00463528 Fb Abb 61680000000
-
Upload
iqbal-harziky -
Category
Documents
-
view
216 -
download
4
description
Transcript of 00463528 Fb Abb 61680000000
-
Copyr
The anesthesia team of the futureKarsten Bartels, Atilio Barbeito and G. Burkhard Mackensen
IntroductionChanging clinical demands, technological advances, andthe extension of anesthetic care across the entire peri-operative continuum are redefining the current practiceof anesthesia. Developments such as large-scale patientsafety initiatives, availability of credentialed subspecialtytraining programs, increasing utilization of electronichealth records (EHRs), the implementation of outcomes-based evidence into clinical practice, as well as the estab-lishment of value-based purchasing in healthcare willcontinue to affect how we provide care for our patients.Meeting the challenge of improving cost-effective peri-operative clinical care, engaging in high-quality research,and advancing educational opportunities for our traineesnecessitates a broad vision for the anesthesia team ofthe future. This review considers the current and futureclinical practice patterns of the perioperative anesthesiateam, discusses the impact of technology on how this teamoperates and utilizes information, and describes to whatextent these developments can be translated into novelconcepts that include epidemiologic considerations.
Clinical practice
The ovprovide
perioperative care. These aims are a reflection of a passio-nate commitment to the care of surgical or critically illpatients as well as those in acute or chronic pain, and ourcommitment to continually improve the anesthetic carewe provide. The anesthesia care team is directed byan anesthesiologist and consists of physicians, includinganesthesiologists, fellows, and resident physicians in train-ing as well as nonphysicians such as anesthesia assistants,physician assistants, and specialized registered nurses,including advanced practice registered nurse practitioners(ARNPs), certified registered nurse anesthetists (CRNAs),and pain management specialist registered nurses [1]. Allthese care providers take on unique tasks in the preopera-tive clinic, inside the operating room, the postoperativecare unit (PACU), the ICU, or the pain clinic. Increasingly,they also find themselves performing cases in nontradi-tional anesthetizing locations such as gastroenterologysuites, the electrophysiology laboratory, or the hybridoperating room. In addition, some countries, such asDenmark, France, Germany, Israel, and Norway, have along tradition of having physicians, often anesthesiologistswith additional training in emergency medicine, deliverprehospital emergency care [2,3].
DepartmenMedical Ce
CorrespondFASE, Ass3094 AnesDurham, NTel: +1 91e-mail: b.m
Current O24:68769
ght
ia
futu
Ce
der
yst
lic
h o
rat
ena
tco
utu
pe
ta a
ive
pinc
0952-790erarching goals of the anesthesia team are tohigh-quality, cost-effective, and well tolerated
Anesthesiologists have chosen to enhance their skills toprovide the best perioperative care possible. This has led
7 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins DOI:10.1097/ACO.0b013e32834c15b6t of Anesthesiology, Duke Universitynter, Durham, North Carolina, USA
ence to G. Burkhard Mackensen, MD, PhD,ociate Professor of Anesthesiology, Boxthesiology, Duke University Medical Center,C 27710, USA9 684 6025; fax: +1 919 681 8993;[email protected]
pinion in Anesthesiology 2011,2
Purpose of reviewThis review is aimed at highli
likely to impact the anesthes
Recent findings
The anesthesia team of the
effective perioperative care.
a diverse team of care provi
of electronic health record s
clinical decision support app
enhanced efficiency, researc
perioperative period. Periope
of anesthesiology ultimately
information into improved ou
Summary
The anesthesia team of the f
across the entire domain of
systems rely on accurate da
and recommendations.
Keywords
anesthesia team, perioperat
Curr Opin Anesthesiol 24:687692 2011 Wolters Kluwer Health | Lip0952-7907ight Lippincott Williams & Wilkins. Unauthorizeing the recent developments and opportunities that are
team of the future.
re aims to provide well tolerated, efficient, and cost-
rtified and subspecialty trained anesthesiologists lead
s in increasingly dissimilar environments. The spread
ems has been the basis for the development of
ations that promise to integrate quality control,
pportunities, and improved patient care in the
ive epidemiology is a likely area of growth within the field
bling the anesthesia team to translate precise real-time
me.
re will require the anesthesiologist to provide expertise
rioperative medicine. Meaningful decision support
nalysis and incorporation of current clinical guidelines
epidemiology, perioperative medicine
ott Williams & Wilkinsd reproduction of this article is prohibited.
-
Copyrig
to formalized didactic curricula and certification of specialcompetence in anesthesia subspecialties other than painmedicinAnestheor is iin pediaemergeCouncilcurrentlmedicinlogy ananesthebut notperiope
The pratime anopportuto reduSuch staccompencomppreoperDespiteimproveperiopeives towthe opetings), aof clinicoperativpreoperstatus,profile fin the pfactorsa periopany esseevaluatiimplantfunctionment dand maIndividuceduralpostdiscpatientsThe demedicinall speccriticallof the f
Despitecare is speriope
ldanlopugrytiaosttiliytotlyeslyndntduy. Plartyprinbevaa Pharofirmdes,ageng-thnindustries such as aviation, nuclear power, andmilitary have long recognized the advantages oflation for training, assessment of competence, andrch and development. On the basis of the beliefsimulation may offer similar benefits to healthcare,al countries have called for simulation to becomempulsory part of training. In Australia and Newnd, The Australian and New Zealand Collegenesthetists (ANZCA) established the Effectiveagement of Anesthetic Crises (EMAC) course in[11], which is now a training requirement and widely
688 Technology, education, training, and information systems
Key points
Incorporating evidence-based medicine algorithmsntoheerorheatiohempivepee and critical care: The Scandinavian Society ofsiology and Intensive Care Medicine recognizesmplementing advanced educational programstric anesthesia, obstetric anesthesia, and criticalncy medicine [4]. In the USA, the Accreditationfor Graduate Medical Education (ACGME)
y certifies fellowship programs in critical caree, pain medicine, adult cardiothoracic anesthesio-d pediatric anesthesiology and soon obstetricsiology. Further subspecialty training is availablelimited to regional anesthesia, neuroanesthesia,rative echocardiography, and hyperbaricmedicine.
ctice of perioperative medicine has evolved overd is expected to present new challenges andnities. Standardization of medical practice aimsce healthcare cost while improving outcomes.andardization in perioperative medicine may belished by introducing clinical pathways thatass the entire perioperative period from theative evaluation to the postdischarge disposition.published evidence that these clinical pathwaysoutcome [5,6], they are widely underutilized in
rative medicine. This is where customized initiat-ards procedure-specific, location-specific (insiderating room and outside the operating room set-nd patient-specific care permit the amalgamational pathway approaches with individualized peri-e care. Individualized care starts with a thoroughative evaluation of the patients current medicalwhich is important to establish a clinical riskor the planned procedure. Credentialed providersreoperative clinic not only recognize relevant risk(e.g., coronary artery disease as a risk factor forerative myocardial infarction), but also completential diagnostic steps such as echocardiographicons, interrogation of pacemakers and automaticable cardioverter defibrillators, or pulmonarytests. In concert, these activities lead to treat-
ecisions that permit preoperative optimizationy influence short-term and long-term outcomes.alization continues throughout the entire pro-aspects of care and may reach well into theharge period, such as in ambulatory surgerywho benefit from postoperative pain services.
velopment of clinical pathways in perioperativee will only succeed in tight collaboration withialties involved, but their implementation willy depend on the leadership of the anesthesia teamuture.
the growing perception that modern anesthesiaufficiently well tolerated, many would agree thatrative care is ultimately not as safe or reliable as
it couanddeveAlthosurgepotenof pBy uthe crecenroachnameremipreveprocesafetvascuSocieinghaveto adthesi1985nonpbe hainclualarmManof locare,rely oKeythesimureseathatsevera coZealaof AMan2002
it
Pf
Tl
Titsht Lippincott Williams & Wilkins. Unauthorizedbe. In addition, long-term effects of both surgeryesthesia require innovative research efforts toeffective strategies that secure long-termbenefits.h the profound proinflammatory response tomay be important for wound healing, it also hasl negative implications for the developmentoperative pain and other surgical outcomes.zing perioperative immunomodulation to bluntkine response to surgical incision, Hu et al. havedemonstrated how novel translational app-
may be employed to affect surgical morbidity,postoperative pain [7,8]. Examples of this natureus to investigate interventions designed tolong-term adverse effects from undergoing are in addition to improving immediate patientrograms such as the Flawless Operative Cardio-Unified Systems (FOCUS) initiative by the
of Cardiovascular Anesthesiologists aim at utiliz-ciples of human systems engineering, whichen successfully applied by the aviation industry,nce perioperative patient safety [9]. The Anes-atient Safety Foundation (APSF) launched ins a significantly longer history as an independentt corporation with the vision that no patient shalled by anesthesia. Recent initiatives of the APSFimproved medication safety, audible physiologicstandardization of Anesthesia Information
ment Systems (AIMSs), and the considerationterm outcomes. As we strive to further improvee anesthesia team of the future will also have tothe development of standards for simulation [10].
all aspects of perioperativemedicine will defineanesthesia team of the future.ioperative epidemiology poses an opportunityimproved patient care, research, and education.anesthesia team of the future employs simu-n-based training and quality assurance systems.anesthesia team of the future needs to lead thelementation of clinical pathways in periopera-medicine in tight collaboration with all
cialties involved. reproduction of this article is prohibited.
-
Copyr
used in continuous professional development. Trainingof future generations of anesthesia providers and con-tinuingand critsimulatisimulatiand themethodquality
Techno
The ansubstancollectiotime dadecisioncollectioa concepracticecharts afor aneoperatin[12,13].completlogic putilizedreal-timinitiativof prophas reviethetic rintegratmated dalso beeroom. Fassessmsettingsalerts tdecreasanical velectronon periexpand.up-to-dlated msignificarely solelikely tocell phpatientsused toneed fo[18]. Paday 1 fomanagesystem
An ambitious but desirable goal would be to continuouslycollect patient parameters throughout their hospital
anionneMSdeproy as.rt eandecolortd
upAmuersrenin
omovedel ctorevanoluucutitivpeoterchimll naliainusatedey
pe
etilesike
teforhan
The anesthesia team of the future Bartels et al. 689medical education (CME) in anesthesiologyical care management will increasingly rely onon-based education and training. Ultimately,on-based assessment of anesthesia providersanesthesia team offers an objective and reliableto guarantee continued improvement of the
of care for patients.
logy
esthesia team of the future will likely drawtial amounts of patient data from automated datan systems. More recently, the addition of real-ta analysis has spurred applications for clinicalsupport systems. Integrating automated datan with analysis and decision support has beenpt applied throughout the realm of anesthetic: AIMSs continue to replace traditional papernd are becoming a de facto standard of caresthesia services provided preoperatively in theg room, the PACU, ICU, and at remote locationsIn addition to providing a more accurate ande reflection of the patients perioperative physio-arameters, AIMS-generated data have beento improve anesthetic care at various levels: usinge reminders, optimal compliance with qualityes and benchmarks, such as timely administrationylactic administration of antibiotics [14], as wellw and documentation of allergies into the anes-ecord [15], have been achieved. The concept ofing data collection of clinical parameters, auto-ata analysis, and real-time decision support hasn successfully applied outside of the operatingor example, continuous collection and automatedent of patient characteristics and ventilatorin the ICU have been used to provide immediateo the patients care providers and therebyed the incidence of potentially injurious mech-entilation settings [16]. The portability ofic resources is ever increasing, and its impactoperative and emergency care will continue toUtilizing a smart phone application that providedate resuscitation algorithms in a study of a simu-edical emergency, physicians performed at antly higher level than their peers who had toly on their memory [17]. Mobile devices are alsotransform how we provide postoperative care:
one photographs of surgical wounds taken byat home following ambulatory surgery have beenassess wound complications and to determine ther in-person evaluation by the treating physicianstients who were discharged on postoperativellowing carotid endarterectomy were successfullyd utilizing universal mobile telecommunications(UMTS) video cell phone technology [19].
staydecisthe aof AIprovito imEveralarmsmafirst,outsidatasuppbe aTo sthecommCentensumea
RandimprintoLocaneedpeer-linesthe vare sinstitinitiaPeriopromreseaandIt wiits quits mtinuoultimtheseis a k
Perio
WunquM
Thetransare cight Lippincott Williams & Wilkins. Unauthorized to provide ongoing analysis and meaningfulsupport for the caring providers. The role of
sthesia team is obvious: having been at the helmand its applications for clinical decision support
s a unique opportunity to apply this knowledgeve care hospital-wide and possibly even at home.nesthesiologist is familiar with false and irrelevantWho better than an anesthesiologist could designnvironments that learn from the patient and cased then adjust accordingly? To carry this conceptof the operating room and ICU and to integratelection and analysis systems to provide decisionthroughout all stages of a hospitalization shouldomain of the anesthesia team of the future.port these efforts, professional societies such aserican Society of Anesthesiologists (ASA) arenicating with governmental bodies such as thefor Medicare and Medicaid Services (CMS) toincentives for anesthesia providers that makegful use of EHR.
ized controlled trials have demonstratedd outcomes when protocols are implementedcision-making in many different areas [6,20].linical data collected by automated systems willbe analyzed using established guidelines andiewed literature in order to generate local guide-d protocols of care where applicable. However,me and diversity of data that need to be assessedh that this cannot be accomplished by singleons but rather will require entrepreneuriales to accomplish. Efforts such as the Multicenterrative Outcomes Group (MPOG) lead the way tomulti-institutional collaboration on outcomesthat ultimately aims to advance knowledge
prove patient care in perioperative medicine.ot be sufficient to only initiate such a system;ty and impact will in large parts be determined bytenance. A semi-automated system that is con-ly updated to provide evidence-based care is angoal of outcomes-based medicine. To spearhead
evelopments throughout perioperative medicinetask for future anesthesiologists.
rative epidemiology
cant act on what we dont know; we wont knowwe search; we wont search for what we donttion; we dont question what we dont measurel Harry (Six Sigma authority)
chnological advances described above havemed the way we practice medicine, just as theyging the way we do everything else. One of thed reproduction of this article is prohibited.
-
Copyrig
results of this transformation is the vast amount of datathat are created by new technologies in the process ofdelivering care. EHRs, AIMS, bar code readers, digitizedX-rays, and the like are filling our servers at a pace fasterthan we can keep up with. The information technologycommunity calls this phenomenon Big Data and somehave referred to the current era as the industrial revolu-tion of data [21,22]. A small current example for the needto provide clinical outcome data is the Medicare HospitalInpatient Value-Based Purchasing Program [23]. Hospi-tals will be rewarded based on reported actual qualityperformance measures. Bonus payments may reach up to2% of the entire Medicare reimbursement for a hospitaland are based on clinical process of care measures suchas the administration of prophylactic antibiotics within1 h prior to surgical incision.
Key in this evolution is the field of data management andanalytics, a discipline that is also growing rapidly. Expertsin this field are finding new ways to extract informationfrom large datasets and transform it into knowledge thatcan be used. Comparative effectiveness research is onesuch approach that includes mining of large-scale datasetsto test if newer procedures or treatments compare favor-ably to established ones. Industry has been successful inmany cases, but healthcare, and especially perioperativecare, has not seen transformational results yet.
The role of the anesthesia team is evolving to accompanythis technological transformation. The modern anes-thesia team is one that is becoming progressively moreinvolved with the perioperative care of patients; one thatis deeply interested in the surgical population as a wholeand in optimizing the way care is delivered arounda surgical procedure. Epidemiology may be defined asthe study of the distribution and determinants of diseasefrequency in human populations and the applicationof this study to control health problems [24]. Here,we introduce the term perioperative epidemiology todescribe the activity of studying surgical populations withthe purpose of improving the way we deliver care aroundthe time of surgery.
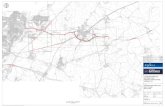
What will the system look like?We propose an iterative process where patient variablesand data from the process of care, together with structuremeasures, are collected and transferred in real-time toa central database (Fig. 1). The database will combineinformation from the hospitals EHR, AIMS, ICU, andPACU systems, laboratory, radiology, and others. Thedata will be filtered and controlled for quality and thendisplayed in real-time through interactive interfacesusing visual analytics principles. Visual analytics is thescience of analytical reasoning facilitated by interactive
690 Technology, education, training, and information systems
Figure 1 The proposed model depicts the flow of data throughout the perioperative period
e
ualt
Patient va theinformatio trointerfaces erglocal revie al gThe local h. Lfinancial aPeerreviewedliterature
NationalGuidelines
Research
Newhypotheses
Datadisplay
Perioperative car
Structure
Process
PatientLocalprotocols &guidelines
Q
riables will be collected together with structure and processmeasures andn from other clinical databases. The data will be filtered and quality-con. The information generated through this system, plus new information emw of the latest peer-reviewed literature will all be combined to generate locdata displayed in real time will also generate new hypotheses for researcnd logistics systems.ht Lippincott Williams & Wilkins. Unauthorizedy filters
Finances
n transferred in real time to a central database that will combinelled and then displayed in real time through interactive visualing from local research, national/international guidelines, and auidelines and protocols and/or assist clinical decision-making.astly, the central data repository could be interconnected withDataanalysis
Logistics
Other clinicaldatabases reproduction of this article is prohibited.
-
Copyr
interfaces. It focuses on the analysis of overwhelmingamounts ofdisparate, conflicting, anddynamic informationand atteand info
Ideally,time anseamlesonly wilof localbut wilexamplesearch qof influewith traControl
The coessentiaplans. Rgreat opstudiesour anespain mIt requiwe dothesioloresearchsuggestanesthecare basprovidequantity
We arechangeRecentgenomiimpact ptions. Tbiologicsignificato betteimprovegenomihave impreoperdecisioncritical
Lastly,connectand maavailabiutilizatiprocesse
institution-specific models derived from AIMS-gene-rated data [27].
mmerheopdeticsofntribe
cluictioutr uhcas temct.s tesw
e opeimtraicingtoionine iosate
nothoinglik
ratio
ictthol fual C
reof pighlspeoutnalLite
A Hcietofeses%
The anesthesia team of the future Bartels et al. 691mpts to facilitate the interaction between humansrmation.
the information will be available to anyone at anyd in any place and will be searchable and allow fors manipulation. This real-time feedback loop notl provide up-to-date information that is reflectivepractices and can inform clinical decision-making,l also be hypothesis generating. An intriguingof such immediate analysis is using Google
ueries related to influenza-like illness: the levelnza activity was predicted 12 weeks earlier thanditional methods from the Centers for Diseaseand Prevention [25].
llection of data to develop guidelines will bel for the development of patient-specific workesearch is integral to this process and represents aportunity for our specialty to engage in clinicalthat reach beyond the traditional four pillars ofthetic domain (anesthesia, critical care medicine,edicine, and critical emergency medicine).res the ability to analyze complex data, whichnot yet teach all our trainees. Training anes-gists as translational investigators by includingas one of the ACGME core competencies as
ed by Reves [26] would not only prepare futuresiologists to lead the quest for improving clinicaled on individual patient data analysis, but alsothem with the skills to enhance the quality andof anesthesia research.
fortunate to practice at a time when medicine willmore rapidly and fundamentally than ever before.developments in regards to the Omics sciencescs, proteomics, and metabolomics will likelyerioperative care and our approach to basic ques-hese include, but are not limited, to the quest foral reasons examiningwhy similar patients can havently different clinical outcomes after surgery, howr tailor perioperative drug therapy, or how toprospective risk assessment by incorporating
c profiling. Ultimately, these developments mayplications ranging from individualized additionalative testing and optimization, to perioperative-making, options of monitoring approaches, andcare resource utilization.
the central data repository could be inter-ed with financial and logistics systems to monitornage elements such as operating room and bedlity, restocking of supplies, and operating roomon and cost. Development of efficient staffings has already been described on the basis of
In sudelivanestits scincluanalycareWe idescr
ConPredtheMajohealttrendotherimpaneedassummoveto thperioand sizedpublutilizdataadditcertafuturany htoler
AckThe aureviewwouldprepa
ConflThe aumentaMedic
RefePapersbeen h of ofAdditioWorld
1 ASSoPrlinight Lippincott Williams & Wilkins. Unauthorizesionng the anesthesia team of the future beyondlined content of this review is challenging.nknowns such as the financial consequences ofre reform and overall healthcare cost, dramaticowards minimal-invasive procedures, as well aserging technologies will likely have a significantTherefore, the anesthesia team of the futureo adapt to the demands of surgical innovation,new supervisory and management roles, andiftly into new opportunities, thus contributing
ptimization of care and outcomes across the entirerative continuum. This requires not only CMEulation-based quality assurance but also special-ining in finance, law, healthcare administration,health, and ultimately, research. Managing,, and analyzing increasing amounts of clinicalenhance perioperative care will continue as anal growth area of our specialty. What remainsis that the perioperative anesthesia team of thes a quintessential component to the success ofpital or operating suite as it provides reliable, welld, modern, and cost-effective care.
wledgementsrs would like to thank Dr Debra A. Schwinn for her efforts inthis manuscript and providing valuable feedback. The authorse to thank Cheryl J. Stetson for assistance in manuscriptn.
s of interestrs have no conflict of interest and were supported by depart-nds of the Department of Anesthesiology, Duke Universityenter.
nces and recommended readingarticular interest, published within the annual period of review, haveighted as:cial intereststanding interestreferences related to this topic can also be found in the Currentrature section in this issue (pp. 711712).
ouse of Delegates. Statement on the anesthesia care team. Americany of Anesthesiology; 2006. http://www.asahq.org/For-Healthcare-sionals//media/For%20Members/documents/Standards%20Guide-20Stmts/Anesthesia%20Care%20Team.ashx [Accessed Sep 2011].ary, technology is rapidly changing the way wecare around the time of surgery. We anticipate thesia team of the future to continue to broadene and to lead a multidisciplinary group that willhealth IT, data management and analytics, visual, and other experts with the goal of enhancing thethe surgical population in the years to come.oduce the term perioperative epidemiology tosuch activity.d reproduction of this article is prohibited.
-
Copyrig
2 Einav S, Donchin Y, Weissman C, Drenger B. Anesthesiologists onambulances: where do we stand? Curr Opin Anaesthesiol 2003; 16:585591.
3 Fischer M, Kamp J, Garcia-Castrillo Riesgo L, et al. Comparing emergencymedical service systems a project of the European Emergency Data (EED)Project. Resuscitation 2011; 82:285293.
4 Soreide E, Kalman S, Aneman A, et al. Shaping the future of Scandinaviananaesthesiology: a position paper by the SSAI. Acta Anaesthesiol Scand2010; 54:10621070.
5 Fleisher LA. Improving perioperative outcomes: my journey into risk, patientpreferences, guidelines, and performance measures: Ninth Honorary FAERResearch Lecture. Anesthesiology 2010; 112:794801.
6 Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professionalpractice, patient outcomes, length of stay and hospital costs. CochraneDatabase Syst Rev 2010; CD006632.
7 Hu Y, Liang D, Li X, et al. The role of interleukin-1 in wound biology. Part I.Murine in silico and in vitro experimental analysis. Anesth Analg 2010;111:15251533.
8 Hu Y, Liang D, Li X, et al. The role of interleukin-1 in wound biology. Part II.In vivo and human translational studies. Anesth Analg 2010; 111:15341542.
9 Spiess BD, Wahr JA, Nussmeier NA. Bring your life into FOCUS! AnesthAnalg 2010; 110:283287.
10 Cumin D, Weller JM, Henderson K, Merry AF. Standards for simulation inanaesthesia: creating confidence in the tools. Br J Anaesth 2010; 105:4551.
11 Weller J, Morris R, Watterson L, et al. Effective management of anaestheticcrises: development and evaluation of a college-accredited simulation-based course for anaesthesia education in Australia and New Zealand.Simul Healthc 2006; 1:209214.
12 Muravchick S. Anesthesia information management systems. Curr OpinAnaesthesiol 2009; 22:764768.
13 Chau A, Ehrenfeld JM. Using real-time clinical decision support to improveperfor2011;
14
Nair Bincludantibio1300.
This articleanalysis to
15 SandbergWS, Sandberg EH, Seim AR, et al.Real-time checking of electronicanesthesia records for documentation errors and automatically text messa-ging clinicians improves quality of documentation. Anesth Analg 2008;106:192201.
16
Herasevich V, Tsapenko M, Kojicic M, et al. Limiting ventilator-induced lunginjury through individual electronic medical record surveillance. Crit Care Med2011; 39:3439.
This study demonstrated the successful implementation of an automated systemintegrating data from multiple sources to provide meaningful decision support toprevent potentially injurious ventilator settings in the ICU.
17 Low D, Clark N, Soar J, et al. A randomised control trial to determine if useof the iResus(c) application on a smart phone improves the performance ofan advanced life support provider in a simulated medical emergency.Anaesthesia 2011; 66:255262.
18 Martinez-Ramos C, Cerdan MT, Lopez RS. Mobile phone-based telemedicinesystem for the home follow-up of patients undergoing ambulatory surgery.Telemed J E Health 2009; 15:531537.
19
Palombo D, Mugnai D, Mambrini S, et al. Role of interactive home teleme-dicine for early and protected discharge 1 day after carotid endarterectomy.Ann Vasc Surg 2009; 23:7680.
This study reports successful utilization of UMTS cell phone technology forpostoperative care at home.
20 Wall RJ, Dittus RS, Ely EW. Protocol-driven care in the intensive care unit:a tool for quality. Crit Care 2001; 5:283285.
21 DoctorowC. Big data: welcome to the petacentre. Nature 2008; 455:1621.
22 Trelles O, Prins P, Snir M, Jansen RC. Big data, but are we ready? Naturereviews. Genetics 2011; 12:224.
23 Services DoHaHSCfMM. Medicare program; hospital inpatient value-basedpurchasing program. Final rule. Fed Regist 2011; 76:2649026547.
24 Aschengrau A, SeageGR, III. The approach and evolution of epidemiology. In:AAaRRS, editor. Essentials of epidemiology in public health. 2nd ed. Sadbury,MA: Jones and Bartlett Publishers; 2008. p. 6.
25
Ginsberg J, Mohebbi MH, Patel RS, et al.Detecting influenza epidemics usingsearch engine query data. Nature 2009; 457:10121014.udy demonstrated the superiority of real-time data analysis (analysis ofsearch query terms) to traditional methods of predicting influenza activity.nce
vese 45
xtereratorm
692 Technology, education, training, and information systems29:5769.
G, Newman SF, Peterson GN, et al. Feedback mechanismsing real-time electronic alerts to achieve near 100% timely prophylactictic administration in surgical cases. Anesth Analg 2010; 111:1293
demonstrated successful, real-time application of automated dataachieve compliance with an established quality of care measure.
This co
26 Reth
27 Deopinfht Lippincott Williams & Wilkins. Unauthorizedpt might be applicable to perioperative settings in the future.
JG. We are what we make: transforming research in anesthesiology:th Rovenstine Lecture. Anesthesiology 2007; 106:826835.
F, Wachtel RE, Epstein RH. Event-based knowledge elicitation ofing room management decision-making using scenarios adapted fromation systems data. BMC Med Inform Decis Mak 2011; 11:2.mance on perioperative quality and process measures. Anesthesiol Clin This stGoogle reproduction of this article is prohibited.
The anesthesia team of thefutureIntroductionClinical practiceTechnologyPerioperative epidemiology
What will the system look like?ConclusionAcknowledgementsConflicts of interest
References and recommended reading


![ip2001-06.ppt [호환 모드] - CHERIC · 2014-02-11 · Comparison of commercial status Status Suppliers Process Markets Fully Commercial ABB/Ebara FB Gasification +Combustion ASR,](https://static.fdocuments.net/doc/165x107/5f28e4fb3c001e42d25403b5/ip2001-06ppt-eeoe-cheric-2014-02-11-comparison-of-commercial-status.jpg)




![14a0054gitecai 14a0054gitecai - FB 002 - FB 002 - Bianca - F.to … · 2014. 3. 10. · 14a0054gitecai-14a0054gitecai-3 - FB 002 - $[LayerName] 14a0054gitecai-14a0054gitecai-4 - FB](https://static.fdocuments.net/doc/165x107/6107fd15e3c88255cd2ce596/14a0054gitecai-14a0054gitecai-fb-002-fb-002-bianca-fto-2014-3-10-14a0054gitecai-14a0054gitecai-3.jpg)