1+1 ..,, ,, CENTRAL HEALTH · 2016-11-07 · JUL-30-2010 09:36 TRAVIS COUNTY ATTORNEY p. 001/001...
Transcript of 1+1 ..,, ,, CENTRAL HEALTH · 2016-11-07 · JUL-30-2010 09:36 TRAVIS COUNTY ATTORNEY p. 001/001...

JUL-30-2010 09:36 TRAVIS COUNTY ATTORNEY p. 001/001
1+1 CENTRAL HEALTH ..,, ,, CENTRAL HEAL TH
BOARD OF MANAGERS
AGENDA
Wednesday, August 4, 2010 5:30 p.m.
Central Health Administrative Offices 1111 E. Cesar Chavez Street
Austin, Texas 78702 Board Room
CITIZENS' COMMUNICATION
CONSENT AGENDA
Notice to Public
Came lo hand and posted on a Bullotin fl-Oa111 in !he Courthouse Austin, Tra11is County, Texas on !his !he i?O""" day of
"},, l;;r 20 I <5 9ana DaBcauvoir
~~~~~eou-n7"{'j_r:--'•~<.2'~·~===-"-fy,_Texa~'~Oeputy a-i, .. ··' All matters listed under the CONSENT AGENDA will be considered by the Board of Managers to be routine and will be enacted by one motion_ There will be no separate discussion of these Items unless members of the Board or persons in the audience request speclftc items be moved from the CONSENT AGENDA to the REGULAR AGENDA for discussion plior to the time the Board of Managers votes on the motion to adopt the CONSENT AGENDA.
C1. Approve minutes for the following meeting of the Central Health Board of Managers:
a. March 25, 2010
REGULAR AGENDA*
1. Receive and discuss a presentation on the HMO Feasibility Study and discuss next steps in the process.
2. Receive and discuss a long-term visioning process for Central Health, including a presentation on Federally Qualified Health Centers.
3. Confirm the next regular Board meeting date, time, and location.
•The Board of Managers may take items in an order that differs from the posted order.
The Board of Managers may consider any matter posted on the agenda in a closed meeting if there are issues that require consideration in a closed meeting and the Board announces that the item will be considered during a closed meeting.
TOTAL P.001

Board of Managers meeting
August 4, 2010
AGENDA ITEMS C1
C1. Approve minutes for the following meeting of the Central Health Board of Managers.

MINUTES OF MEETING – MARCH 25, 2010
TRAVIS COUNTY HEALTHCARE DISTRICT d/b/a CENTRAL HEALTH
BOARD OF MANAGERS MEETING
On Thursday, March 25, 2010, a regular meeting of the Central Health Board of Managers convened in open session at 5:33 p.m. in the Ned Granger Building Commissioners Courtroom, 314 West 11th Street, Austin, Texas 78701. A quorum of the Board was present. Chairperson Coopwood and Secretary Barker were present. Clerk for the meeting was Margo Davis. ___________________________________________________________________________________
CITIZENS’ COMMUNICATION
Clerk’s Notes: None.
CONSENT AGENDA
C1. Approve minutes for the following meetings of the Central Health Board of Managers: (a) December 17, 2009; and (b) January 9, 2010.
Clerk’s Notes: None. C2. Receive the March 2010 Investment Report and ratify Central health investments for
March 2010. Clerk’s Notes: None. C3. Approve the previously proposed amendments to the Bylaws of the Board of Managers of
Central Health. Clerk’s Notes: None. Manager Coleman-Beattie MOVED that the Board approve Consent Agenda Items C1 – C3.
Secretary Barker SECONDED the motion. The motion was adopted on the following vote: Chairperson Tom Coopwood For Vice-Chairperson Rosie Mendoza For Treasurer Frank Rodriguez Absent Secretary Bobbie Barker For Manager Anthony Haley For Manager Clarke Heidrick Absent Manager Donald Patrick Absent Manager Brenda Coleman-Beattie For Manager Katrina Daniel Absent
REGULAR AGENDA

MINUTES – March 25, 2010
3. Receive and discuss information regarding the Children’s Optimal Health program. Clerk’s Notes: This item was taken out of order. Manager Katrina Daniel and Manager Clarke Heidrick joined the meeting during this agenda item.
Beth Peck, Senior Healthcare Planner for Central Health, introduced Kit Abney Spelce, Acting
Director for Children’s Optimal Health, and Dr. Stephen Pont, Co-Chair of the Technical Advisory Committee for Children’s Optimal Health, noting that a two-part presentation would be made for this agenda item.
Ms. Spelce provided an overview of the current state of the organization. Children’s Optimal
Health’s mission was presented as follows: “Through a commitment of shared data, collaboration, and ongoing communication, Children’s Optimal Health is a collective leadership initiative to ensure that every child in Central Texas becomes a healthy, productive adult engaged in his or her community.” Central Health’s role as a funding charter member of Children’s Optimal Health was noted. The goal of Children’s Optimal Health and the use of Geographic Information System (GIS) mapping is to inform policy, improve operations, promote research, and mobilize the community to better the lives of children and youth by bringing together public and proprietary data.
To illustrate the value of data sharing, Dr. Pont reviewed maps that track childhood obesity for 2007-08 and 2008-09 that were created using Austin Independent School District (AISD) data on body mass index and cardiovascular fitness. The maps sort childhood obesity data according to various geographic and economic criteria and correlations to socioeconomically challenged areas were demonstrated. Dr. Pont noted that a map can also show positive and negative influences on the food environment (e.g. grocery stores and fast food restaurants), and access to possible venues for physical activity for children (e.g. parks). Further data correlation could include crime factors affecting safe access to physical activity venues and the presence or absence of ready access to fresh food. Dr. Pont discussed ways in which the maps have motivated change in schools and communities, and how action at a Board level could also have an impact on problems such as obesity.
Questions were raised by Board members regarding the source of the AISD data, along with the status of physical education generally in the public schools, the timing of intervention for childhood obesity given that risk factors develop earlier in life, and Central Health’s access to maps from various projects. In response, Dr. Pont noted that the AISD data was gathered in connection with TEA-mandated fitness testing for children in grades 3 through 12, and the scope of student participation in the fitness assessment varied according to school involvement. Data from the maps could be used to further evaluate contributing factors in geographic areas and identify effective early childhood intervention strategies for siblings and relatives of identified obese students, such as promotion of breastfeeding and reduction of passive activity. The methodology for measuring cardiovascular fitness was explained, and the potential for error in assessing a particular student’s cardiovascular fitness on a pass/fail scale was highlighted. Dr. Pont indicated that maps from the childhood obesity project and a trauma project will be shared with Central Health.
Dr. Pont also reported that Children’s Optimal Health is currently working on a pre-natal project in which birth and outcome data from hospital systems is being evaluated. The various Children’s Optimal Health projects go forward in a community summit forum where agencies and Boards participate to spur community action. Additionally, Children’s Optimal
Page 2

MINUTES – March 25, 2010
Health has received national attention by having an article on childhood obesity published in the journal Health Affairs. It was noted that HBO discussed a documentary it is producing about obesity with that organization; that documentary will broadcast in Fall 2012.
5. Receive and discuss an update on federal health reform. Clerk’s Notes: This item was taken out of order in order to allow presentation of this update
and consideration of an agenda item in Executive Session to occur prior to Manager Heidrick’s departure.
Stacy Wilson, Director of Government Affairs; Albert Hawkins, public policy consultant under contract with Central Health and CommUnityCare; and Marsha Jones, partner with the firm HillCo Partners, discussed health reform. Ms. Wilson gave a ten year overview of the healthcare reform bill and discussed implications of the legislation. Mr. Hawkins discussed the Patient Protection and Affordable Care Act and significant changes that will occur within six months including changes regarding pre-existing conditions, lifetime caps on private healthcare policies, the ages to which unmarried children may stay on their parents’ group insurance, changes to Medicaid and Medicare, and increased funding for community health centers. Ms. Jones offered a framework for legislature actions and the political response. Board members raised questions regarding the anticipated impact of the legislation on assistance programs, which serve a segment of the population that is targeted for federal healthcare coverage. The presenters noted continuing concern about the impact of reform on providers who accept Medicaid, despite inclusion of an increase in payment rates for primary care providers. The increased rate, as proposed, would be federally funded for a two-year period with maintenance of the increased rate falling to the states thereafter. Questions were also raised by Board members regarding provisions in the proposed reform legislation for insurance premium increases, high risk pools, and drug cost subsidies; along with the impact of the proposed legislation on healthcare for undocumented immigrants and coverage for mental health services.
8. Discuss and take appropriate action on information related to the status of the North
Central Health Center.
Clerk’s Notes: This item was taken out of order. Chairperson Coopwood announced that the Board of Managers would convene in Executive Session to discuss Agenda Item 8 under Section 551.071 of the Texas Government Code, Consultation with Attorney. The Board of Managers convened in closed session at 6:49 p.m. Manager Heidrick left the meeting during Executive Session. The Board of Managers re-convened in open session at 7:29 p.m.
3. Receive and discuss information regarding the Children’s Optimal Health program.
Page 3

MINUTES – March 25, 2010
Clerk’s Notes: The Board of Managers resumed consideration of this item following
conclusion of the Executive Session. Beth Peck, Senior Healthcare Planner, reviewed multiple data maps and explained
information the maps convey. Board members discussed with Ms. Peck how capacity of the Central Health provider network could be correlated with demand for services the various locations, and the joint planning process with CommUnityCare to yield a plan for facilities, partnerships, and service strategies as guided by the data.
1. Receive and discuss a report of the February 2010 financial statements for Central
Health.
Clerk’s Notes: John Stephens, Chief Financial Officer, discussed financial statements for Central Health for the month of February 2010 and reported that the financial condition of Central Health is strong. In response to a question from Chairperson Coopwood, Mr. Stephens stated that reimbursement of DSH / UPL funds is not anticipated during the current or upcoming fiscal year.
2. Receive and discuss the fiscal year 2009 Annual Report. Clerk’s Notes: Christie Garbe, Chief Communications and Planning Officer, and Mike
McKinnon, Communications Coordinator, presented an overview of the 2009 Annual Report. A pre-production copy of the report was presented, with final copy available by the next Board meeting. Ms. Garbe and Mr. McKinnon worked with Hahn Texas on development of the printout, graphic design, and new logo. The layout of the report was reviewed, and Ms. Garbe gave highlights of the content. Board comment was received on the choice of graphic representations rather than images of people in the 2009 report, and Ms. Garbe noted that a piece that includes such images is currently in development.
4. Discuss and take appropriate action on a Letter of Support for the City of Austin’s
application for the “Google Fiber for the Home” program. Clerk’s Notes: Manager Katrina Daniel discussed Google’s effort to place an ultra high speed
broadband network in a small number of communities in the country, the benefit of the network for the healthcare community and for Google, and a possible letter of support from Central Health.
Manager Daniel MOVED that the Board authorize the Board Chair to sign a Letter of Support on
behalf of Central Health to be included with the City of Austin’s application for the “Google Fiber for the Home” program as presented by staff. Manager Coleman-Beattie SECONDED the motion. The motion was adopted on the following vote:
Chairperson Tom Coopwood For
Vice-Chairperson Rosie Mendoza For Treasurer Frank Rodriguez Absent Secretary Bobbie Barker For
Page 4

MINUTES – March 25, 2010
Manager Anthony Haley For Manager Clarke Heidrick For Manager Donald Patrick Absent Manager Brenda Coleman-Beattie For Manager Katrina Daniel For 6. Receive and discuss the CEO’s report on the following District activities: (a) procurement
activity; (b) communications/outreach statistics for February 2010; (c) the MAP Program, including March enrollment and activities; and (d) an update on the Community Planning Initiative.
Clerk’s Notes: Patricia Young Brown, President and Chief Executive Officer, gave a report on particular District activities. The report included public presentations by staff on various topics such as healthcare reform, and increasing Medical Assistance Program enrollment. Board members discussed with staff the possibility of having, in addition a MAP enrollment chart, a chart reflecting approved Sliding Fee Scale applications. Final resolution of this matter is subject to changes being made to eligibility and enrollment processes.
7. Confirm the next regular Board meeting date, time, and location. Clerk’s Notes: Chairperson Coopwood announced that the next regular Board meeting is
scheduled to be held on Thursday, April 8, 2010, at 5:30 p.m., in the Cesar Chavez Building, Board Room, 1111 East Cesar Chavez Street, Austin, Texas, 78702.
There being no further discussion on agenda items, Manager Coleman-Beattie MOVED that the meeting adjourn. Manager Haley SECONDED the motion. The motion was adopted on the following vote:
Chairperson Tom Coopwood For Vice-Chairperson Rosie Mendoza For Treasurer Frank Rodriguez Absent Secretary Bobbie Barker For Manager Anthony Haley For Manager Clarke Heidrick Absent Manager Donald Patrick Absent Manager Brenda Coleman-Beattie For Manager Katrina Daniel For The meeting adjourned at 8:21 p.m.
Page 5

MINUTES – March 25, 2010
Page 6
___________________________________ Tom Coopwood, Chairperson Central Health Board of Managers ATTESTED TO BY: ___________________________________ Bobbie Barker, Secretary Central Health Board of Managers

Board of Managers meeting
August 4, 2010
AGENDA ITEMS 1
1. Receive and discuss a presentation on the HMO Feasibility Study and discuss next steps in the process.

August 4, 2010
Presented By Dennis Edmonds, PresidentDennis Edmonds & Associates, LLC
HMO Feasibility Study Update
Presentation to Board of Managers
2
Presentation Outline
• Stakeholder Discussion Highlights
• HMO Flow of Funds Overview
• Feasibility Study Dashboard

3
Reasons For a Non-Profit Community Based HMO
• Rapidly growing Medicaid population• Alternative to 2 for-profit health plans• Expand patient access• Promote preventive care and a medical home • Coordinate care and social services • Link public and private resources• Reinvest profits in the community• Central Health uniquely positioned to sponsor
HMO
4
Key Themes
• Central Health is respected in community• There is a need for a community-based HMO• Expanding patient access is critical• Coordinated approach and leveraging of
public/private resources would be beneficial• Opportunities to collaborate abound • Frequent changes in eligibility status can create
problems/bad debt• For the most part, Medicaid patients take more
time to serve than commercial

5
Key Themes - Continued
• Medicaid reimbursement is inadequate• There is a shortage of primary/specialty care
providers – and some are not willing to see Medicaid patients
• Everyone is preparing for healthcare reform• It may be possible to leverage FQHC funding• HMO must be fiscally sound and well managed• Strong community outreach will be required• Link medical care with mental health and social
services
6
HMO Flow of Funds Overview
• HMO Perspective• Health Exchange Perspective• HHSC Perspective• Central Health MAP Perspective

7
Central Health HMO Perspective
Central Health HMO
Urgent Care Centers
Central Health Health ExchangeHHSC
Specialists
PCPs
CommUnitycare
Ancillary Providers
Reinsurer
Hospitals
Administrator
Pharmacy (PBM)
Mental Health Central Health
Medical Expenses Admin. Expenses
ASO Fees $Medicaid Premium $ Other Plan Premium $
Claims Reserves
HMO Admin.
$ $
$ $
8
Health Exchange Perspective
Health Plans
Health ExchangeFederal Subsidies
Individuals Small Groups
Administrator
Premiums $
$ $
Subsidized Premium $
e.g. Central Health HMO

9
HHSC Perspective
Health Plans
HHSC
Federal Funds
Administrator
$
$
Premium $
State Funds
Rebate $
10
Central Health MAP Perspective
Central Health
Breckenridge Lease Pmts & Other
Central Health HMO
$
$ ASO Fee
Property Tax
Providers
Claim $
Administrative Services

11
HMO Feasibility Study Dashboard Phase 1
Activity Status Results Next StepsStakeholder Meetings
40% •17 of 20 Initial Target Interviews
–Providers–Elected Officials–Community Organizations–Educational Institutions
•Preliminary Feedback Favorable•Expanded Target List to 44
•Additional Interviews•Finalize Results
Network Strategy 60% •Researched Delivery System•Competitor Network Assessment•Network Overview Spreadsheet•Basic Network Strategy
•Confirm Hospitals•Finalize Network Strategy
Strategic Objectives 10% •Initial Discussions •Alternative Strategies•Recommendations
12
HMO Feasibility Study Dashboard Phase 2
Activity Status Results Next StepsHealth Care Reform Assessment
50% •Research•Display Key Provisions
•Additional Research•Final Summary
Preliminary Financial Plan
10% •Flow of Funds•Roles & Responsibilities Matrix
•Financial Assumptions•Proforma P&L
Other Health Care Districts
10% •Initial Staff Discussions•Identified 5 Districts•Targeted Key Contacts
•Conduct Meetings•Lessens Learned•Recommendations

13
HMO Feasibility Study Dashboard Phase 3
Activity Status Results Next StepsCompetitor Assessment
0% •NA •Update Preliminary Assessment
HHSC Contract Interest
0% •NA •Confirm HHSC Interest
Marketing Strategy 0% •NA •Update Preliminary Assessment
Enrollment Forecast 0% •NA •Marketing Assumptions•3-Year Monthly Forecast
14
HMO Feasibility Study Dashboard Phase 4
Activity Status Results Next StepsLegal / Regulatory Plan
0% •NA •Detailed Plan & Assumptions
Governance, Organization & Staffing Plan
0% •NA •Detailed Plan & Assumptions
Marketing Plan 0% •NA •Detailed Plan & Assumptions
Network Plan 0% •NA •Detailed Plan & Assumptions
Operations and IT Plan
0% •NA •Detailed Plan & Assumptions
Medical Management Plan
0% •NA •Detailed Plan & Assumptions
Detailed Financial Plan
0% •NA •Detailed Breakeven Analysis

15
Open Discussion
• Key Issues To Explore• Questions and Information Needed• Next Steps
Learn more about us at:
www.traviscountyhd.org

Board of Managers meeting
August 4, 2010
AGENDA ITEMS 2
2. Receive and discuss a long-term visioning process for Central Health, including a presentation on Federally Qualified Health Centers.

Memo
To: Central Health Board of Managers From: Beth Peck, Senior Healthcare Planner CC: Patricia A. Young Brown, Christie Garbe Date: July 29, 2010 Re: Preparation for Board Meeting This is to provide you with an overview of the long-range visioning discussion planned for the August 4, 2010 board meeting. The discussion will focus on the planning question – “How does Central Health best utilize CommUnityCare and its associated federally qualified health center (FQHC) status as a resource for the community?” To frame the discussion, staff will be presenting a very high-level overview of what a federally qualified health center is as well as the relationship between Central Health and CommUnityCare. Following this presentation, Jackie Leifer, Partner with Feldesman Tucker Leifer Fidell LLP, will be returning to discuss a number of opportunities available to FQHCs through the health reform legislation, including additional funding, medical schools, accountable care organizations, and teaching centers. I have attached the informational sheet that Ms. Leifer provided at our May 27, 2010, meeting along with some background materials that Ms. Leifer sent to provide more in-depth information on some of these issues. Finally, staff will conclude the discussion of this item by facilitating a dialogue with the Board around the following questions –
• What is the Board’s opinion on extending FQHC status to other community primary care providers through affiliation as a strategy for more fully supporting community health care services?
• Which of the opportunities mentioned is the Board most interested in pursuing? • What additional information does the Board feel is needed to help determine how best to use
the FQHC asset that we have?
I hope that you find the attached information useful for next week’s discussion. As always, thank you for your commitment to Central Health and to this planning process.

Travis County HealthCare District Opportunities to Access Additional Federal Resources in Support of the Community’s
Health Care Safety Net
May 27, 2010
Longstanding Safety Net Grant Programs • Section 330
o FY2010 Budget $2.19 billion o President’s FY2011 Budget proposes a $290 million increase for the Section 330
program • Ryan White • Other (e.g., Title X)
American Recovery and Reinvestment Act (ARRA)
• Signed into law on February 17, 2009 • $2 billion in grants to FQHCs to support the provision of comprehensive primary and
preventive health care to an increasing number of patients; create or retain thousands of jobs; and enable FQHCs to address pressing capital improvement needs, such as construction, repair, renovation, and equipment purchases (including health information technology – HIT – systems)
• $1.5 billion for Community Health Center Capital Programs
Texas Home Health Grant • $25 million in grants for eight pilot projects, each of which will receive $1 – 2 million • Target population: minimum 5,000 Medicaid kids with special needs • Encourages collaborations • See “Health Home Grant Discussion” document for additional information
Health Reform
• Signed into law on March 23, 2010 • New funding for FQHCs
o Allocates $11 billion to FQHCs over the next 5 years, which includes $1.5 billion for capital projects (FY 2011 - $1.0 billion; FY 2012 - $1.2 billion; FY 2013 - $1.5 billion; FY 2014 - $2.2 billion; and FY 2015 - $3.6 billion; there is no annual breakdown for the capital projects funds)
o It is anticipated that HRSA will issue a request for New Access Point applications this summer, with expansion opportunities to follow shortly thereafter
• National Health Service Corps
o Allocates $1.5 billion over five years for the National Health Service Corps, which will place an estimated 15,000 primary care providers in communities with health professional shortages (FY 2011 - $290 million; FY 2012 - $295 million; FY 2013 - $300 million; FY 2014 - $305 million; and FY 2015 - $310 million)
1

• Title VII Teaching Health Centers Development Grants
o Grants will be awarded to cover the costs of establishing or expanding primary care residency training programs (i.e., family medicine, internal medicine, pediatrics, internal medicine-pediatrics, obstetrics and gynecology, psychiatry, general dentistry, pediatric dentistry and/or geriatrics), including costs associated with curriculum development; recruitment, training and retention of residents and faculty; accreditation by the Accreditation Council for Graduate Medical Education, the American Dental Association, or the American Osteopathic Association; and faculty salaries during the development phase
$230 million over 5 years
• Other New Programs and Demonstration Projects
o Center for Medicare and Medicaid Innovation (CMI) (must begin carrying out its duties no later than January 1, 2011)
Purpose of CMI is to test innovative payment and service delivery models (e.g., patient-centered medical home models, community-based health teams to support small-practice medical homes by assisting the PCP in chronic care management, risk-based comprehensive payment to providers)
Preference is for models that improve the coordination, quality, and efficiency of healthcare services
$10 billion is appropriated during FY 2011-2019
o Community Health Teams and Patient-Centered Medical Homes Grants Authorizes grants or contracts to states to support the establishment of
health teams that support primary care practices, including OB/GYN practices
Model of care that includes: • Personal physicians • Whole person orientation • Coordinated and integrated care • Safe and high-quality care through evidence-informed
medicine, appropriate use of HIT “Health teams” must:
• Include interdisciplinary, inter-professional team of health care providers
• Support patient-centered medical homes • Collaborate with local primary care providers to coordinate
disease prevention, chronic disease management, transitioning between health care settings, and case management
• Demonstrate the "capacity to implement and maintain health information technology . . . to facilitate coordination among the
2

members of the health team and affiliated primary care practices”
• Provide other support necessary for primary care providers to improve quality of care
o Accountable Care Organizations (ACOs)
Medicare Shared Saving Program (begins no later than January 1, 2012)
• Eligible ACOs may be composed of group practices, networks of individual practices, partnerships or joint venture arrangements between hospital and practitioners, hospitals employing practitioners, and other groups of providers/suppliers as determined by HHS
• Providers must meet certain criteria, including quality measurements, to form an ACO
• ACO must: o Be accountable for the quality and cost of healthcare
services for the Medicare fee-for-service beneficiaries assigned to it
o Include primary care professionals o Have a formal legal structure o Have a shared governance structure and engage in joint
decision-making o Have a leadership and management structure that
includes clinical and administrative systems o Demonstrate that it meets patient-centeredness criteria
• Eligible ACOs must have at least 5,000 Medicare fee-for-service beneficiaries and must commit to participate for three years
• Participating ACO will be eligible to receive payments from savings if it achieves quality and cost containment standards
o Medicaid Global Payment System Demonstration (effective fiscal years 2010 through 2012)
Authorizes demonstration projects in the Medicaid program Global safety net hospital systems or networks would move from a
FFS structure to a global capitated payment model Limited to 5 states
o Community-Based Collaborative Care Networks
Grants will be awarded to support community-based collaborative care networks; the network is described as a consortium of health care providers with a joint governance structure (including providers within a single entity) that provides comprehensive coordinated and integrated health care services for low-income populations
3

4
Must include a hospital and all federally qualified health centers located in the community
Must have a joint governance structure
o Co-locating Primary and Specialty Care in Community-Based Mental Health Settings
Authorizes grants and cooperative agreements to community mental health centers to establish demonstration projects for the provision of coordinated and integrated services to special populations through the co-location of primary and specialty care services in community-based mental and behavioral health settings
$50,000,000 for FY2010 and such sums as may be necessary for FY2011 through FY2014
Core Health Center Requirements and Unique FQHC Benefits
Range of Collaboration Opportunities
• Referral arrangements • Co-location arrangements • Integration of services of multiple providers (e.g., behavioral health) • Transfer existing sites to health center license • Establish new sites • Teaching agreements • “ER diversion” programs • Retail clinics • Community benefit grants

ISSUE BRIEF Accountable Care Organizations
March 2009
Reforming Provider Payment Moving Toward Accountability for Quality and Value
Introduction The ongoing debate over health care reform in the United States has expanded from targeted concerns about the millions of Americans without health insurance to broader consideration of gaps in quality, rising health care costs, and the structure of a system that is failing to address either problem. Dramatic variations in healthcare spending that bear little correlation to quality indicate that our current system neither rewards nor encourages higher-value care. For example, we spend three times more per Medicare beneficiary in certain geographic regions than in others – and yet the quality and outcomes of care are no better. In addition, many preventive services are underused, and adherence to proven-effective therapies for many chronic diseases is low. Medical errors and other safety problems remain too common, accounting for many thousands of deaths and billions of dollars in health care costs. All of these gaps in care are reinforced by Medicare’s current payment systems, which tend to promote high-volume and high-intensity care regardless of quality, and do not support innovative approaches to coordinating care or preventing avoidable complications or services. The Need for a New Payment Model and Principles for Payment Reform Increasing awareness of these problems has resulted in a growing array of public- and private-sector initiatives to promote efforts by providers to improve care and to foster greater accountability for both quality and cost. While there is ongoing debate over the specific form that such approaches should take and how to implement them around the country, these efforts are marked by growing consensus on several guiding principles for reform. First, there is increasing agreement on the need for local accountability for quality and cost across the continuum of care. The consistent provision of high-quality care – particularly for those with serious and chronic conditions – will require the coordination and engagement of multiple health care professionals across different institutional settings and specialties. The health care system must not only facilitate, but also encourage such coordination. Second, a successful approach to achieving greater accountability must be viable across the diverse practice types and organizational settings that characterize the U.S. health care system and should be sufficiently flexible to allow for variation in the strategies that local health systems use to improve care. Third, successful reform will require a shift in the payment system from one that rewards volume and intensity to one that promotes value (improved care at lower cost), encourages collaboration and shared responsibility among providers, and ensures that payers – both public and private – offer a consistent set of incentives to providers.

Finally, with increased accountability on the part of providers must come greater transparency for consumers. Measures of overall quality, cost, and other aspects of performance relevant to consumers will facilitate informed choices of both providers and services and increase consumers’ confidence in the care they are receiving as their providers face different incentives. Many of the payment reforms that have been proposed or are already in use – for example, bundled payments, disease management, and pay for performance – represent meaningful steps toward greater accountability. The next step is accountability for care that leads to better outcomes and lower costs at the person level, with support for the infrastructure required to provide high-quality, coordinated care. The Accountable Care Organization Model The Accountable Care Organization (ACO) model establishes a spending benchmark based on expected spending. If an ACO can improve quality while slowing spending growth, it receives shared savings from the payers. This model is well-aligned with many existing reforms, such as the medical-home model and bundled payments, and also offers additional support (and accountability) to the provider organization to enable them to deliver more efficient, coordinated care. This approach has been implemented in programs like Medicare’s Physician Group Practice (PGP) Demonstration, which has shown significant improvements in quality and savings for large group practices. Because the groups receive a share of the savings beyond a threshold level, steps like care coordination services, wellness programs, and other approaches that achieve better outcomes with less overall resource use result in greater reimbursement to the providers. These steps thus “pay off” and are sustainable in a way that they are not under current reimbursement systems. In addition, the shared savings approach provides an incentive for ACOs to avoid expansions of health care capacity that are an important driver of both regional differences in spending and variations in spending growth, and that do not improve health. The ACO approach also builds on current reform efforts that focus on one key group of providers, as in the medical-home model, or on a discrete episode of care, as in bundled payments. On their own, these initiatives may help strengthen primary care and improve care coordination, but they do not address the problem of supply-driven cost growth highlighted by the Dartmouth group. If adopted within a framework of overall accountability for cost and quality as is envisioned in the ACO model, both the medical home and bundled payment reforms would have added incentives to support not only better quality, but also lower overall spending growth (see Table 1). By shifting the emphasis from volume and intensity of services to incentives for efficiency and quality, ACOs provide new support for higher-value care without radically disrupting existing payments and practices. The ACO model builds on current provider referral patterns and offers shared savings payments, or bonuses, to providers on the basis of quality and cost. A wide variety of provider collaborations can become ACOs assuming that they are willing to be held accountable for overall patient care and operate within a particular payment and performance measurement framework. Examples include existing integrated delivery systems, physician networks such as independent practice associations, physician-hospital organizations, hospitals that have their own primary-care physician networks, and multispecialty group practices. Alternatively, primary-care groups or other organizations that provide basic care could contract with specialized groups that provide high-quality referral services with fewer costly complications.
2

Table 1 Comparison of Payment Reform Models
Accountable
Care Organization
(Shared Savings)
Primary Care Medical Home
Bundled Payments Partial Capitation Full Capitation
General strengths and weaknesses
Makes providers accountable for total per-capita costs and does not require patient “lock-in.” Reinforced by other reforms that promote coordinated, lower-cost care
Supports new efforts by primary-care physicians to coordinate care, but does not provide accountability for total per-capita costs
Promotes efficiency and care coordination within an episode, but does not provide accountability for total per-capita costs
Provides “upfront” payments that can be used to improve infrastructure and process, but provides accountability only for services/providers that fall under partial capitation, and may be viewed as too risky by many providers/patients
Provides “upfront” payments for infrastructure and process improvement and makes providers accountable for per-capita costs, but requires patient “lock-in” and may be viewed as too risky by many providers/ patients
Strengthens primary care
directly or indirectly
Yes – Provides incentive to focus on disease management within primary care. Can be strengthened by medical home or partial capitation to primary-care physicians
Yes – Changes care delivery model for primary-care physicians allowing for better care coordination and disease management
Yes/No – Only for bundled payments that result in greater support for primary-care physicians
Yes – Assuming that primary care services are included in the partial capitation model allows for infrastructure, process improvement, and a new model for care delivery
Yes – Gives providers “upfront” payments and changes the care delivery model for primary-care physicians
Fosters coordination
among all participating
providers
Yes – Significant incentive to coordinate among participating providers
No – Specialists, hospitals and other providers are not incentivized to participate in care coordination
Yes (for those within the bundle) – Depending on how the payment is structured, can improve care coordination
Yes– Strong incentive to coordinate and take other steps to reduce overall costs
Yes– Strong incentive to coordinate and take other steps to reduce overall costs
Removes payment
incentives to increase volume
Yes – Adds an incentive based on value, not volume
No – There is no incentive in the medical home to decrease volume
No, outside the bundle – There are strong incentives to increase the number of bundles and to shift costs outside
Yes/No – Strong efficiency incentive for services that fall within the partial capitation model
Yes – Very strong efficiency incentive
Fosters accountability for total per-capita costs
Yes – In the form of shared savings based on total per-capita costs
No – Incentives are not aligned across provider, no global accountability
No, outside the bundle, no accountability for total per-capita cost
Yes/No – Strong efficiency incentive for services that fall within partial capitation
Yes – Very strong accountability for per-capita cost
Requires providers to bear risk for excess costs
No – While there might be risk-sharing in some models, the model does not have to include provider risk
No – No risk for providers continuing to increase volume and intensity
Yes, within episode – Providers are given a fixed payment per episode and bear the risk of costs within the episode being higher than the payment
Yes – Only for services inside the partial capitation model
Yes – Providers are responsible for costs that are greater than the payment
Requires “lock-in” of patients
to specific providers
No – Patients can be assigned based on previous care patterns, but includes incentives to provide services within participating providers
Yes – To give providers a PMPM payment, patients must be assigned
No – Bundled payments are for a specific duration or procedure and do not require patient “lock-in” outside of the episode
Yes (for some) – Depending on the model, patients might need to be assigned to a primary-care physician
Yes – To calculate appropriate payments, patients must be assigned
3

Regardless of specific organizational form, the ACO model has three key features:
1. Local Accountability. ACO entities will be comprised of local delivery collaborations that can effectively manage the full continuum of patients’ care, from preventive services to hospital-based and nursing-home care. Their patient populations are comprised of those who receive most of their primary care from the primary-care physicians associated with the ACO (see Figure 1). (As noted above, ACOs may include a range of specialists, hospitals, and other providers, or may contract or collaborate with them in other ways.)
Multi‐Specialty Group Practice
ACO Model 3
Hospital
Specialty Group
PCP Group
ACO Model 1
Community Hospital
Specialty Group
PCP Group
ACO Model 2
Home Health Services
Mental Health Facility
Tertiary Care Facility
Specialty Physicians
Specialty Hospital
Figure 1
ACOs Can Be Configured in Different Ways(Some care will likely be delivered outside of the ACO)
2. Shared Savings. ACO-specific expenditure benchmarks will be based on historical trends
and adjusted for patient mix. Contingent on meeting designated quality thresholds, ACOs with expenditures below their particular benchmark will be eligible for shared savings payments, which can be distributed among the providers within the ACO. These shared savings allow for investments – in health IT or medical homes, for example – that can in turn improve care and slow cost growth (see Figure 2).
Projected Spending
Actual Spending
Shared Savings
Spending Benchmark
Launch of “Illustrative” ACO
Figure 2
Shared Savings Derived from Spending Below Benchmarks That Are Based on Historical Spending Patterns
3. Performance Measurement. Valid measurement of the quality of care provided through
ACOs will be essential to both ensuring that cost savings are not the result of limiting necessary care and promoting higher-quality care. Such measurement should include meaningful outcome and patient-experience data.
4

Laying the Foundation for Successful Implementation
While the ACO framework holds promise for improving quality, cost, and overall efficiency, it does create some important implementation issues. It is worth highlighting some factors that can improve the likelihood of success. Engagement of a broad range of key local stakeholders, such as payers, purchasers, providers, and patients alike, can provide momentum for ACOs. A demonstrated history of successful innovation and reform with respect to health IT adoption and clinical innovations, for example, may also be a good foundation for further ACO reforms. Having a structural foundation in place at the outset will also facilitate the transition to an ACO. Key factors include patient populations that are sufficient in size to permit reliable assessment of expenditures and quality performance relative to benchmarks, in order to calculate shared savings. Additional key elements include some degree of integration – either formal or virtual (i.e., for the purposes of the ACO) – within the delivery system and the capacity for collecting and reporting on the performance of participating providers. Finally, having an agreement and process in place for distributing shared savings will be critical in terms of presenting an attractive proposition to providers – that is, a real opportunity to generate additional payments in return for improved care – and rewards genuine improvements in efficiency. Key Design Components While consideration of the more technical aspects of implementation are beyond the scope of this overview, a brief description of several key design questions highlights the decisions that will need to be made at the ACO level through negotiations with participating payers:
• Organization of the ACO. The form and management of the ACO need to be well-defined. ACO “leaders” who will drive improvements in care and efficiency must be identified from the start.
• Scope of the ACO. The specific providers involved in ACOs are likely to include primary-care
physicians and may also include selected specialists as well as hospitals and other providers. Such decisions about the scope of providers to be included will clearly shape many of the technical aspects of the ACO, referral patterns, and other behavioral changes induced by the ACO itself.
• Spending and quality benchmarks. Spending benchmarks must be projected with sufficient
accuracy based on historical data (or other comparison groups) and savings thresholds to provide confidence that overall savings will be achieved. Sufficient measures of quality to provide evidence of improvement are also essential.
• Distribution of shared savings. Elements of the distribution of savings that will be subject to
negotiation include the percentage split between providers and payers, for example 80/20 or 50/50, and the specific agreement governing how the savings will be distributed among the ACO providers.
5

Looking Ahead: The Promise of ACOs The ACO model is receiving significant attention among policymakers and leaders in the health care community, not only because of the unsustainable path on which the country now finds itself, but also because it directly focuses on what must be a key goal of the health care system: higher value. The model offers a promising approach for achieving this goal without requiring radical change in either the payment system or current referral patterns. Rather, fee-for-service remains in place, and most physicians already practice within natural referral networks around one or a few hospitals. By promoting more strategic and effective integration and care coordination, the ACO model holds substantial promise as a reform that offers a potential win-win for providers, payers, and patients alike. For a more technical discussion of the ACO model, including budget implications, see:
• CBO, Budget Options, Volume I: Health Care (December 2008), pp. 72-74 (Option 37, “Bonus Eligible Organizations”).
• Fisher, Elliott, Mark McClellan, John Bertko, Steven Lieberman, Julie Lee, Julie Lewis, and
Jonathan Skinner. “Fostering Accountable Health Care: Moving Forward in Medicare.” Health Affairs Web Exclusive, January 27, 2009: w219-w231.
6

Can Accountable Care Organizations Improve the Value of Health Care by Solving
the Cost and Quality Quandaries?
Timely Analysis of Immediate Health Policy IssuesOctober 2009
Kelly Devers and Robert Berenson
Introduction In the current health reform discussions, accountable care organizations (ACOs) have been proposed as a novel way to slow rising health care costs and to improve quality in the traditional Medicare program and perhaps other public and private insurance programs. However, for many, it is not clear what ACOs are and whether and how they differ from other past reform approaches intended to achieve the same goals. The ACO concept is confusing partly because it is a concept with a history, one that is rapidly evolving and for which the terminology seems to keep changing. In fact, as the Issue Brief will show, different reform ideas have now been joined under the rubric of ACO.
The primary purposes of this Issue Brief are to provide insight into what ACOs seem to represent and whether they potentially offer a new and improved way to reform U.S. provider payment and delivery systems, with an emphasis on their application in Medicare. First, we clarify what ACOs generally are, including the current concept’s genesis and important dimensions on which ACOs might vary. Second, we discuss what is new about the current ACO concept compared to previous reform concepts, such as “accountable health plans” or Health Maintenance Organizations (HMOs) and provider-sponsored organizations (PSOs) that were established for Medicare in the Balanced Budget Amendment (BBA) of 1997.
Third, we identify key ACO program features and issues policymakers are grappling with and about which there are different and even divergent viewpoints. These include: (1) the ACO definition and qualifying criteria, such as what kinds of providers must be included and whether an ACO is different from a patient-centered medical home (PCMH); (2) whether an ACO program should be voluntary or mandatory for providers; (3) similarly, whether beneficiaries should be assigned to ACOs or should elect to participate in one; (4) alternative ACO payment methods and their respective strengths and weaknesses; and, (5) quality measurement and monitoring. Decisions about these program features and issues will strongly influence providers and patients’ reactions to the ACO concept.
Finally, we discuss several major implementation challenges, specifically, participation of and possible untoward impact on other payers and the new roles, responsibilities, and capabilities for providers and government. We also summarize some of the pointed skepticism that some have leveled at the ACO concept and consider whether this is another example of a concept advanced more by wishful thinking than by empirically based policy analysis.
We conclude that ACOs are no game changer in the short run because they require resolution of some challenging and complex issues as well as significant provider and policymaker learning, but nonetheless, they are important to try.
If done well, an ACO program could build on lessons learned from and since the managed care era of the 1990s, get critical provider payments and delivery system changes underway, and perhaps in the long run move us beyond reliance on what many consider a dysfunctional fee-for-service (FFS) payment system.
What is an ACO?Fundamentally, the ACO concept couples provider payment and delivery system reforms in an attempt to solve the “chicken and egg” problem.1 Many believe that to bend the cost curve while improving quality, we must reform the provider payment system first, because it pays for volume rather than value. Others hold that it is impossible to change the payment system to achieve the desired objectives unless delivery system reform first produces organizations capable of handling an altered payment system. They point to the need for health care professionals, now usually working in separate institutional settings, to work collaboratively and to demonstrate their capacity for handling new payment approaches. To avoid the quandary of where to start first—provider payment or delivery system reform—the ACO concept attempts to combine them.
More specifically, ACOs can generally be defined as a local entity and a related set of providers, including at least primary care physicians, specialists, and hospitals, that can be held accountable for the cost and quality of care delivered to a defined subset of traditional

Timely Analysis of Immediate Health Policy Issues 2
Medicare program beneficiaries or other defined populations, such as commercial health plan subscribers.2 The primary ways the entity would be held accountable for its performance are through changes in traditional Medicare provider payment featuring financial rewards for good performance based on comprehensive quality and spending measurement and monitoring. Public reporting of cost and quality information to affect public perception of an ACO’s worth is another way of holding the ACO accountable for its performance.
Proponents generally view three ACO characteristics as essential. These characteristics include: (1) the ability to provide, and manage with patients, the continuum of care across different institutional settings, including at least ambulatory and inpatient hospital care and possibly post acute care; (2) the capability of prospectively planning budgets and resource needs; and, (3) sufficient size to support comprehensive, valid, and reliable performance measurement.3 Table 1 summarizes the diverse entities that could serve as an ACO, solely or in combination, including their capacity on the first two criteria.
Diverse entities could serve as an ACO, alone or in combination with each other, the collective serving as a local provider umbrella organization, system, or network (see figure 1). Shortell and Casalino4 identify five different types of
existing organizations that could either exclusively serve as an ACO in a local geographic area, or more likely lead or be part of an ACO led by another provider organization in the area. These existing provider organizations include (1) various types of physician groups or physician-centered organizations, namely multispecialty group practices (MSGs) and interdependent physician organizations (IPOs)—what most people refer to as an independent practice association (IPA); (2) hospital-centered organizations, namely hospital medical staff organizations (MSOs) and physician-hospital organizations (PHOs); and (3) Health Plan-Provider Organization or Networks (HPPNs). The latter is similar to a particular type of HMO, specifically one that contracts with one or more IPAs or with independent physician practices. However, rather than discussing HPPNs which can already participate in Medicare as a Medicare Advantage (PA) plan, we discuss organized or integrated delivery systems (ODSs or IDSs) more narrowly.5
Fisher and his team6 also acknowledge that this range of existing provider organizations could surely serve as ACOs, but they also introduce the idea that a new type of organization,7 fostered by analysis of Medicare claims data and comprised of local hospitals and the physicians who work in and around them, could also form ACOs. It is this “virtual” organization concept
that spurred the recent ACO interest based on the view that these less formal organizations could develop relatively quickly and throughout the heterogeneous forms of U.S. health care delivery.
Together, the Medicare Payment Advisory Commission (MedPAC), the organization that advises Congress on payment and related policies for Medicare, and Fisher provided the impetus for the current concept and interest in ACOs, building on two developments—an early, positive evaluation of the Medicare Physician Group Practice (PGP) Demonstration that relied on an FFS-based payment model8 and analysis by Fisher that patients cared for by particular physician groups flowed to or clustered at particular hospitals.9 The latter analysis suggested to some that a virtual, extended hospital medical staff could be held accountable for total spending and the quality of care for patients who obtain their care from this set of physicians, similar to the way that the MSGs in the PGP demonstration were being held accountable in determining their eligibility for financial bonuses for performance.10
Others have followed with their own versions of ACOs, sometimes using different terminology and offering somewhat different prescriptions for their design features. For example, in the House of Representatives
Table 1. Potential ACO Models and Their Characteristics
Provider TypeAbility to Provide or Manage
Care Across Continuum
Ability to Plan Budgets and Resource Needs (Accept and manage non-FFS payment)
Provider Inclusiveness Level of Performance
Accountability
IPA Low/Medium Medium High Medium
Multispecialty Group Medium/High Medium Low/Medium Medium/High
Hospital Medical Staff Organization
Medium Low/Medium Medium Low/Medium
Physician-Hospital Organization (PHO)
Medium/High Medium/High Low/Medium Medium/High
Organized or Integrated Delivery Systems
Medium/High Medium/High Medium Medium/ High
Virtual approach-Extended Hospital Medical Staff
Medium Low/Medium High Low
*Based on the literature about these types of organizations.

Timely Analysis of Immediate Health Policy Issues 3
Tri-Committee on Health Reform draft legislation that set up ACO demonstrations,11 the definition of an ACO is quite broad, and the Secretary of the Department of Health and Human Services would delineate a more specific definition and qualifying criteria when proceeding to solicit demonstration participants. Qualifying criteria would have to delineate, for example, what legal structure would be acceptable for permitting the ACO entity and its constituent providers to receive and distribute payments and the minimum number and types of physicians needed in an ACO. The Senate Finance Committee Chairman’s Mark also uses a quite broad ACO definition, but articulates more specific qualifying criteria, leaving less discretion for the Secretary in designing the demonstrations.12
What is new about the ACO concept and proposals?While the notion of accountability is not new, the locus of accountability has changed. “Accountability” became
a key word and critical part of the managed competition approach adopted in President Clinton’s Health Security Act, in which health maintenance organizations (HMOs) were dubbed “accountable health plans.”13 Developers of the ACO concept also emphasize accountability, but focus directly on health care providers and the delivery system instead of insurers and HMOs. The focus on local providers and delivery systems stems from a desire to address a number of continuing, frequent problems, including absence of financial incentives to reduce cost and improve quality and resultant problems, such as uncoordinated care and unwarranted geographic variation in practice patterns and health spending. The new approach, then, emphasizes accountability at the level of actual care delivery.
Second, the ACO concept envisions direct contracting with provider organizations without the reliance on a health plan intermediary and thus is distinct and separate from the contracting that occurs in the Medicare
Advantage program, which presumably would continue in parallel. Actually, in the BBA of 1997, PSOs were created to facilitate Medicare engaging in financial risk contracting directly with provider organizations. However, only a few PSOs have developed and participated in the program in the decade that this option has been available. As discussed later, current ACO proposals do not envision the degree of provider risk assumption that subjected PSOs to state insurance regulation or the BBA-enabled alternative. Nevertheless, to the extent that some ACO proposals would involve providers taking financial risk, thereby raising concerns about solvency, and would employ even mild limitations or incentives to channel beneficiaries to ACO providers, the program might again have to address complex insurance regulation issues that affected the PSO effort.14
Third, the ACO concept and current proposals potentially allow great flexibility in both the types of organizations that would qualify to serve as an ACO and the available provider payment methods. Some think this degree of flexibility differs from previous reform approaches that emphasized particular types of insurance or provider organization—HMOs or IDSs—or one approach to provider payment—full capitation, as in the PSO program. The degree of flexibility in the ACO concept and in some proposals is recognition of the substantial variation in local health care markets, as well as in provider organizations and their willingness and ability to accept nonstandard, FFS payments. The increased flexibility presumably would provide opportunities for virtually all physicians and hospitals to participate and would “let the market work,” in the sense that local market conditions and dynamics would ultimately determine which ACO organizational model and supportive payment approach prevailed in any particular area.
Figure 1. Possible ACO Configurations, Comprised of Different Provider Organizations in Local and Regional Geographic Areas
Tertiary or Quaternary Care Facility and Associated Specialty Physicians*
ACO Model 1 ACO Model 2 ACO Model 3 ACO Model 4
Independent Practice Association
(IPA) or
Primary Care Physician Groups
Specialty Groups
Multispecialty Group
Hospital
Hospital
Hospital Medical Staff Organization
(MSO) or
Physician-Hospital Organization (PHO)
Organized Delivery System
*Hospital
*Employed and Affiliated Physicians
*Possibly Other Providers, like
Post-Acute Care
*Most care provided by single ACO, but some care will be delivered by other ACOs or regional referral centers like tertiary or quaternary hospitals and their associated specialists, unless a strict beneficiary lock-in is utilized.

Timely Analysis of Immediate Health Policy Issues 4
Key ACO program featuresAlthough various authors and legislative proposals have described the broad outlines of the ACO concept,15 there are many program options and design features that are being actively discussed and debated. Decisions about these ACO program options and features would substantially affect the nature and contours of the ACO program; its implementation, including its scale, pace, challenges, and potentially necessary supports; and short and long-term outcomes with respect to cost reduction and quality improvement. Here we discuss five key issues to watch as ACO program proposals unfold.
Specific ACO definition and qualifying criteria
Legislative proposals in the House and Senate16 both define ACOs quite broadly, but seem to leave important aspects of the ACO concept somewhat unclear or reflect different perspectives on some key issues, including how much of the decisions should be left to the Secretary of HHS. Program design decision issues include which type of provider organization can lead an ACO, in particular whether it must be physician led; what other types of provider organizations may or must be included; what specific ACO qualifying criteria should govern participation; and whether PCMHs can lead or be part of an ACO.
Some believe that physician-centered organizations should lead ACOs because the resources that flow from the decisions physicians make with patients account for a major portion of overall health care costs, regardless of where the care actually takes place. Most existing physician practices, which are solo or small, single specialty groups would not possess the three essential ACO characteristics described above.17 MedPAC and others have suggested that IPAs are an organizational model that would permit even small physician practices to come together to form organizations fulfilling these criteria. Some hold that if a MSG- or IPA-based ACO did not include a hospital, these
physician-based organizations could still be held accountable for the quality and costs associated with hospitalization.
Consistent with the call for flexibility, hospitals or hospital systems (ODSs or IDSs) might also be allowed to lead an ACO. In many communities, hospitals employ a large portion of the physician workforce and they may be more likely to provide capital and management skills that ACOs would require to produce the kind of system redesign needed to methodically improve quality and reduce wasteful care in accord with a spending budget.
Indeed, to address the problem of care fragmentation, some think that local hospitals must be included in an ACO. However, others think that the relationship between physicians and hospitals is becoming so severely strained18 that perhaps we should allow separate outpatient and inpatient ACOs to develop and not force a marriage between feuding partners. While the latter approach might defeat one of the primary purposes of ACOs—accountability for the full continuum of care—it may be more feasible in the short term and potentially allow separate ACOs to come together in the future.19
Similarly, some would want other provider types, such as post acute care facilities and ambulatory surgery centers, to be part of broad ACOs. In contrast, others would not require their inclusion but would want to hold the ACO accountable for the care—and costs—provided across the range of services beneficiaries might need.
The ACO definition and accompanying qualifying criteria delineated in final legislation or demonstration guidance would strongly influence, if not actually determine, what types of organizations would lead or participate in an ACO and how they would have to be legally structured. For example, if an ACO were defined as a physician-led organization and the minimum number of physicians needed set at 200 or more, as in the PGP demonstration, only a relatively small number of existing physician groups,
mostly MSGs, would be able to meet the criteria. Smaller groups would either have to merge or, more likely, would have to form an IPA to participate. Yet, again, the current interest in ACOs arose from a desire to permit even virtual organizations of physicians working in close proximity and serving the same patients to become ACOs and thus permit looser organizations to constitute eligible ACOs.
Some recommend that even very small physician groups, such as those with three to five physicians, should be allowed to serve as ACOs; the Senate Finance Committee Chairman’s Mark also adopts this view.20 However, this approach raises concerns about small practices’ ability to fulfill the three key ACO characteristics described in the introduction and would create a much greater administrative burden for the Centers of Medicare and Medicaid Services (CMS) than a program relying on a smaller number of larger physician groups, IPAs, or provider organizations.
Indeed, it is not clear how the expectations for an ACO with a few physicians differ conceptually from a PCMH, and to what extent ACOs and PCMH programs complement or conflict with each other. The PCMH is an enhanced primary care practice model that provides comprehensive and timely care with appropriate reimbursement, emphasizing the central role of teamwork by a group of health professionals and more active engagement by those receiving care. The PCMH concept not only emphasizes enhanced primary care but also incorporates the ideas of provider payment and delivery system reforms, including primary care providers’ voluntary acceptance of accountability for the quality of care provided to their patients.21 Some believe that ACOs and PCMHs are complementary innovations and discuss ways they could be mutually beneficial and reinforcing.22, 23
Voluntary or mandatory provider participation
The House bill proposes a voluntary ACO provider program24 and MedPAC

Timely Analysis of Immediate Health Policy Issues 5
describes this approach as well.25 That is, an existing provider organization or new configurations of them (see figure 1 and table 1) would have to indicate proactively a desire to participate. If the traditional Medicare program adopts policies that strictly limit provider payment increases, physicians (with or without hospital partners) might want to opt out of the payment constrained FFS program by selecting the alternative ACO pathway that offers them the potential of both expanding their patient base and achieving financial rewards based on their own actual performance. Another reason physicians might voluntarily want to become an ACO is that some physicians do not like the incentives inherent in standard FFS payments and would like to be rewarded for achieving high standards on quality measurement and prudent management of health resources, which should include building stronger partnerships with patients. In short, physicians and other providers might be both pushed and pulled into an ACO program offered by the nation’s largest and most important payer—Medicare.
A voluntary provider program has several potential strengths. First, provider organizations that are able to meet the accountability tests would choose to participate, increasing the likelihood of initial ACO success and providing models for others to emulate. Second, a narrower, voluntary participation program would require fewer resources to administer and oversee initially.
However, relying on voluntary participation might result in relatively little uptake, as occurred with the PSO program. An initiative that is small in scale and involving a unique set of providers might not be particularly relevant to the challenge of fundamentally restructuring payment and practice across the country. In addition, only organizations that feel confident they would earn bonuses might choose to participate, raising concerns that a voluntary ACO program
overall would not generate savings for Medicare.26
Alternatively, in a mandatory provider program, physicians and hospitals would be assigned to a virtual ACO based on analysis of claims data; currently, provider organizations and professionals generally do not know how frequently their patients are flowing to each other’s practices and institutions and may not perceive themselves as having a common interest in caring for these patients. Plausibly, their assignment into the same virtual organization would provide them with this key information and a reason to develop their relationships, a culture of collective responsibility, and an effective governance structure.
Accordingly, there are several positive attributes of a mandatory ACO program. First, it can be much more widely applied than a voluntary program because it should engage most physicians, hospitals, and perhaps other key providers that serve Medicare beneficiaries and would provide them a reason to work together. Because of its much broader application, a mandatory program could result in greater Medicare savings27—but only if the selected payment model in fact succeeds in achieving spending reductions.
On the other hand, a broad program of assigning beneficiaries, physicians, and other providers to statistically determined ACOs would be challenging to administer. In addition, some providers would be reluctant or unprepared to alter their practice patterns to reduce cost and improve quality. Merely providing them a mild financial incentive to change their practice patterns would not guarantee that they would actually change. In addition, the physicians assigned to the ACO would need to develop a common vision of how to achieve their organizational objectives and would have to implement a functional governance structure. Some doubt that these ACO prerequisites would be accomplished in many cases. Indeed,
imposing a requirement that key health care providers participate together in an ACO might only exacerbate conflicts between health care organizations and professionals that have developed over the years, such as those between physicians and hospitals and between primary care physicians and specialists.
How beneficiaries participate in ACOs
Beneficiaries’ reactions to the ACO concept will also be important, because their perceptions would affect whether they will ultimately select ACOs if given an opportunity or whether they will support or oppose them in other ways, such as a through political activity; further, their responses could affect providers’ ability to improve their cost and quality performance. For example, if beneficiaries believe that ACOs are essentially tightly managed “HMOs in drag” that are going to restrict their choices, undermine the doctor-patient relationship, and result in cheaper but lower-quality care, the concept will be met with skepticism, if not overt opposition. On the other hand, if ACOs are viewed as a way to make the health care system easier to navigate and to improve the quality of care, to provide more for their health care dollars, and to put critical health care decisions in the hands of local doctors, hospitals, and the communities and patients they serve, the concept is likely to be more positively received. Whether and how CMS and providers communicate with beneficiaries about these ACO-related issues will influence their response to the innovation, as will two important ACO program features: (1) whether they are assigned to an ACO or, alternatively, are allowed to select participation in an ACO; and (2) whether and to what degree their access to care outside an ACO is restricted in any way.
In some ACO proposals, beneficiaries would be assigned to an ACO based on where claims analysis shows they go for their care; adopting the PGP demonstration approach, they might not even have to be informed of this

Timely Analysis of Immediate Health Policy Issues 6
assignment because their freedom of provider choice would not be restricted in any way. In this case, ACO assignment is coupled with a “no lock-in” feature. Although providers would be managing their care, beneficiaries would not necessarily even know it. Indeed, if beneficiaries’ care patterns change from one year to the next, their ACO assignments would likely change accordingly. There is a slight difference on this issue between the House Tri-Committee’s and Senate Finance Committee’s proposals, with both proposing beneficiary assignment but the House requiring that beneficiaries must be informed of that assignment and the Senate not stipulating that beneficiaries have to be informed.
Beneficiaries may view claims-based assignment and no lock-in positively, because it does not interfere with their choices or existing doctor-patient relationships; further, these features would simplify the administration of an ACO program. On the other hand, if beneficiaries indirectly and retrospectively learn that their provider had an incentive to reduce cost and improve quality, it might undermine trust in their physicians, as some contend that HMOs and managed care potentially does.28 In addition, this no lock-in feature might negatively affect ACOs’ interest in actually managing patients’ care and their ability to actually do so, making it harder to determine which patients and care management processes to focus on to achieve cost and quality targets.
An alternative is to require beneficiaries to affirmatively select an ACO if one exists in the community, much as patients select an HMO network, and to commit to seeking their care from ACO providers for some set time. This option would require more extensive efforts to help beneficiaries and consumers understand what ACOs are and the respective roles and responsibilities that pertain. The mere process of facilitating beneficiary selection of ACOs would be administratively much more complex than a statistically based assignment.
This approach might invoke the need for additional regulatory oversight if ACOs wanted to use techniques to manage care similar to those used by HMOs and the rare PSOs in the Medicare Advantage program.
Because of the concern that a true lock-in would discourage beneficiary participation in what would likely be restricted ACO provider networks, variants of what might be called a soft lock-in have been suggested for ACOs where beneficiaries make an affirmative decision to associate with a particular ACO. A soft lock-in might involve financial incentives, such as differential cost sharing, to encourage beneficiaries to seek care mostly from the ACO they have selected, an approach used in preferred provider organizations and point-of-service plans. A soft lock-in might even be as simple as a good faith social contract between beneficiaries and the ACO, outlining the parties’ responsibilities to each other but otherwise not restricting freedom of choice.
Provider payment methods and financial incentives
While a number of payment models to support ACOs are possible, two very different types of ACO payment methods are included in the current House legislative proposals for testing: a shared savings program (SSP) and partial capitation, based on what some call population-based payment (PBP).29
The basic SSP concept is fairly straightforward and illustrated in figure 2. The FFS system remains intact, so providers continue to be paid on that basis. However, Medicare calculates and sets the expected total expenditures for the patients cared for by the ACO while measuring and assessing the quality of care. If the ACO provides the care its patients need for less than expected and the quality standards are met, the ACO is rewarded with a portion of the savings as a bonus. A variant of the SSP is that some portion of billed for FFS payments are withheld and only returned if the ACO provides the care its patients need for less than expected.30
Figure 2. Shared Saving Program (SSP)
2008 2009 2010 2011 2012 2013 2014
High Spending Area
Projected Spending
Low Spending Area
ACO Program Launch
Actual Spending
Actual Spending
Actual Spending
Savings
Savings*
Savings
Hea
lth C
are
Sp
end
ing
*How any savings would be shared (e.g., 80/20, 50/50, 40/60) by payers and providers has yet to be determined.

Timely Analysis of Immediate Health Policy Issues 7
A critical issue with the SSP payment method is how to calculate and set the expected total expenditures for patients cared for by the ACO. While the PGP demonstration used a control group as the source of expected expenditures, setting up a control group for every ACO would not be administratively feasible, particularly for a large-scale program. As an alternative, MedPAC proposes determining expected total costs and setting benchmarks based on historical spending over a three-year period, adjusted for patient case mix. Yet, even here, there are options that vary on two dimensions: (1) use of local, regional, or national spending; and (2) a focus on base spending, the rate of spending growth, or some combination of the two. Different configurations for setting spending targets would importantly determine the likelihood that any particular ACO would in fact achieve bonuses based on the success of their spending management.31
Whatever variant of the SSP payment options are selected, the anticipated virtue of determining bonuses based on a shared savings approach is that it does not involve financial risk taking, making it more attractive to many would-be ACOs. In addition, SSP should be relatively easy to implement, since the basic FFS payment system remains in place, with determination of bonuses a retrospective accounting matter.
However, there may be a fundamental weakness to the SSP payment method for ACOs—it leaves the “do more, get paid more” incentives of FFS in place. New services or care management approaches that might reduce total expenditures but are not paid for under FFS system, such as greater reliance on nurse care managers for chronic care patients and enhanced patient communication outside of standard office visits by phone or e-mail, may go untried. Otherwise, the ACO would have to finance these activities directly, with uncertain prospects of financial rewards for so doing. It is also hard to see how the prospect of a potential bonus sometime in the future would
counter the real-time FFS incentive to generate more services. The speculative nature of a potential bonus may be too weak to motivate an ACO to commit to innovate, perform well, and sustain gains. Although acknowledging that FFS incentives are a problem, proponents of this approach nevertheless believe that the prospects of a substantial bonus based on achieving overall savings could produce different referral patterns within the ACO such that more care would be channeled to the clinicians who demonstrate more prudent use of health care resources.
In addition, a SSP based on local spending primarily rewards improvement rather than good performance. Communities and providers that have the most to gain from an SSP are the ones seemingly wasting the most resources (see figure 2). Those that are already doing well by being low cost and high quality would have to make greater investments to improve and would be less likely to be rewarded (see figure 2). Indeed, since current SSP models provide no downside risk or penalty to the provider for missing both quality and cost targets, ACOs and affiliated providers would have a perverse incentive to increase utilization and total costs in order to create future opportunities for “savings” and “bonuses.”32
The alternative to SSP specified in the House legislation is partial capitation or a PBP system, where a predetermined amount is prepaid to a provider for the services needed by a specific group of people for a fixed period. Capitation or PBP payment methods encourages providers to think in terms of the resources required to take care of the overall population they are accountable for and involves a greater degree of financial risk for them which is typically greater than any type of SSP with a withhold. More specifically, capitation prepayments are calculated on a per person, per month—per capita—basis.
Historically, financial risk taking by providers raised complex insurance regulation issues, and there have been
numerous problems with capitated payment approaches. Capitation payments to providers generally were not risk-adjusted for patient health status; capitation payment amounts were sometimes driven down to levels providers found inadequate to support needed care; in some contracting situations, no provisions were made for costly cases, which could deplete the capitation funds.33 Providers also executed poorly in many cases because they lacked both administrative and clinical infrastructures needed to effectively manage the amount of financial risk they were assuming.34
Imposed administrative requirements undermined the theoretical simplicity of making a single monthly payment rather than paying claims for each service rendered. For example, physicians often still had to submit “shadow” claims as if they were real. Lastly, when capitation was more widely used in the 1980s and 1990s, there was less measurement and reporting of quality information, leading to a public perception that the financial incentives may have resulted in providers’ stinting on care.
Proponents of retesting capitation hope that these problems with capitation can be overcome and that ACOs offer a more promising programmatic vehicle for direct contracting with Medicare than the failed PSO approach.35 They note MSGs, IPAs, and other organizations’ success in managing capitation in California and elsewhere, and so think that providers with more experience and improved infrastructure are more capable of managing financial risk than a decade ago when the PSO experiment fizzled. With payments based on improved risk-adjustment tools, ACOs, which could well have sicker than average patients if they recruit from their own patient rosters, would not be disadvantaged as would have been the case in the 1990s.
An important variation on the BBA-PSO capitation approach would be the introduction of risk and profit sharing, rather than full-risk contracting to ACOs—that is, partial rather than full

Timely Analysis of Immediate Health Policy Issues 8
capitation. A model here is the Medicare Prescription Drug Program (PDP) established by the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, in which risk corridors were set up to limit a prescription drug plan’s potential losses should the plan happen to experience much higher utilization and costs than expected.36 It could be that with Medicare directly sharing risk under a population-based payment approach, providers would be more likely to participate. And with Medicare’s “deep pockets”, public policy concerns about provider financial solvency would be mitigated.
If properly designed, partial capitation might have a number of theoretical advantages over the SSP payment method. First, ACOs and affiliated providers would have greater incentives and the flexibility to deploy newer services and care management approaches that are not currently covered or paid for in the FFS system. Second, ACOs would receive funds upfront and on a regular basis, facilitating capital and other investments. Third, and most importantly, the nature of the payment provides fundamentally different payment incentives. For example, under an SSP hospitals remain primarily an accounting “profit center” for an ACO; under a capitated, population-based payment model, the hospital essentially becomes a “cost center.” Further, the ACO would have an incentive not only to reduce total costs but also to sustain the improvements over time. Yet, because the ACO must meet the quality targets before they are eligible for retaining their savings, Medicare beneficiaries would have some protection against ACOs stinting on care.
If using capitation, the difficult issues that have caused controversy in determining Medicare Advantage–capitated payments would also arise in determining capitation amounts for ACOs. Would capitation amounts be based on spending in the local area, be ACO specific, or reflect national norms? What would be the basis for
determining annual increases? Aside from these technical issues related to determining ACO payments, the fundamental question is whether there are enough physicians interested in doing the hard work of forming and managing ACOs capable of directly managing even partial capitation risk. It is possible that for all of the theoretical advantages of this approach, there would be few takers in a voluntary ACO program using any form of capitation
Accountability for quality
As already emphasized, whichever payment model is adopted, the financial benefits of achieving cost targets are contingent on quality.37 Thus, another important issue is how quality will be assessed and what level of quality performance or improvement will be required. ACO proponents are concerned that without a serious quality assessment and reporting component, ACOs might emphasize cost cutting rather than improved value. MedPAC suggests that “quality measures and targets could be aggregated into a weighted quality score.”38 CMS could begin with a limited set of existing and appropriate risk-adjusted quality measures, improvements in infrastructure that support quality-improvement efforts such as “meaningful use” of electronic health records, and potentially incorporate and align ACO measures with those used in the PCMH demonstration. Additional quality measures could be added to over time.
There also are benefits of applying quality measures at the ACO level, rather than the individual clinician or facility level. First, measures that capture issues in care coordination across different providers could appropriately be applied to ACOs. Second, aggregation to the ACO level provides adequate numbers to assure a level of statistical validity that is lacking when applied to individual clinicians. Finally, theory —and some empirical data—support the notion that some larger organizations are better able to mount and sustain quality-improvement activities than
smaller organizations or individual health professionals, who are typically consumed with the day-to-day pressures of clinical practice.
Implementation challenges Implementation is always challenging, and decisions about the ACO program features discussed will have a substantial impact on the implementation process. However, there are some core implementation issues that will need to be addressed, regardless of the ACO program specifics.
Participation of, and impact on, other public and private payers
If ACOs provide desirable delivery system enhancements for Medicare, we would hope and possibly expect that they would also be desirable for other payers as well. In fact, some recommend that self-funded employers and commercial insurers should follow Medicare’s lead or collaborate with them on an ACO program initiative. Massachusetts is considering ACOs as way to control health care spending as part of the state’s continued evolution of comprehensive health reform.39 Arguably, such payer collaboration would align and strengthen providers’ financial incentives and avoid conflicting program features and additional administrative burden.
However, an ACO program designed for traditional Medicare beneficiaries, particularly a mandated program based on analysis of Medicare claims data as some proposals call for, might not serve private employers’ or health plans’ interests very well. The pattern of care for employee or health plan enrollees might be quite different from that of Medicare beneficiaries, reflecting referral patterns characteristic of plan-specific provider networks.
Perhaps even more serious, purchasers and plans are concerned that sanctioning the collaboration of most of the physicians with each other, perhaps also with one or more hospitals in a geographic area, would increase providers’ market power and result

Timely Analysis of Immediate Health Policy Issues 9
in substantially increased provider prices gained through negotiated contracts, costing the payers much more than if the providers remained in their fragmented silos. In short, newly empowered ACOs might be well positioned to reduce spending and spending growth for Medicare, but not for commercial insurers and self-funded employers; providers might be able to demand higher payments from private payers even as their own costs go down.
Further, the Federal Trade Commission (FTC) and Department of Justice (DOJ) might actually want to prohibit for antitrust reasons certain ACO entities that Medicare might want to promote (e.g., loosely affiliated physicians and hospitals constituting an ACO under a share saving payment model).40 To date, whether and how ACOs would be allowed to operate in relation to commercial payers, including a possible role for public regulation of private sector prices, have not been explored but likely must be before the ACO concept goes very far.
New roles and responsibilities for providers and government agencies
Clearly, the ACO concept poses a variety of implementation challenges for health care providers and federal government officials. In a new provider payment and delivery system environment—a much more value-focused system—each party would have to change and take on new roles and responsibilities.
To be successful in an ACO program, providers would need to utilize and strengthen a variety of organizational, technical, and clinical skills over time. Some would describe the nature of needed provider changes as truly transformational. Even providers with greater experience with the kinds of payment methods and programs discussed find that it takes time and capacity building in key areas, such as cultural change, managerial and physician leadership, teamwork, health information technology, and care
management process redesign and improvement.41
Prior experience in health care, as well as other industries, provides practical approaches and lessons for helping providers get started and successfully move forward. For example, technical assistance, quality-improvement collaboratives, coaching, and sharing of key resources, information, and tools are likely to be helpful to providers participating in an ACO program. Provider professional associations and consulting firms may provide these kinds of support and assistance to ACOs, but there is potentially a very important role here for Medicare Quality Improvement Organizations (QIO) and other public entities as well.
Federal officials would also need to make changes and develop new capacities to administer an ACO program, and the more providers and beneficiaries involved, the more difficult these changes are to make. In addition to supporting and assisting providers, there are a range of complementary policies that would have to be reviewed and probably altered to permit ACOs to form and succeed. Some include antitrust enforcement, “gainsharing” (profit sharing between hospitals and physicians), state-based insurance regulation, and issues related to professional and organizational liability. Finally, depending on which ACO approaches are being tested, there might need to be extensive education of beneficiaries about their opportunities, responsibilities, and rights.
All of these activities would require time and expertise. They are much more complex and resource intensive than current administrative payment methods, which essentially require uniform application of national payment formulas. Therefore, to embark down the road of even broad pilots and demonstrations of ACOs, Congress would need to assure that CMS would receive adequate resources for supporting the demonstrations
and assuring adequate evaluation and midcourse corrections.
Skeptics arise
Some experienced hands counsel that ACOs are a bad idea—that Congress should not embark down this road at all. In the words of Jeff Goldsmith, a health care consultant who helped put together prior versions of ACOs more than a decade ago, “The problem with this movie is that we’ve actually seen it before and it was a colossal and expensive failure.”42 That experience was related to risk-bearing provider organizations, which imposed restrictions on patients’ freedom of choice. He not only points to the serious problems of execution that plagued these organizations but even more fundamentally challenges the concept itself in concluding that employers and patients preferred open panels managed by health insurers to closed panels managed by providers.
Goldsmith is no less sparing in his criticism of the ACO model that is receiving the most attention now—the shared saving payment approach that does not restrict patient choice or require any providers to take financial risks. He points to the fact that in many medical markets, the physician community has drawn away from the hospital and functions increasingly independently on a day-to-day basis. The weak financial incentives in the SSP payment model, he asserts, would not be able to bring together these increasingly independent professionals, who have interest in preserving the status quo, not participating in substantial collective efforts for nominal shared savings.
Conclusion There is broad policy agreement on, and an evidence base regarding, the need for provider payment and delivery system reforms that create financial incentives for providers to work together to bend the cost curve and improve quality. The ACO proposals are one of the few serious attempts to move ahead to achieve these objectives.

Timely Analysis of Immediate Health Policy Issues 10
However, there are quite different interpretations of the current ACO concept and its predecessors. One view is that the ideas are fundamentally flawed and that the conditions are not right for changes of this kind, and may have even gotten worse since the mid-1980s and 1990s. Another perspective is that the flaws with the concept have or could be overcome, and that some conditions have not only improved, but also can be positively affected by the policy decisions made moving ahead.
ACOs will not be a real game changer in the short run but are definitely worth a concerted try, given long-standing problems with the FFS provider payment and delivery systems that impede health care cost control and quality improvement. ACOs can help overcome the impasse of where to start first—provider payment or delivery system reform—by coupling and coevolving them over time. ACO proposals also offer the opportunity
to harness the tremendous purchasing power of the traditional Medicare program, potentially creating a much greater incentive for providers to begin assuming real accountability and making necessary improvements. In addition, the ACO concept may avoid a one-size-fits-all provider payment or delivery system reform approach, which is unlikely to work given the variation in local markets and provider organizations and their capabilities. Lastly, ACOs can potentially complement other reform initiatives, including the patient-centered medical home, meaningful use of electronic medical records, and comparative effectiveness research.
Nevertheless, there still are very challenging implementation issues that need to be recognized and addressed. In order for ACOs to be a real game changer in the long run, the concept needs to move past the rosy-scenario phase that has become common for energetically endorsed new or reprised
concepts and now confront the many evident challenges. Lessons from previous experiences and ongoing demonstrations can help identify potential solutions to the complex financial, organizational, legal and regulatory issues, and provide insight into the trade-offs between various program proposals and options. In addition, the ability to learn from the early ACO efforts and to make program modifications as necessary will be critical, as it is unreasonable to expect substantial changes to occur without some problems or failures or in the short run.
In sum, there is a ripe opportunity for policymakers and providers to get critical provider payment and delivery system reform processes underway, potentially moving us into a new era in which local physicians and provider organizations have not only the accountability but authority, financial incentives, and capacity to redesign the delivery system to add greater value.
Notes1 Crosson, Francis J. “Medicare: The Place To Start
Delivery System Reform,” [Health Affairs 28, no. 2 (2009): w232–w234 (published online 27 January 2009; 10.1377/hlthaff.28.2.w232)]
2 Throughout this Issue Brief, we use the term accountable care organization (ACO) for simplic-ity because it is the term used in the House Tri-Committee Health Reform Bill (HR 3200), in other proposals and documents out of the Sen-ate, and by MedPac (2009). The term was coined by Fischer et al (2006). However, other terms have been used for similar concepts. Specifically, the term accountable care system (ACS) is the term used by Shortell and Casalino (2007; 2008); “bonus-eligible organization” (BEO) is a term sometimes used by the Congressional Budget Of-fice (CBO); and accountable care entities (ACE) is a term sometimes used by the Medicare Physician Value-Based Purchasing Program. House Tri-Committee Health Reform Bill (HR 3200) July 14, 2009. Available at http://docs.house.gov/edlabor/AAHCA-BillText-071409.pdf, other draft. For Senate documents, see “Description of Policy Options—Transforming the Health Care Delivery System: Proposals to Improve Patient Care and Reduce Health Care Costs. “Senate Finance Committee, April 29, 2009. Available at http://finance.senate.gov/sitepages/leg/LEG%202009/042809%20Health%20Care%20Descrip-tion%20of%20Policy%20Option.pdf. U.S. Senator, Max Baucus, Chairman, Senate Finance Committee, Call to Action: Health Reform 2009, November 12, 2008, Final White Paper,
http://finance.senate.gov/healthreform2009/ finalwhitepaper.pdf. Chairman’s Mark, America’s Healthy Futures Act of 2009, Amended http://finance.senate.gov/ sitepages/leg/LEG%202009/100209_Americas_Healthy_Future_Act_AMENDED.pdf. Kennedy HELP Committee Bill (615 pages). To make quality, affordable health care available to all Americans, reduce costs, improve health care qual-ity, enhance disease prevention, and strengthen the health care workforce. Available at http://help.senate.gov/BAI09A84_xml.pdf. MedPAC, Improving Incentives in the Medicare Program, Chapter 2, Accountable Care Organiza-tions, Washington, DC: June, 2009, http://www.medpac.gov/documents/Jun09_EntireReport.pdf Fisher, Elliott S., and Douglas O. Staiger, Julie P. W. Bynum, and Daniel J. Gottlieb, “Creating Account-able Care Organizations: The Extended Hospital Medical Staff,” Health Affairs 26, no. 1 (2007): w44–w57 (published online 5 December 2006; 10.1377/hlthaff.26.1.w44). Fisher, Elliott S., and Mark B. McClellan, John Bertko, Steven M. Lieberman, Julie J. Lee, Julie L. Lewis, and Jonathan S. Skinner, “Fostering Account-able Health Care: Moving Forward In Medicare,” Health Affairs 28, no. 2 (2009a): w219–w231 (published online 27 January 2009; 10.1377/hlthaff.28.2.w219). Fisher, E., J. Bynum, and J. Skinner. 2009b. “Slowing the Growth of Health Care Costs—Lessons from
Regional Variation.” New England Journal of Medicine 360: 849–852. Shortell, S. M., and L. P. Casalino, “Accountable Care Systems for Comprehensive Healthcare Reform.” Prepared for the workshop “Organization and De-livery of Care and Payment to Providers.” Center for Advanced Study in the Behavioral Sciences, Stanford University, March 1–2, 2007. http://www.rwjf.org/files/research/aresystemsforcomprehen-sivehealthcarereform.pdf. Shortell, S. M. and L. P. Casalino, “Health Care Re-form Requires Accountable Care Systems,” JAMA, 2008; 300(1):95–97 (doi:10.1001/jama.300.1.95). CBO, http://www.whitehouse.gov/omb/blog/09/06/17/CBOPointstheWay/ Center for Medicare and Medicaid Services (CMS), “Roadmap for Implementing Value Based Purchas-ing in the Traditional Medicare Fee-for-Service Program,” http://www.cms.hhs.gov/QualityInitia-tivesGenInfo/downloads/VBPRoadmap_OEA_1-16_508.pdf.
3 Insufficient size makes it difficult to assess the full continuum of care and leads to variation in results because of chance or error, not real cost and qual-ity performance differences. Fisher et al 2009a and MedPac, June 2009 suggest that the minimum size is 5,000 or more beneficiaries.
4 Shortell and Casalino 2007, 2008
5 Shortell and Casalino (2007) mention organized or integrated delivery systems when they discuss multispecialty groups. However, there are a variety of ODS or IDS types, some that have an exclu-

Timely Analysis of Immediate Health Policy Issues 11
sive arrangement with a multispecialty group and some that do not. Similarly, some types of organized or integrated delivery systems include a health plan and some do not. See, for example, the work by Bazzoli et al. (1999), Shortell et al. (2000), and Dubbs et al. (2004) on different types of systems. Bazzoli, G. J., S. M. Shortell, N. Dubbs, C. Chan, and P. Kralovec. “A Taxonomy of Health Networks and Systems: Bringing Order Out of Chaos.” Health Serv Res. 1999 Feb; 33(6): 1683–717. Shortell, S. M., G. J. Bazzoli, N. L. Dubbs, and P. Kral-ovec. “Classifying Health Networks and Systems: Managerial and Policy Implications.” Health Care Manage Rev. 2000 Fall;25(4):9-17. Dubbs, N.L., G. J. Bazzoli, S. M. Shortell, and P. D. Kralovec. “Reexamining organizational configura-tions: an update, validation, and expansion of the taxonomy of health networks and systems. Health Serv Res. 2004 Feb;39(1):207-20
6 Fischer et al, 2006 and 2009a from above (footnote 2).
7 Health care provider organizations that exist today use vertical (i.e., ownership, joint ventures) and virtual (i.e., contractual) integration strategies, emphasizing one or the other or blending them in different ways. However, the “virtual” organiza-tion that Fisher and his team propose is a specific type of virtual provider organization, defined not by how different provider organizations relate to each other but by where beneficiaries or enroll-ees receive their care.
8 The Physician Group Practice (PGP) Demonstra-tion is the first pay-for-performance initiative for physicians under the Medicare program. The dem-onstration creates incentives for physician groups to coordinate the care delivered to Medicare patients, rewards them for improving the quality and cost efficiency of health care services, and creates a framework to collaborate with providers to the advantage of Medicare beneficiaries. CMS selected 10 physician groups on a competitive ba-sis to participate in the demonstration. The groups in the PGP demonstration are large, averaging 500 doctors and 22,000 beneficiaries. They also tend to be tightly managed groups that have the ability to take joint actions to change care protocols, improve quality metrics, and constrain capacity growth. Leavitt, Michael O., Report to Congress, Physician Group Practice Demonstration, First Evaluation Report, Secretary for Health and Human Service, 2006 http://www.cms.hhs.gov/DemoProjectsEval-Rpts/downloads/PGP_Final_Congress.pdf RTI. 2008. Physician Group Practice demonstra-tion selected results from performance year two. Research Triangle Park, NC: RTI. Also see Medicare Physician Group Practice Demonstration Fact Sheet, Center for Medicare and Medicaid Services, August, 2009, http://www.cms.hhs.gov/DemoProjectsEvalRpts/downloads/PGP_Fact_Sheet.pdf. Sibelius, Kahtleen, Report to Congress, Physician Group Practice Demonstration, Secretary for Health and Human Service, 2009 http://www.cms.hhs.gov/DemoProjectsEvalRpts/downloads/PGP_RTC_Sept.pdf
9 Fisher 2009 above (footnote 2)
10 The most recent MedPAC Report to Congress (June, 2009, full citation above in footnote 2)
reflects this genesis of the ACO concept, particu-larly the convergence of Fisher’s work and lessons from the PGP demonstration.
11 House Resolution 3200, Tri-Committee Health Reform Bill. July 14, 2009. Available at http://docs.house.gov/edlabor/AAHCA-BillText-071409.pdf.
12 Senate Finance Committee Chairman’s (Baucus) Proposal above (footnote 1).
13 Clinton, B. The President’s Health Security Plan: The Complete Draft and Final Reports of the White House Domestic Policy Council. New York: Times Books, 1993 Iglehart, JK. Managed competition. New England Journal of Medicine, 1993: 328: 1208-12. Emanuel, L. and S. Latham, M. Ile, J. Munson, J. Berg, and E. Emanuel, “Bringing Market Medicine to Professional Account”, JAMA, March 26, 1997; 277(12): 1004 – 1005.
14 Hirshfeld, Edward. Assuring the Solvency of Provider Sponsored Organizations. Health Affairs 15(3): 28-30. 1996. Kongstvedt, PR, The Managed Health Care Hand-book, 4th edition, Gaithersburg, Maryland: Aspen Publications, 2001
15 Besides the House Tri-Committee Health Reform Bill, see the documents cited below from the Senate Finance Committee and proposed legisla-tion from the Senate HELP Committee, which discusses the ACO concept. See Description of Policy Options—Transform-ing the Health Care Delivery System: Proposals to Improve Patient Care and Reduce Health Care Costs. Senate Finance Committee, April 29, 2009. Available at: http://finance.senate.gov/sitepages/leg/LEG%202009/042809%20Health%20Care%20Description%20of%20Policy%20Option.pdf. U.S. Senator, Max Baucus, Chairman, Senate Finance Committee, Call to Action: Health Reform 2009, November 12, 2008, Final White Paper, http://finance.senate.gov/healthreform2009/final-whitepaper.pdf Chairman’s Mark, America’s Healthy Futures Act of 2009, Amended http://finance.senate.gov/sitepag-es/leg/LEG%202009/100209_Americas_Healthy_Future_Act_AMENDED.pdf. Kennedy HELP Committee Bill (615 pages). To make quality, affordable health care available to all Americans, reduce costs, improve health care qual-ity, enhance disease prevention, and strengthen the health care workforce. Available at: http://help.senate.gov/BAI09A84_xml.pdf.
16 HR 3200, first cited above in footnote 2.
17 Forty-seven percent of all U.S. physicians practice in medical groups with five or fewer physicians. Thirty-two percent of physician practice in solo or two-physician practices, and fifteen percent practice in groups with three to five physicians. Boukus, E. A. Cassil, and A.S. O’Malley, A Snapshot of U.S. Physicians: Key Findings from the 2008 Tracking Physician Survey, Center for Studying Health System Change, Data Bulletin, No. 35, September, 2009
18 Berenson, R., P. Ginsburg, and J. May, Hospital-Physician Relations: Cooperation, Competition, Or Separation? Health Affairs, Published online December 5, 2006;
Goldsmith J., Hospitals and Physicians: Not a Pretty Picture, Health Affairs, Published online December 5, 2006. Burns, LR, Nash, DB, and Wholey, DR, The Evolving Role of Third Parties in the Hospital Physician Relationship, Am J of Med Qual, 2007. Nov-Dec;22(6):402-9
19 See for example Dove, J.T, W.D. Weaver, and J. Lewin, Delivery System Reform: Accountable Care Organizations, Journal of the American College of Cardiology, v. 54, no. 11, forthcoming (September 2009)
20 Fisher et al 2009a from above (footnote 2).
21 See, for example, the Joint Principles of the Patient Centered Medical Home (PCMH), written by the American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), and the American Osteopathic Association (AOA), written and endorsed in February, 2007 at http://www.pcpcc.net/content/joint-principles-patient-centered-medical-home. Robert Graham Center, The Patient Centered Medical Home: History, Seven Core Features, Evidence, and Transformational Change, Novem-ber, 2007, http://www.graham-center.org/PreBuilt/PCMH.pdf. Iglehart, J., No Place Like Home—Testing A New Model of Care Delivery, NEJM, September 18, 2008, v. 358, no. 12: 1200-1202 Rittenhouse, DR and SM Shortell, The Patient-Centered Medical Home: Will It Stand the Test of Health Reform? JAMA, May 20, 2009, v. 301, no. 19: 2038-2040
22 Rittenhouse, D.R., S.M. Shortell, and E.S. Fisher, “Primary Care and Accountable Care – Two Es-sential Elements of Delivery System Reform,” New England Journal of Medicine, October 28, 2009, www.NEJM.org and http://healthcarereform.nejm.org/
23 The House Tri-Committee’s draft legislation has a “no duplication in pilot participation” clause, which states that a physician in a group practice that participates in the PCMH pilot program will not be eligible to participate in the ACO pilot pro-gram. Whether this restriction reflects a judgment that PCMHs represent a fundamentally different approach that should not be intermingled with ACOs or, more pragmatically, is designed to sup-port a demonstration strategy permitting clear-cut evaluations of different approaches (which then might be merged subsequently) is not clear. If not changed, the clause in the House draft legisla-tion might create a conflict between these two programs and force some primary care practices and physicians (PCPs) to choose to participate in one or the other program.
24 HR 3200, first cited above in footnote 2.
25 MedPac, June 2009 first cited above in footnote 2.
26 MedPac June, 2009, pg. 48, first cited in 2 above.
27 MedPac June 2009 report first cited in 2 above
28 See for example: Mechanic, D and Schlesinger, M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA. 1996 Jun 5;275(21):1693-7 Miller TE, Sage WM. Disclosing physician financial incentives. JAMA. 1999 Apr 21;281(15):1424-30 Hall MA, Dugan E, Balkrishnan R, Bradley D. How disclosing HMO physician incentives

Timely Analysis of Immediate Health Policy Issues 12
affects trust. Health Aff (Millwood). 2002 Mar-Apr;21(2):197-206. Pearson SD, Kleinman K, Rusinak D, Levinson W. A trial of disclosing physicians’ financial incen-tives to patients. Arch Intern Med. 2006 Mar 27;166(6):623-8 Miller TE, Horowitz CR. Disclosing doctors’ incentives: will consumers understand and value the information? Health Aff (Millwood). 2000 Jul-Aug;19(4):149-55 Kao AC, Zaslavsky AM, Green DC, Koplan JP, Cleary PD. Physician incentives and disclosure of payment methods to patients, J Gen Intern Med. 2001 Mar;16(3):181-8
29 See section on population based health (pg. 94) in Institute of Medicine (IOM), Performance Mea-surement: Accelerating Improvement, Washington, DC: National Academies Press, 2006.
30 The SSP approach is based on the one used in the PGP demonstration, in which Parts A and B but not D spending for the medical group was compared to spending for a control population in the same geographic area. The spending for the control group became the projected expenditures to determine whether the group received a bonus.
31 For example, expenditure targets to determine eligibility for bonuses could be based on a local area or ACO-specific data, with a focus on the rate of spending growth. Alternatively, one could use a national spending norm and focus on absolute spending. Use of local trends or ACO-specific data might reward savings but would accept the historical geographic differences in costs. Some might view this as advantaging those areas and ACOs with high baseline spending (see figure 2—top trend line and related savings in red). In contrast, using national levels to calculate and set total expenditure targets would address unwar-ranted geographic variation, but such targets might not be achievable for many providers in traditionally high-cost areas. Further, recent work suggests there is not a good correlation between baseline spending and spending growth, and it is not inherently clear which spending parameter should be emphasized in an SSP. Basing rewards on targets of spending growth might have the per-verse effect of rewarding high–baseline spending ACOs that successfully come in under their target based on high prior-year spending growth while not rewarding ACOs with low baseline spending that happen to have targets based on low prior-year spending growth.
32 See for Miller , HD, How to Create Accountable Care Organizations, Center for Healthcare Quality & Payment Reform, www.CHQPR.org, 2009, on these and other problems with the SSP provider payment model.
33 Goroll AH, Berenson RA, Schoenbaum SC, and Gardner LB, Fundamental Reform of Payment for Adult Primary Care: Comprehensive Payment for Comprehensive Care. Journal Of General Inter-
nal Medicine, 2007 Mar;22(3):410-5. Hurley, R., J. Grossman, T. Lake, and L. Casalino, A Longitudinal Perspective On Health Plan–Provider Risk Contracting, Health Affairs, v.24 (4), July-August, 2002: pp.144-153.
34 As Hurley et al (2002) point out, financial risk involves both (1) actuarial or insurance risk that is subject to random fluctuations providers have no control over and (2) more technical risk for the cost of care that providers have more control over, although patient decisions also have a significant impact. A key challenge is how to put providers at technical risk, for example, for avoidable costs but not subject them to any or little actuarial or insurance risk. Several refinements to capitated payments have been developed—such as better risk adjustment, exclusion of high-cost cases, and establishment of risk corridors—in an attempt to achieve this aim. Other provider payment meth-ods have also been developed in an attempt to achieve similar aims—to give providers a financial incentive for technical risk and associated avoid-able costs while eliminating or minimizing any actuarial or insurance risk over which they have no control. See, for example, the discussion of alternative provider payment methods in: Rosenthal, M. Beyond Pay for Performance: Emerg-ing Models of Provider Payment Reform: New Eng-land Journal of Medicine, September 18, 2009, 359 (12): 1197-1200
35 The BBA provided for PSOs to be state licensed as insurers but provided a fallback mechanism to al-low theCMS to license them directly if necessary, guided by somewhat lesser solvency and enroll-ment requirements.
36 Risk corridors may make an ACO program more attractive for providers to participate in, as they did in the case of the prescription drug program (PDP), because they reduce risk associated with new programs and payment methods or random fluctuations in cost. Risk corridors are centered on a target point, such as the total annual insur-ance premiums (excluding administrative costs) in the PDP program or the total annual projected expenditures for care in an ACO program. Gains or losses within a given percentage above or below the target point are assumed by the insurer or pro-vider. Gains or losses beyond the established risk corridor are shared by the payer, in this case, CMS. For example, if the target amount were set at $10,000, and a provider assumed full risk for costs 10 percent above or below that amount, the provider would keep the gains or savings if costs totaled $9,000 to $10,000 and would assume the losses if they totaled $10,000 to $11,000. If costs fell below $9,000, the gains or savings would be shared by the provider and CMS in predetermined percentages (e.g., 50/50), and if costs exceeded $11,000, the losses would also be shared (e.g., 50/50).
37 This has been well described for the Shared Sav-ings Program, but in a partial capitation payment model, the mechanism for doing this would need to be worked out.
38 MedPac, June 2009 report first cited in 2 above
39 Kowalczyk, L, Pay for Care a New Way, State is Urged, Boston Globe, July 17, 2009 http://www.boston.com/news/local/massachusetts/articles/2009/07/17/pay_for_care_a_new_way_state_is_urged/?page=1 Kowalczyk, L. Hospitals attack state pay proposal: Call cost-curbing plan unrealistic; Say changes should be gradual October 4, 2009, The Boston Globe http://www.boston.com/news/local/massachusetts/articles/2009/10/04/health_execu-tives_wary_of_proposed_payment_system_ap-peal_to_patrick/ Recommendations of the Special Commission on the Health Care Payment System http://www.mass.gov/?pageID=eohhs2terminal&L=4&L0=Home&L1=Government&L2=Special+Commissions+and+Initiatives&L3=Special+Commission+on+the+Health+Care+Payment+System&sid=Eeohhs2&b=terminalcontent&f=dhcfp_pay-ment_commission_payment_commission_final_report&csid=Eeohhs2 Payment Reform Commission Unanimously Sup-ports Move to Global Payment System to Improve Patient Care and Contain Health Care Costs http://www.mass.gov/?pageID=eohhs2modulechunk&L=4&L0=Home&L1=Government&L2=Special+Commissions+and+Initiatives&L3=Special+Commission+on+the+Health+Care+Payment+System&sid=Eeohhs2&b=terminalcontent&f=dhcfp_payment_commission_pr_2009_07_16&csid=Eeohhs2
40 Casalino, LP. The Federal Trade Commission, Clini-cal Integration, and the Organization of Physician Practice Journal of Health Policy, Politics and Law. 2006, 31(3): 569-585.
41 Casalino L, Gillies RR, Shortell SM, Schmittdiel JA, Bodenheimer T, Robinson JC, Rundall T, Oswald N, Schauffler H, Wang MC, External incentives, infor-mation technology, and organized processes to im-prove health care quality for patients with chronic diseases, JAMA. 2003 Jan 22-29;289(4):434-41 Bodenheimer T, Wang MC, Rundall TG, Shortell SM, Gillies RR, Oswald N, Casalino L, Robinson JC. What are the facilitators and barriers in physician organizations’ use of care management processes? Jt Comm J Qual Saf. 2004 Sep;30(9):505-14.
42 Goldsmith, J. The Accountable Care Organiza-tion: Not Ready For Prime Time, Health Affairs Blog, August 17, 2009 http://healthaffairs.org/blog/2009/08/17/the-accountable-care-organiza-tion-not-ready-for-prime-time/

Timely Analysis of Immediate Health Policy Issues 13
The views expressed are those of the authors and should not be attributed to any campaign or to the Robert Wood Johnson Foundation, or the Urban Institute, its trustees, or its funders.
Information about the Authors and AcknowledgementsKelly J. Devers, Ph.D., is a Senior Fellow and Robert A. Berenson, M.D., is an Institute Fellow at the Urban Institute.
This research was funded by the Robert Wood Johnson Foundation. The authors thank Stan Dorn and John Holahan for their comments and suggestions.
About the Urban InstituteThe Urban Institute is a nonprofit, nonpartisan policy research and educational organization that examines the social, economic, and governance problems facing the nation.
About the Robert Wood Johnson FoundationThe Robert Wood Johnson Foundation focuses on the pressing health and health care issues facing our country. As the nation’s largest philanthropy devoted exclusively to improving the health and health care of all Americans, the Foundation works with a diverse group of organizations and individuals to identify solutions and achieve comprehensive, meaningful, and timely change. For more than 35 years, the Foundation has brought experience, commitment, and a rigorous, balanced approach to the problems that affect the health and health care of those it serves. When it comes to helping Americans lead healthier lives and get the care they need, the Foundation expects to make a difference in your lifetime. For more information, visit www.rwjf.org.

American Academy of Family Physicians (AAFP) American Academy of Pediatrics (AAP) American College of Physicians (ACP)
American Osteopathic Association (AOA)
Joint Principles of the Patient-Centered Medical Home March 2007
Introduction The Patient-Centered Medical Home (PC-MH) is an approach to providing comprehensive primary care for children, youth and adults. The PC-MH is a health care setting that facilitates partnerships between individual patients, and their personal physicians, and when appropriate, the patient’s family. The AAP, AAFP, ACP, and AOA, representing approximately 333,000 physicians, have developed the following joint principles to describe the characteristics of the PC-MH. Principles
Personal physician - each patient has an ongoing relationship with a personal physician trained to provide first contact, continuous and comprehensive care.
Physician directed medical practice – the personal physician leads a team of individuals at the practice level who collectively take responsibility for the ongoing care of patients. Whole person orientation – the personal physician is responsible for providing for all the patient’s health care needs or taking responsibility for appropriately arranging care with other qualified professionals. This includes care for all stages of life; acute care; chronic care; preventive services; and end of life care.
Care is coordinated and/or integrated across all elements of the complex health care system (e.g., subspecialty care, hospitals, home health agencies, nursing homes) and the patient’s community (e.g., family, public and private community-based services). Care is facilitated by registries, information technology, health information exchange and other means to assure that patients get the indicated care when and where they need and want it in a culturally and linguistically appropriate manner.
Quality and safety are hallmarks of the medical home:
Practices advocate for their patients to support the attainment of optimal, patient-centered outcomes that are defined by a care
Page 1 of 3

planning process driven by a compassionate, robust partnership between physicians, patients, and the patient’s family.
Evidence-based medicine and clinical decision-support tools guide decision making
Physicians in the practice accept accountability for continuous quality improvement through voluntary engagement in performance measurement and improvement.
Patients actively participate in decision-making and feedback is sought to ensure patients’ expectations are being met
Information technology is utilized appropriately to support optimal patient care, performance measurement, patient education, and enhanced communication
Practices go through a voluntary recognition process by an appropriate non-governmental entity to demonstrate that they have the capabilities to provide patient centered services consistent with the medical home model.
Patients and families participate in quality improvement activities at the practice level.
Enhanced access to care is available through systems such as open scheduling, expanded hours and new options for communication between patients, their personal physician, and practice staff.
Payment appropriately recognizes the added value provided to patients who have a patient-centered medical home. The payment structure should be based on the following framework:
It should reflect the value of physician and non-physician staff patient-centered care management work that falls outside of the face-to-face visit.
It should pay for services associated with coordination of care both within a given practice and between consultants, ancillary providers, and community resources.
It should support adoption and use of health information technology for quality improvement;
It should support provision of enhanced communication access such as secure e-mail and telephone consultation;
It should recognize the value of physician work associated with remote monitoring of clinical data using technology.
It should allow for separate fee-for-service payments for face-to-face visits. (Payments for care management services that fall outside of the face-to-face visit, as described above, should not result in a reduction in the payments for face-to-face visits).
It should recognize case mix differences in the patient population being treated within the practice.
Page 2 of 3

It should allow physicians to share in savings from reduced hospitalizations associated with physician-guided care management in the office setting.
It should allow for additional payments for achieving measurable and continuous quality improvements.
Background of the Medical Home Concept The American Academy of Pediatrics (AAP) introduced the medical home concept in 1967, initially referring to a central location for archiving a child’s medical record. In its 2002 policy statement, the AAP expanded the medical home concept to include these operational characteristics: accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective care. The American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) have since developed their own models for improving patient care called the “medical home” (AAFP, 2004) or “advanced medical home” (ACP, 2006). For More Information: American Academy of Family Physicians http://www.futurefamilymed.org American Academy of Pediatrics: http://aappolicy.aappublications.org/policy_statement/index.dtl#M American College of Physicians http://www.acponline.org/advocacy/?hp American Osteopathic Association http://www.osteopathic.org
Page 3 of 3

PHYSICIAN PRACTICE CONNECTIONS®– PATIENT-CENTERED MEDICAL HOME (PPC-PCMH™)
RECOGNIZING PHYSICIAN PRACTICES AS MEDICAL HOMES
NCQA’s Physician Recognition Programs identify physicians who deliver superior care using standards firmly rooted in medical evidence. To date, nearly 10,000 physicians nationwide have been recognized by NCQA in the areas of diabetes care, cardiovascular care, back pain care and practices that systematically provide preventive and chronic care. On January 2, 2008, NCQA released standards for Physician Practice Connections®–Patient‐Centered Medical Home (PPC‐PCMH™). This program builds upon NCQA’s current Physician Practice Connections program to identify primary care practices that function as patient‐centered medical homes. Why the Patient‐Centered Medical Home? WHAT IS A MEDICAL HOME?
The patient‐centered medical home is a model for care provided by physician practices that seeks to strengthen the physician‐patient relationship by replacing episodic care based on illnesses and patient complaints with coordinated care and a long‐term healing relationship. The American College of Physicians, the American Academy of Family Practice, the American Academy of Pediatrics and the American Osteopathic Association have jointly defined the medical home as a model of care where each patient has an ongoing relationship with a personal physician who leads a team that takes collective responsibility for patient care. The physician‐led care team is responsible for providing all the patient’s health care needs and, when needed, arranges for appropriate care with other qualified physicians. A medical home also emphasizes enhanced care through open scheduling, expanded hours and communication between patients, physicians
The patient‐centered medical home is a model of care that holds significant promise for better health care quality, improved involvement of patients in their own care and reduced avoidable costs over time. The precepts of the medical home are articulated in the Joint Principles of the Medical Home developed by the primary care medical societies (see sidebar, right) and measured by the PPC‐PCMH program. How does PPC‐PCMH compare with PPC? PPC‐PCMH builds upon NCQA’s Physician Practice Connections (PPC) Recognition Program. The programs share many requirements; both have nine generally similar standards, score on a scale of 100 points and have three possible levels of Recognition. Notable differences between the programs are highlighted below:
• For PPC‐PCMH Recognition, practices “must pass” at least five basic elements (two for PPC).

• Some elements differ between the two versions. Most notably, a standard on interoperability in PPC has been changed for PPC‐PCMH to assess advanced electronic communications with and about patients.
• The relative weighting of certain elements differ between the two programs. • Minor changes to the standards make them more universal to primary care practice,
making it feasible for more practices (e.g., pediatric practices) to participate. What does PPC‐PCMH measure? Among the aspects of care measured by PPC‐PCMH:
• Access and Communication • Patient Tracking and Registry Functions • Care Management • Patient Self‐Management Support • Electronic Prescribing
• Test Tracking • Referral Tracking • Performance Reporting and Improvement • Advanced Electronic Communications
Why apply? Many private and public health plans and employers are considering projects to Recognize and compensate practices as patient‐centered medical homes. The AAFP, AAP, ACP and AOA support the use of PPC‐PCMH within medical home demonstration projects. PPC‐PCMH Recognition demonstrates that a physician practice is a patient‐centered medical home and NCQA broadly publicizes Recognized physicians. And where select demonstration programs are in place, practices earning PPC‐PCMH Recognition may qualify for additional payment. Bridges to Excellence considers PPC‐PCMH Recognition to satisfy their requirements to qualify for Physician Office Link rewards in the same way as PPC Recognition. Should I apply for PPC or PPC‐PCMH Recognition? PPC Recognition satisfies requirements for a number of programs, including Bridges to Excellence. Practices seeking designation as a patient‐centered medical home should apply for PPC‐PCMH. PPC‐PCMH will satisfy requirements for some programs presently in existence and a number of demonstration programs currently in development. NCQA is developing a process by which practices Recognized for PPC can be re-evaluated for PPC-PCMH Recognition.
FOR MORE INFORMATION ABOUT PPC-PCMH, VISIT WWW.NCQA.ORG OR CONTACT NCQA CUSTOMER SUPPORT AT (888) 275-7585.
For more information about NCQA, visit us on the Web at www.ncqa.org.

Board of Managers meeting
August 4, 2010
AGENDA ITEMS 3 (No Backup)
3. Confirm the next regular Board meeting date, time, and
location.









![QCC ITSV 001 001 IT Software Validation[1]](https://static.fdocuments.net/doc/165x107/577d2a881a28ab4e1ea9710a/qcc-itsv-001-001-it-software-validation1.jpg)



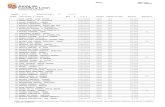



![BENGALURU CENTRAL UNIVERSITY · BENGALURU CENTRAL UNIVERSITY Central College Campus, Dr. B. R. Ambedkar Veedhi, Bengaluru -560 001 College : [ 1827 ] Vijaya College, Basavanagudi](https://static.fdocuments.net/doc/165x107/5f7232dee2cc56738026b159/bengaluru-central-university-bengaluru-central-university-central-college-campus.jpg)

