balleine BW, Killcross S (2006) Parallel incentive processing: an integratedview of amygdala function. Trends Neurosci 29:272279.
Bechara A, Damasio H, DamasioAR, Lee GP (1999) Different contributions
5462 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions in Pain
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
13/14
of the human amygdala and ventromedial prefrontal cortex to decision-making. J Neurosci 19:54735481.
Bechara A, Damasio H, Damasio AR (2003) Role of the amygdala indecision-making. Ann N Y Acad Sci 985:356369.
Bird GC, Lash LL, Han JS, Zou X, Willis WD, Neugebauer V (2005) Proteinkinase A-dependent enhanced NMDA receptor function in pain-relatedsynaptic plasticity in rat amygdala neurones. J Physiol 564:907921.
Breiter HC, Aharon I, Kahneman D, Dale A, Shizgal P (2001) Functional
imaging of neural responses to expectancy and experience of monetarygains and losses. Neuron 30:619639.Carrasquillo Y, Gereau RW 4th (2007) Activationof the extracellular signal-
regulated kinase in the amygdala modulates pain perception. J Neurosci27:15431551.
Carvalho TP, Buonomano DV (2009) Differential effects of excitatory andinhibitory plasticity on synaptically driven neuronal input-output func-
tions. Neuron 61:774785.Constantinidis C, Goldman-Rakic PS (2002) Correlated discharges among
putative pyramidal neurons and interneurons in the primate prefrontalcortex. J Neurophysiol 88:34873497.
Cruikshank SJ, Lewis TJ, Connors BW (2007) Synaptic basis for intense
thalamocortical activation of feedforward inhibitory cells in neocortex.Nat Neurosci 10:462468.
Daw ND, ODoherty JP, Dayan P, Seymour B, Dolan RJ (2006) Corticalsubstrates for exploratory decisions in humans. Nature 441:876 879.
Delgado MR, Nearing KI, Ledoux JE, Phelps EA (2008) Neural circuitry
underlying the regulation of conditioned fear and its relation to extinc-tion. Neuron 59:829838.
Doyle MW, Andresen MC (2001) Reliability of monosynaptic sensorytransmission in brain stem neurons in vitro. J Neurophysiol85:22132223.
Ehrlich I, Humeau Y, Grenier F, Ciocchi S, Herry C, Luthi A (2009) Amyg-dala inhibitory circuits and the control of fear memory. Neuron62:757771.
Ferrante M, Migliore M, Ascoli GA (2009) Feed-forward inhibition as abuffer of the neuronal input-output relation. Proc Natl Acad Sci U S A
106:1800418009.Ferreira JG, Cruz C, Vinson GP, Pignatelli D (2004) ACTH modulates ERK
phosphorylation in the adrenal gland in a time-dependent manner. En-docr Res 30:661666.
Fu Y, Neugebauer V (2008) Differential mechanisms of CRF1 and CRF2receptor functions in the amygdala in pain-related synaptic facilitationand behavior. J Neurosci 28:38613876.
Gabbott PL, Warner TA, Busby SJ (2006) Amygdala input monosynapti-cally innervates parvalbumin immunoreactive localcircuit neurons in ratmedial prefrontal cortex. Neuroscience 139:10391048.
Garcia R, Vouimba RM, Baudry M, Thompson RF (1999) The amygdalamodulates prefrontal cortex activity relative to conditioned fear. Nature402:294296.
Hampton AN, Bossaerts P, ODoherty JP (2006) The role of the ventrome-dial prefrontal cortex in abstract state-based inference during decision
making in humans. J Neurosci 26:83608367.HerryC, Ciocchi S, SennV, Demmou L, Muller C, Luthi A (2008) Switching
on and off fear by distinct neuronal circuits. Nature 454:600606.Holland PC, Gallagher M (2004) Amygdala-frontal interactions and reward
expectancy. Curr Opin Neurobiol 14:148155.Hull C, Adesnik H, Scanziani M (2009) Neocortical disynaptic inhibition
requires somatodendritic integration in interneurons. J Neurosci29:89918995.
IkedaR, TakahashiY, InoueK, KatoF (2007) NMDAreceptor-independentsynaptic plasticity in thecentral amygdala in therat modelof neuropathic
pain. Pain 127:161172.Ishikawa A, Ambroggi F, Nicola SM, Fields HL (2008) Contributions of the
amygdala and medial prefrontalcortex to incentivecue responding. Neu-roscience 155:573584.
JasminL, RabkinSD,Granato A,Boudah A, OharaPT (2003) Analgesiaand
hyperalgesia from GABA-mediated modulation of the cerebral cortex.Nature 424:316320.
Ji G, Neugebauer V (2007) Differential effects of CRF1 and CRF2 receptorantagonists on pain-related sensitization of neurons in the central nucleus
of the amygdala. J Neurophysiol 97:38933904.Ji G, NeugebauerV (2009) Hemispheric lateralization of pain processing by
amygdala neurons. J Neurophysiol 102:22532264.
Ji G, Fu Y, Ruppert KA, Neugebauer V (2007) Pain-related anxiety-like be-
havior requires CRF1 receptors in the amygdala. Mol Pain 3:1317.Kita H,KitaiST (1990) Amygdaloidprojectionsto thefrontalcortex andthe
striatum in the rat. J Comp Neurol 298:4049.
Kouneiher F, Charron S, Koechlin E (2009) Motivation and cognitive con-trol in the human prefrontal cortex. Nat Neurosci 12:939945.
Laviolette SR, Grace AA (2006) Cannabinoids potentiate emotional learn-ing plasticity in neurons of the medial prefrontal cortex through basolat-
eral amygdala inputs. J Neurosci 26:64586468.Ling DS, Benardo LS (1995) Recruitment of GABAA inhibition in rat neo-cortex is limited and not NMDA dependent. J Neurophysiol
74:23292335.Manning BH, Mayer DJ (1995) The central nucleus of the amygdala con-
tributes to the production of morphineantinociception in the rattail-flicktest. J Neurosci 15:81998213.
Maren S, Quirk GJ (2004) Neuronal signalling of fear memory. Nat Rev
Neurosci 5:844 852.Markram H, Toledo-Rodriguez M, Wang Y, Gupta A, Silberberg G, Wu C
(2004) Interneurons of the neocortical inhibitory system. Nat Rev Neu-rosci 5:793807.
McDonald AJ (1991) Organization of amygdaloid projections to the pre-
frontal cortex and associated striatum in the rat. Neuroscience 44:114.McGaraughty S, Heinricher MM (2002) Microinjection of morphine into
various amygdaloid nuclei differentially affects nociceptive responsive-ness and RVM neuronal activity. Pain 96:153162.
McGaugh JL (2004) The amygdala modulates the consolidation of memo-
ries of emotionally arousing experiences. Annu Rev Neurosci 27:128.Metz AE, Yau HJ, Centeno MV, Apkarian AV, Martina M (2009) Morpho-
logical and functional reorganization of rat medial prefrontal cortex inneuropathic pain. Proc Natl Acad Sci U S A 106:24232428.
Milad MR, Wright CI, Orr SP, Pitman RK, Quirk GJ, Rauch SL (2007) Re-
call of fear extinction in humans activates the ventromedial prefrontalcortex and hippocampus in concert. Biol Psychiatry 62:446 454.
Miller RJ (1998) Presynaptic receptors. Annu Rev Pharmacol Toxicol38:201227.
Murakami N, Takahashi K (1983) Enhancement of corticosterone release
by repeated injections of ACTH in the dexamethasone pre-treated rat.Acta Endocrinol (Copenh) 102:583588.
Myers B, Greenwood-Van Meerveld B (2007) Corticosteroid receptor-
mediated mechanisms in the amygdala regulate anxiety and colonic sen-sitivity. Am J Physiol Gastrointest Liver Physiol 292:G1622G1629.
Neugebauer V, Li W (2003) Differential sensitization of amygdala neuronsto afferent inputsin a model of arthriticpain. J Neurophysiol89:716727.
Neugebauer V, Keele NB, Shinnick-Gallagher P (1997) Epileptogenesis invivo enhances the sensitivity of inhibitory presynaptic metabotropic glu-tamate receptors in basolateral amygdala neurons in vitro. J Neurosci
17:983995.Neugebauer V, Chen PS,Willis WD (1999) Role of metabotropic glutamate
receptor subtype mGluR1 in brief nociception and central sensitization ofprimate STT cells. J Neurophysiol 82:272282.
Neugebauer V, Zinebi F, Russell R, Gallagher JP, Shinnick-Gallagher P
(2000) Cocaine and kindling alter the sensitivity of group II and IIImetabotropic glutamate receptors in the central amygdala. J Neuro-physiol 84:759770.
Neugebauer V, Li W, Bird GC, Bhave G, Gereau RW 4th (2003) Synapticplasticity in the amygdala in a model of arthritic pain: differential roles of
metabotropic glutamate receptors 1 and 5. J Neurosci 23:5263.Neugebauer V, Li W, Bird GC, Han JS (2004) The amygdala and persistent
pain. Neuroscientist 10:221234.Neugebauer V, Han JS, Adwanikar H, Fu Y, Ji G (2007) Techniques for
assessing knee joint pain in arthritis. Mol Pain 3:820.Neugebauer V, Galhardo V, Maione S, Mackey SC (2009) Forebrain pain
mechanisms. Brain Res Rev 60:226242.Orozco-Cabal L, PollandtS, Liu J, Vergara L, Shinnick-GallagherP, Gallagher
JP (2006) A novel rat medial prefrontal cortical slice preparation to in-
vestigate synaptic transmission from amygdala to layer V prelimbic pyra-midal neurons. J Neurosci Methods 151:148158.
Ortiz JP, Heinricher MM, Selden NR (2007) Noradrenergic agonist admin-istration into the central nucleus of the amygdala increases the tail-flick
latency in lightly anesthetized rats. Neuroscience 148:737743.Oya H, Adolphs R, Kawasaki H, Bechara A, Damasio A, Howard MA 3rd
(2005) Electrophysiological correlates of reward prediction error re-
Ji et al. Amygdalo-Cortical Interactions in Pain J. Neurosci., April 14, 2010 30(15):54515464 5463
-
8/2/2019 2010 - Ji Et Al - J Neuroscience
14/14
corded in the human prefrontal cortex. Proc Natl Acad Sci U S A102:83518356.
Pais-Vieira M, Lima D, Galhardo V (2007) Orbitofrontal cortex lesions dis-rupt risk assessment in a novel serial decision-making task for rats. Neu-roscience 145:225231.
Pais-Vieira M, Mendes-Pinto MM, Lima D, Galhardo V (2009) Cognitiveimpairment of prefrontal-dependent decision-making in rats after theonset of chronic pain. Neuroscience 161:671679.
Paulus MP (2007) Decision-making dysfunctions in psychiatryaltered ho-meostatic processing? Science 318:602606.
Phelps EA, LeDoux JE (2005) Contributions of the amygdala to emotionprocessing: fromanimal models to human behavior.Neuron 48:175187.
Rainnie DG, Bergeron R, Sajdyk TJ, Patil M, Gehlert DR, Shekhar A (2004)Corticotrophin releasing factor-induced synaptic plasticity in the amyg-dala translates stress into emotional disorders. J Neurosci 24:34713479.
Ren M, Yoshimura Y, Takada N, Horibe S, Komatsu Y (2007) Specializedinhibitory synaptic actions between nearby neocortical pyramidal neu-rons. Science 316:758761.
Roozendaal B, McEwen BS, Chattarji S (2009) Stress, memory and theamygdala. Nat Rev Neurosci 10:423433.
Sah P, Faber ES, Lopez De Armentia M, Power J (2003) The amygdaloidcomplex: anatomy and physiology. Physiol Rev 83:803834.
Seymour B, Dolan R (2008) Emotion, decision making, and the amygdala.Neuron 58:662671.
Silberberg G, Markram H (2007) Disynaptic inhibition between neocorticalpyramidal cells mediated by Martinotti cells. Neuron 53:735746.
Snow PJ, Lumb BM,Cervero F (1992) Therepresentationof prolongedandintense, noxious somatic and visceral stimuli in the ventrolateral orbitalcortex of the cat. Pain 48:8999.
Stalnaker TA, Franz TM, Singh T, Schoenbaum G (2007a) Basolateralamygdala lesions abolish orbitofrontal-dependent reversal impairments.Neuron 54:5158.
Stalnaker TA, Roesch MR, Franz TM, Calu DJ, Singh T, Schoenbaum G(2007b) Cocaine-induceddecision-making deficits are mediated by mis-coding in basolateral amygdala. Nat Neurosci 10:949951.
Tanimoto S, Nakagawa T, Yamauchi Y, Minami M, Satoh M (2003) Differ-ential contributions of the basolateral and central nuclei of the amygdalain the negative affective component of chemical somatic and visceralpains in rats. Eur J Neurosci 18:23432350.
Taylor SF, Martis B, Fitzgerald KD, Welsh RC, Abelson JL, Liberzon I, HimleJA, Gehring WJ (2006) Medial frontal cortex activity and loss-relatedresponses to errors. J Neurosci 26:40634070.
Urry HL, van Reekum CM, Johnstone T, Kalin NH, Thurow ME, SchaeferHS, Jackson CA, Frye CJ, Greischar LL, Alexander AL, Davidson RJ(2006) Amygdala and ventromedial prefrontal cortex are inversely cou-pledduring regulationof negative affect and predict the diurnal pattern ofcortisol secretion among older adults. J Neurosci 26:4415 4425.
Vertes RP (2006) Interactions among the medial prefrontal cortex, hip-pocampus and midline thalamus in emotional and cognitive processingin the rat. Neuroscience 142:120.
Walf AA, Frye CA (2007) The use of the elevated plus maze as an assay ofanxiety-related behavior in rodents. Nat Protoc 2:322328.
Washburn MS, Moises HC (1992) Electrophysiological and morphological
properties of rat basolateral amygdaloid neurons in vitro. J Neurosci12:40664079.
Yang S, Follett KA (1998) The effectof morphine on responsesof ventrolat-eralorbital cortex (VLO) neurons to colorectaldistension in the rat.BrainRes 808:101105.
5464 J. Neurosci., April 14, 2010 30(15):54515464 Ji et al. Amygdalo-Cortical Interactions










![COELI DÈSUPER CopioneUnificato.pdf · 4 Nitida stella [1:00] - (Anunziata) Anonimo afff32 F =150 3 jj jj jj eii jj jj jj jj i ji j i ji j i ji j eiizz bfff32 j j j i j j j j i j](https://static.fdocuments.net/doc/165x107/5fde88e826cc8964f53d1e56/coeli-d-copioneunificatopdf-4-nitida-stella-100-anunziata-anonimo-afff32.jpg)
![JI – 5 · JI – 5 Sprinkler Assembly JI – 5 Tripod Stand Sprinkler 1TFGTKPI 5RGEK ECVKQPU ¢ £ ¤ ¥ c g j m _ j ¦ ] d b w _ d z {§ ¨ l ©] g j b ª « ¬ « ® ¯ ° ±](https://static.fdocuments.net/doc/165x107/604e5e8b665e866ff03c696b/ji-a-5-ji-a-5-sprinkler-assembly-ji-a-5-tripod-stand-sprinkler-1tfgtkpi-5rgek.jpg)